Abstract
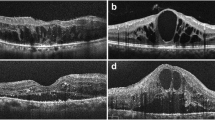
The aim of the current pilot study is to investigate the efficacy of a novel enhanced vitreous imaging (EVI) in primary macular holes (MHs) using a spectral-domain optical coherence tomography (SD-OCT). Thirty-four eyes of 32 consecutive patients with a MH were examined in one time cross-sectional study. The vitreomacular interface was assessed using SD-OCT with conventional and EVI technique. Twenty-three of the 34 eyes did not show a Weiss ring, and in 22 of those, we observed a MH with an open roof or operculum and a detached posterior vitreous cortex with conventional vitreous imaging. Using EVI-OCT, we visualized the reflection of the posterior vitreous with a vitreopapillary attachment. One of the 23 eyes without a Weiss ring had a central round retinal defect without an operculum, and the conventional SD-OCT showed an empty vitreous, suggesting a complete posterior vitreous detachment. However, the EVI-OCT revealed the reflection of the posterior vitreous, and the cortex appeared to still be completely attached. In all the 23 eyes without a Weiss ring, EVI-OCT detected the reflection of the posterior vitreous and vitreopapillary attachment. In all 11 eyes with a Weiss ring (stage 4 hole), EVI-OCT showed an optically empty space in the posterior vitreous cavity without a vitreopapillary attachment. EVI-OCT may be a new reliable method for preoperative evaluations to determine the presence or absence of a complete posterior vitreous detachment in macular diseases with an indistinct Weiss ring.



Similar content being viewed by others
References
Gass JDM (1995) Reappraisal of biomicroscopic classification of stages of development of a macular hole. Am J Ophthalmol 119:752–759
Gaudric A, Haouchine B, Massin P, Paques M, Blain P, Erginay A (1999) Macular hole formation: new data provided by optical coherence tomography. Arch Ophthalmol 117:744–751
Duker JS, Kaiser PK, Binder S et al (2013) The International Vitreomacular Traction Study Group classification of vitreomacular adhesion, traction, and macular hole. Ophthalmology 120:2611–2619
Takahashi A, Yoshida A, Nagaoka T et al (2012) Idiopathic full-thickness macular holes and the vitreomacular interface: a high-resolution spectral-domain optical coherence tomography study. Am J Ophthalmol 154:881–892
Pang CE, Freund KB, Engelbert M (2014) Enhanced vitreous imaging technique with spectral-domain optical coherence tomography for evaluation of posterior vitreous detachment. JAMA Ophthalmol 132:1148–1150
Itakura H, Kishi S (2011) Aging changes of vitreomacular interface. Retina 31:1400–1404
Kishi S, Takahashi H (2000) Three-dimensional observations of developing macular holes. Am J Ophthalmol 130:65–75
Johnson MW, Van Newkirk MR, Meyer KA (2001) Perifoveal vitreous detachment is the primary pathogenic event in idiopathic macular hole formation. Arch Ophthalmol 119:215–222
Takahashi A, Nagaoka T, Ishiko S, Kameyama D, Yoshida A (2010) Foveal anatomic changes in a progressing stage 1 macular hole documented by spectral domain optical coherence tomography. Ophthalmology 117:806–810
Takahashi A, Nagaoka T, Yoshida A (2011) Stage 1-A macular hole: a prospective spectral-domain optical coherence tomography study. Retina 31:127–147
Privat E, Tadayoni R, Gaucher D, Haouchine B, Massin P, Gaudric A (2007) Residual defect in the foveal photoreceptor layer detected by optical coherence tomography in eyes with spontaneously closed macular holes. Am J Ophthalmol 143:814–819
Guillaubey A, Malvitte L, Lafontaine PO et al (2007) Incidence of retinal detachment after macular surgery: a retrospective study of 634 cases. Br J Ophthalmol 91:1327–1330
Akiba J, Ishiko S, Yoshida A (2001) Variations of Weiss’s ring. Retina 21:243–246
Kakehashi A, Inoda S, Shimizu Y, Makino S, Shimizu H (1998) Predictive value of floaters in the diagnosis of posterior vitreous detachment. Am J Ophthalmol 125:113–115
Kakehashi A, Takezawa M, Akiba J (2014) Classification of posterior vitreous detachment. Clin Ophthalmol 8:1–10. doi:10.2147/OPTH.S54021
Ueda-Arakawa N, Ooto S, Ellabban AA et al (2014) Macular choroidal thickness and volume of eyes with reticular pseudodrusen using swept-source optical coherence tomography. Am J Ophthalmol 157:994–1004
Adhi M, Liu JJ, Qavi AH et al (2014) Choroidal analysis in healthy eyes using swept-source optical coherence tomography compared to spectral domain optical coherence tomography. Am J Ophthalmol 157:1272–1281
Liu JJ, Witkin AJ, Adhi M et al (2014) Enhanced vitreous imaging in healthy eyes using swept source optical coherence tomography. PLoS One. doi:10.1371/journal.pone.0102950.2014.07.18
Barteselli G, Bartsch DU, El-Emam S et al (2013) Combined depth imaging technique on spectral-domain optical coherence tomography. Am J Ophthalmol 155:727–732
Ip MS, Baker BJ, Duker JS et al (2002) Anatomical outcomes of surgery for idiopathic macular hole as determined by optical coherence tomography. Arch Ophthalmol 120:29–35
Ullrich S, Haritoglou C, Gass C, Schaumberger M, Ulbig MW, Kampik A (2002) Macular hole size as a prognostic factor in macular hole surgery. Br J Ophthalmol 86:390–393
Ruiz-Moreno JM, Staicu C, Piñero DP, Montero J, Lugo F, Amat P (2008) Optical coherence tomography predictive factors for macular hole surgery outcome. Br J Ophthalmol 92:640–644
Gupta B, Laidlaw DA, Williamson TH, Shah SP, Wong R, Wren S (2009) Predicting visual success in macular hole surgery. Br J Ophthalmol 93:1488–1491
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
Conflict of interest
The authors report no financial support or financial conflict of interest.
Ethical approval
The current study followed the tenets of the Declaration of Helsinki, and the Institutional Review Board of Asahikawa Medical University approved the prospective study design. The nature of the study, participation in its research, and its possible consequences were explained to the patient, after which the patient provided informed consent.
Additional information
The authors have no proprietary or commercial interest in any materials discussed in this article.
Rights and permissions
About this article
Cite this article
Takahashi, A., Nagaoka, T. & Yoshida, A. Enhanced vitreous imaging optical coherence tomography in primary macular holes. Int Ophthalmol 36, 355–363 (2016). https://doi.org/10.1007/s10792-015-0126-y
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s10792-015-0126-y