Abstract
Background
Melatonin is an indole hormone secreted primarily by the pineal gland that showing anti-oxidant, anti-inflammatory and anti-apoptotic capacity. It can play an important role in the pathophysiological mechanisms of various diseases. In this regard, different studies have shown that there is a relationship between Melatonin and Multiple Sclerosis (MS). MS is a chronic immune-mediated disease of the Central Nervous System.
Aim
The objective of this review was to evaluate the mechanisms of action of melatonin on oxidative stress, inflammation and intestinal dysbiosis caused by MS, as well as its interaction with different hormones and factors that can influence the pathophysiology of the disease.
Results
Melatonin causes a significant increase in the levels of catalase, superoxide dismutase, glutathione peroxidase, glutathione and can counteract and inhibit the effects of the NLRP3 inflammasome, which would also be beneficial during SARS-CoV-2 infection. In addition, melatonin increases antimicrobial peptides, especially Reg3β, which could be useful in controlling the microbiota.
Conclusion
Melatonin could exert a beneficial effect in people suffering from MS, running as a promising candidate for the treatment of this disease. However, more research in human is needed to help understand the possible interaction between melatonin and certain sex hormones, such as estrogens, to know the potential therapeutic efficacy in both men and women.
Similar content being viewed by others
Avoid common mistakes on your manuscript.
Introduction
Melatonin is an important regulator of physiological processes and a guardian of body homeostasis (Chitimus et al. 2020). In addition to its chronobiotic properties (Cardinali 2019), melatonin has shown to have antioxidant, anti-inflammatory and immunomodulatory and anti-apoptotic capacity, as well as a neuroprotective effect (Reiter et al. 2000; Esposito and Cuzzocrea 2010; Rosales-Corral et al. 2012; Wang et al. 2013; Bahamonde et al. 2014). Due to the multiple locations of formation and expression of melatonin receptors, it is called pleiotropic factor (Claustrat and Leston 2015; Skarlis and Anagnostouli 2020). Due to this characteristic, this hormone is gaining interest (Carrascal et al. 2018) as a possible therapy in autoimmune and inflammatory processes (Carrascal et al. 2018; Zhao et al. 2019) This is also because dysregulation of melatonin secretion has been associated with the pathogenesis of several autoimmune disorders, such as Multiple Sclerosis (MS) (Farez et al. 2016; Skarlis and Anagnostouli 2020).
MS is a chronic immune-mediated disease of the central nervous system (SCN), characterized by destruction of myelin by autoreactive T cells (Farez et al. 2015; Long et al. 2018) and axonal degeneration (Faissner et al. 2019). It presents a wide range of signs and symptoms that alter physical, cognitive, emotional and social functioning (Harbo et al. 2013; Sakkas et al. 2019). Melatonin levels have been linked to the severity and relapse of MS (Ghareghani et al. 2018). It has been confirmed that melatonin can exert beneficial effects on some of the symptoms that MS produces, improving the quality of life of patients. In fact, a clinical trial is currently being carried out on the treatment with melatonin in patients with Relapsing–Remitting Multiple Sclerosis (RRMS), with the aim of evaluating whether supplementation with 3 mg of this hormone affects the level of 6-sulfatexymelatonin (6-SMT) in urine, as well as the effect on different aspects, such as quality of life and number of relapses in patients (“Melatonin in Patients With Multiple Sclerosis (MS).—Full Text View—ClinicalTrials.gov,” 2018). This and other clinical trials could clarify whether melatonin may represent an option in the design of therapies for MS (Skarlis and Anagnostouli 2020), so it is also very necessary to know how melatonin acts in the different pathophysiological processes that occur in the MS course. Therefore, the objective of this review will be to evaluate the mechanisms of action of melatonin on oxidative stress, inflammation and intestinal dysbiosis caused by MS, as well as its interaction with different hormones and factors that can influence the pathophysiology of the disease.
Methodology
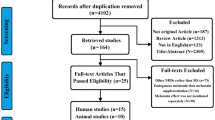
A literature search was performed in the PubMed and Scopus databases, without language limitations. The search was limited to articles published between 2010 and 2021. The keywords “melatonin”, “multiple sclerosis” and “demyelinating disease” were used. These terms were searched for alone or in combination, for example by combining “melatonin AND multiple sclerosis”. In addition, the references of relevant studies, reviews and editorials were also searched from the articles read. Specific references were also sought to write sections that were added throughout the writing of the manuscript, using keywords, such as “vitamin D”, “sex hormones”, “neurotrophic factors”, and “Covid-19”. A total of 624 articles were collected, including original articles, review articles and abstracts. Articles dealing with the effect of melatonin on clinical symptoms of MS were excluded; therefore, 192 articles were included. After reading these manuscripts, 40 more articles were searched, so that finally 232 scientific productions were included in the review.
Melatonin: synthesis, secretion, receptors and function
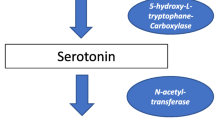
Melatonin (N-acetyl-5-methoxytryptamine) is an indole hormone synthesized from tryptophan and mainly secreted by the pineal gland in a circadian rhythm (Escribano et al. 2014; Carrascal et al. 2018), although it can be secreted by other extrapineal sources such as cells from the immune system, the brain, the skin and the gastrointestinal tract (Carrascal et al. 2018). Its synthesis and secretion at the pineal gland level are controlled by the suprachiasmatic nucleus in the hypothalamus, this being induced by darkness and inhibited in the light (Skarlis and Anagnostouli 2020). In adults, the nocturnal serum level of melatonin is of 25–85 pg/ml, reaching its peak between 4:00 and 6:00 h and diminishing between 7:00 and 9:00 h (Akpinar et al. 2008). Likewise, melatonin presents seasonal fluctuations (Mocayar-Marón et al. 2020), reaching its maximum concentration in the autumn–winter months (Farez et al. 2015).
The effects of melatonin are exerted through dependent and independent receptor pathways (Kern et al. 2019). Melatonin-binding sites have been found in the membranes of several tissues known as high affinity G-protein coupled receptors (Zhao et al. 2019; Kern et al. 2019). Those receptors are MT1 and MT2, which are expressed, among other places, in several areas of the CNS (Soto-Brambila et al. 2017). MT1, is codified by the gene MTNR1A in chromosome 4q35.1 (Li et al. 2013) and is mainly found in the hippocampus, retina, thalamus, vestibular nuclei, brain and cerebellum; and MT2 is codified by the gene MTNR1B in chromosome 11q21-q22 (Li et al. 2013) and is located in the hippocampus, brain, cerebellum, reticular thalamus, substantia nigra, supraoptic nucleus and red nucleus (Musshoff et al. 2002; Comai and Gobbi 2014; Beriwal et al. 2019). Other nuclear melatonin-binding sites have also been described, such as orphan receptors related to retinoic acid (ROR) (Soto-Brambila et al. 2017; Kern et al. 2019).
The chief function of melatonin is to transmit information on the daily light and darkness cycle (Claustrat et al. 2005) and it plays a key role in the regulation of the sleep-awakeness cycle, puberty development, seasonal adaptation and memory formation (Giannoulia-Karantana et al. 2007; Skarlis and Anagnostouli 2020). Furthermore, melatonin is known to be a multifunctional molecule (Onaolapo et al. 2019), and has been seen to have an anti-oxidant, anti-inflammatory (Escribano et al. 2014) and anti-apoptotic capacity, as well as acting in immune responses and mitochondrial homeostasis (Carrascal et al. 2018) contributing to the multiple cell differentiation and survival in the brain (Onaolapo et al. 2019).
These properties indicate that melatonin can have an important incidence in the physiopathological mechanisms of diverse diseases (Gunata et al. 2020) (The main effects of melatonin in humans and in animal models are summarized in Tables 1, 2). It has been proved that melatonin levels are correlated with neuroimmune diseases (Ghareghani et al. 2018), and that a low level of this hormone is associated with diseases, such as Alzheimer, Parkinson’s, Lateral Amyotrophic Sclerosis LAS), and Multiple Sclerosis (MS) (Tan and Hardeland 2020). Research on MS is especially important, as many of the factors behind its pathogenesis are still unknown and there are no medications to cure this disease. (Miller et al. 2013). MS is also the most common cause of non-traumatic disability in young adults (Chen et al. 2020), between the ages of 20–30 (Gunata et al. 2020).
Multiple sclerosis
Symptoms, types, causative agents, and prevalence
MS is a disease that causes motor, sensorial and cognitive deficits (Soto-Brambila et al. 2017). Patients with this disease have a wide variety of symptoms (Huang et al. 2017), although the most common ones are: vision deficiency, extreme fatigue, spasms, (Soto-Brambila et al. 2017), bladder dysfunction, paresthesia, dysesthesia, diplopia, ataxia, vertigo, trigeminal neuralgia and optic neuritis (Hauser and Goodwin 2008; Goldenberg 2012; Escribano et al. 2014). It is also associated with comorbidities, such as anxiety, depression and sleep alterations (Skarlis and Anagnostouli 2020). The physiopathological characteristics of MS are: inflammation that occurs in white matter areas of the CNS (Sánchez-López et al. 2018), demyelination and glial healing (Akpinar et al. 2008), that occurs focally or diffusely all over the grey and white brain matter and the spinal cord (Lassmann et al. 2007, 2012; Escribano et al. 2014). Demyelination is propagated through the CNS and may vary in distribution, pattern and size (Soto-Brambila et al. 2017). These lesions are produced by an immuno-mediated dysregulation of the blood brain barrier (BBB), facilitating the entry of inflammatory cells activated in the brain and spine (Yeganeh-Salehpour et al. 2019).
There are four types of MS: progressive relapsing, primary-progressive, relapsing–remitting (RRMS), and secondary-progressive (SPMS) (Compston and Coles 2002, 2008; Bahamonde et al. 2014), with RRMS, being the main form of the disease (Adamczyk-Sowa et al. 2016b) affecting 85% of patients (Michaličková et al. 2020b). In the four types of MS there is neurodegeneration and inflammation, but the RRMS is characterized by the appearance of symptoms, followed by a period of clinical remission (Adamczyk-Sowa et al. 2016b).
MS affects 2,5 million people world-wide (Yeganeh-Salehpour et al. 2019) with a higher proportion of women suffering from it than men (Zeydan et al. 2020). Women have a more robust immune system than that of men, hence the female prevalence of MS (Avila et al. 2018) suggests that the sex hormones play a part in the pathogenesis of this disease (Gold and Voskuhl 2009). In addition, MS appears earlier in women than in men, although the male sex gives a worse clinical result and a greater accumulation of disability (Ribbons et al. 2015; Dupuis et al. 2021).
A higher prevalence is also observed in countries with high altitudes, where the sunlight is limited and its inhabitants present vitamin D deficiencies (Ghareghani et al. 2018), this being a risk factor for the development and progression of MS (Ascherio 2013). Thus, environmental factors seem to have some weight in the geographic prevalence patterns of this disease (Sakkas et al. 2019).
In addition to the latitude, another aspect increasing the risk of suffering from MS is that of viral infections. Infection by the Epstein–Barr virus is one of the most important risk factors for this disease (Ascherio 2013), but also infection by the human 6 Herpes virus (Long et al. 2018; Yosefifard et al. 2019) and by certain members of the coronavirus family (Matías-Guiu et al. 2020).
Genetics is the main factor related to the development of MS, with the genetic locus of the major histocompatibility complex being in chromosome 6, a good candidate for determining susceptibility to MS (Yosefifard et al. 2019). The allele with the highest risk for developing MS is HLA-DRB1*15:01, which is associated with a 6 times greater danger of contracting the disease in homozygote carriers (Patsopoulos et al. 2013).
In MS pathology, neurotrophins such as nerve growth factor (NGF) and brain-derived neurotrophic factor (BDNF) also play an important role (Langhnoja et al. 2021). Despite their cellular and molecular functions still not being well-known (Langhnoja et al. 2021). These neurotrophins have a fundamental involvement in neuronal repair and plasticity (Gold et al. 2003), promoting the proliferation of neural stem cells and their differentiation in the oligodendroglial lineage (Langhnoja et al. 2021). All this suggests the neuroprotective capacity of these proteins in MS patients (Gold et al. 2003).
Cellular and molecular mechanisms involved in multiple sclerosis
In MS, the definitive presence of oxidative stress has been demonstrated (Holton and Kirkland 2020). It acts as a mediator of demyelination, axonal damage and neurodegeneration (Ramirez-Ramirez et al. 2013; Sánchez-López et al. 2018). MS patients present high levels of oxidative stress biomarkers, as well as an overall antioxidant deficiency (Bahamonde et al. 2014; Escribano et al. 2017). In addition, in the study made by Conde et al., 2019, for the first time, the presence of intense oxidative stress in non-nervous organs in the animal MS model, experimental autoimmune encephalomyelitis (EAE), was verified, which suggests that something similar may occur in MS patients (Conde et al. 2019). During the course of the disease, the infiltration of autoreactive effector T cells Th1 and Th17 into the CNS, causes an increase in pro-inflammatory cytokines (Interferon-γ (IFN-γ), the tumoral necrosis factor (TNF), Interleukin-17 (IL-17) (van den Hoogen et al. 2017) and Interleukin-22 (IL-22)), which attack the myelin sheath (Michaličková et al. 2020b). After the inflammatory reaction, the permeability of the BBB is increased by the action of the matrix metalloproteinase-9 (MMP-9), and other immune cells such as B lymphocytes and monocytes are recruited (Adamczyk-Sowa et al. 2016a; Michaličková et al. 2020a) (Fig. 1).
Cellular and molecular mechanisms involved in Multiple Sclerosis CNS central nervous system, VCAM-1 vascular cell adhesion molecule 1, Th1,Th17 cells T helper 1, T helper 17, IL-17 Interleukin 17, IL-22 interleukin 22, IL-1α Interleukin 1α, TNF-α tumor necrosis factor-α, IFN-γ Interferon-γ, LPS lipopolysaccharide, LBP LPS-binding protein, CP carbonylated proteins, LPO lipid peroxidation products, NO nitric oxide, MDA malondialdehyde, tG total glutathione, GSSG oxidized glutathione, GPx glutathione peroxidase, GSH reduced glutathione, SIRT3 sirtuin 3, NF-κB factor nuclear kappa B, Nrf2 Factor 2 related to nuclear erythroid 2, ROS reactive oxygen species, iNOS nitric oxide synthase
An increase in pro-inflammatory cytokines induces an excessive production of reactive oxygen species (ROS) and reactive nitrogen species (RNS) (Soto-Brambila et al. 2017; Conde et al. 2019). The latter are extremely unstable and have a great oxidative capacity (Long et al. 2018). ROS activates the nuclear kappa B factor (NF-κB) (Valacchi et al. 2018), which is activated in multiple CNS cells, including the T cells, microglia, macrophages, astrocytes, oligodendrocytes and neurons, and regulates positively the expression of factors implicated in the pathogenesis of MS, including TNF-α, nitric oxide synthase (iNOS), IL-1α and molecule 1 of vascular adhesion (VCAM-1) and several growth factors (Michaličková et al. 2020a). When NF-κB is activated, it causes an increase in inflammation and demyelination and triggers the onset of the disease (Yue et al. 2018). Recently, the implication of inflammasomes in the pathogeneses of neurodegenerative diseases has begun to be studied. It was observed that inflammasome NLRP3, plays a vital role in MS (Feng et al. 2021). The activation of NF-κB, together with that of pro-caspase 1 are the two signals required to activate this inflammasome (Michaličková et al. 2020b). When NLRP3 is active, it causes a proteolytic activation of caspase-1, enabling the secretion of the pro-inflammatory cytokines IL-1β and IL-18 (Lahooti et al. 2021) and also regulates the response of cells Th1 and Th17 (Feng et al. 2021) (Fig. 1).
Another of the effects provoking the persistent activation of NF-κB is the dysregulation of transcription factor Nrf2 (Nuclear factor-erythroid 2 related factor 2) (Fernández-Ortiz et al. 2020), the latter being the principal regulator of antioxidant protection mechanisms (Shih and Yen 2006) and whose transactivation is induced in presence of ROS and RNS (Zhang et al. 2013; Escribano et al. 2014).
Due to oxidative stress, another crucial phenomenon occurring in MS is the alteration in the homeostasis of glutathione (Michaličková et al. 2020b), which is the principal brain antioxidant and has a key role in the detoxification of reactive species (Carvalho et al. 2014) (Fig. 1).
Relationship of melatonin with multiple sclerosis
The different studies carried out have shown that there is a relationship between melatonin and MS. MS patients showed a decrease in both nocturnal melatonin, which has been correlated with the severity of the disease, and with symptoms, such as fatigue, insomnia or depression. (Álvarez-Sánchez et al. 2017), and in their principal metabolite in urine, 6-SMT (Álvarez-Sánchez et al. 2015).
Melatonin levels, which peak in fall–winter, show an inverse correlation with clinical disease activity in MS patients, since its symptoms are more likely to occur in spring/summer than in fall/winter (Farez et al. 2015). This seasonal pattern that led Farez et al. (2015) to the study of the relationship between multiple sclerosis and melatonin. Quintana, associate professor in the Ann Romney Center for Neurologic Diseases at Brigham and Women’s Hospital (BWH), with colleagues at the Center for Research on Neuroimmunological Diseases (CIEN) at the Raul Carrea Institute for Neurological Research (FLENI) in Argentina, found that during the fall and winter, a group of 139 relapsing remitting MS patients, experienced a significant improvement in symptoms. They explored a variety of environmental factors (vitamin D levels, UV incidence and upper respiratory tract infections), but the factor that was consistently associated with severity of MS symptoms was melatonin (Farez et al. 2015). A thorough study in mouse and human cells led them to the conclusion that melatonin affects the roles of two kinds of cells that are important in MS disease progression: pathogenic T cells that directly attack and destroy tissue and regulatory T cells, which are supposed to keep pathogenic T cells in check. This higher incidence of MS in spring/summer has been verified in different studies such as in the meta-analysis carried out by Jin et al. (2000) who report that the beginnings of monosymptomatic optic neuritis, the first clinical manifestation of MS in 20–30% of cases and in its exacerbations, present a similar pattern with higher frequencies in spring and lower in winter (Jin et al. 2000). Similarly, Spelman et al. (2014), determine that relapse onset in MS followed an annual cyclical sinusoidal pattern with peaks in early spring (Spelman et al. 2014). Among the reasons for which it is believed that MS patients exhibit a lower level of melatonin is that it is due to the deposition of calcium in the pineal gland (Akpinar et al. 2008; Tan et al. 2018; Yosefi-Fard et al. 2020) or to hypothalamic dysfunction in the regulation of the oscillatory secretion of the melatonin (Akpinar et al. 2008).
It has been established that one of the most successful clinical treatments existing currently for treating MS is Natalizumab that triggers an increase in the serum concentration of melatonin (Bahamonde et al. 2014) so that part of the effects exerted by Natalizumab in these patients could be explained by the stabilization of melatonin levels (Bahamonde et al. 2014; Zhao et al. 2019). Melatonin could have a prophylactic and therapeutic effect on this disease (Gunata et al. 2020), and it has been evidenced that supplementation with this hormone contributes to alleviating cognitive and motor imbalances (Chen et al. 2020). In addition, melatonin improves oligodendroglial differentiation and maturation and myelin repair. (Ghareghani et al. 2017b). Melatonin therapy modulates brain metabolism and improves remyelination. This is associated with an increase in pyruvate dehydrogenase kinase-4 (PDK-4), an enzyme involved in the synthesis of fatty acids during remyelination. (Ghareghani et al. 2019).
However, a study by Constantinescu et al., 1997 concluded that melatonin could exacerbate autoimmunity, suggesting that inhibition of melatonin could prevent demyelination (Constantinescu et al. 1997). Similarly, Ghareghani et al., 2017a, b, found a negative impact of melatonin on the recovery of EAE in young rats, by improving IFN-γ, the ratio of Th1/Th2 cells and astrocyte activation, which can delay the remyelination process, so they conclude that age plays a substantial role in melatonin therapy (Ghareghani et al. 2017a).
Discussion of melatonin use in clinical studies
The clinical studies included in this review use very different doses of melatonin as treatment for RRMS patients, mostly SPMS or PPMS patients. These doses range from 3 to 25 mg, all administered once a day. In four of the articles, this dose is administered orally (Adamczyk-Sowa et al. 2016a; Sánchez-López et al. 2018; Yosefifard et al. 2019; Yosefi-Fard et al. 2020), while in two of them, the route of melatonin administration is not specified (Miller et al. 2013; Roostaei et al. 2021). Similarly, the duration of the treatment varies considerably from article to article, the shortest duration being 1 month (Miller et al. 2013) and the longest 1 year (Roostaei et al. 2015). Regarding oxidative stress, there is a reduction in its biomarkers in all the articles that study this effect, regardless of the dose, regimen or route of administration of melatonin. Obtain a decrease in malondialdehyde (MDA) (Miller et al. 2013), lipid hydroperoxides (Adamczyk-Sowa et al. 2016a) and NO (Sánchez-López et al. 2018). Likewise, Miller et al. 2013 show an increase in the enzymes SOD and GPx. Regarding inflammation, different results appear in the studies that evaluate the effect of melatonin on the levels of proinflammatory cytokines. Sánchez-López et al. 2018 obtained a reduction in the levels of TNF-α, IL-1β and IL-6, using a dose of 25 mg/day for 6 months. However, Yosefifard et al. 2019 do not obtain changes in the levels of TNF-α after a treatment of 3 mg/day for 24 weeks, although they do observe a reduction in the levels of IL-1β (Yosefifard et al. 2019). These results could indeed indicate a different dose-dependent effect on TNF-α levels, since the route of administration is the same, the duration of treatment is similar and the Expanded Disability Status Scale (EDSS) of patients was 0–0.5 to 5 in both studies. Apparently, a higher dose of melatonin favors the reduction of TNF-α levels in patients with RRMS, while the levels of other proinflammatory cytokines, such as IL-1β, decrease regardless of dose. On the other hand, the administration of 3 mg/day of melatonin for 1 year in the study by Roostaei et al. 2015, did not produce effects on measures of clinical and functional disability and on the development of brain lesions. Based on these results, it might be thought that, to reduce the clinical activity of MS, it is necessary to use a higher dose of melatonin (Table 1).
Immunomodulator and anti-inflammatory effect of melatonin in multiple sclerosis. Mechanism of action
The immunomodulatory and anti-inflammatory effects of melatonin allow it to inhibit the expression and activation of NF-κB, preventing its translocation to the nucleus and its binding to DNA (Maldonado et al. 2010; Escribano et al. 2014), thus reducing the synthesis of inflammatory mediators and, ultimately, suppressing inflammation (Ramos González et al. 2018; Sánchez-López et al. 2018; Zhao et al. 2019; Luo et al. 2020).
The inflammasome NLRP3 has been identified as being a new molecular target for melatonin (García et al. 2015), and it is capable of counteracting and inhibiting the effects of NLRP3 (Michaličková et al. 2020b; Luo et al. 2020; Fernández-Ortiz et al. 2020).
In the course of MS, an increase is also produced in adhesion molecules (intracellular adhesion molecules (ICAM-1) and VCAM-1), which promote the adherence of the leukocytes to the endothelial cells (Maldonado et al. 2010; Escribano et al. 2014). Melatonin deficit has been associated with an increase in the levels of these molecules, as well as of MMP-9 (Wang 2009; Lin et al. 2013; Bahamonde et al. 2014). However, the administration of melatonin in EAE animals resulted in a reduction in ICAM-1 levels (Kang et al. 2001; Bahamonde et al. 2014). A recent study has shown that melatonin can reduce ICAM-1 levels through the RORα/miR-223/STAT-3 signaling pathway. This pathway is involved in the regulation of ICAM-1. Melatonin could induce the expression of miR-223 through its receptor RORα. Upregulation of miR-223 causes downregulation of STAT-3 expression, triggering suppression of ICAM-1 expression (Yi and Yang 2021). This causes a decrease in the migration of transendothelial cells (Maldonado et al. 2010; Escribano et al. 2014).
The effect of melatonin on T cells
In MS, it is widely known that there is an imbalance in T cell responses, which is fundamental for the development and progression of the disease (Long et al. 2018). Melatonin affects the differentiation and function of effector and regulator T cells in vivo and in vitro (Farez et al. 2015) in MS, and is capable of reducing the number of inflammatory infiltrates into the CNS in the EAE model (Long et al. 2018).
Álvarez-Sánchez et al. 2015 report that melatonin reduces the peripheric and central responses of Th1 and Th17, and improves the regulatory T cell Tr1’s levels, thus increasing the IL-10 in the EAE model (Álvarez-Sánchez et al. 2015). However, in a study by those same authors, carried out in RRMS patients, melatonin administration diminished the Th1 and Th22 responses, but did not affect the subgroups Th17 and Tr1 (Álvarez-Sánchez et al. 2017). Chang et al., 2020 in their study on myasthenia gravis, were also able to verify that melatonin produced a significant decrease in the response of Th1 and Th17 cells (Chang et al. 2020). The work done by Farez et al., 2015 demonstrates that melatonin promotes the differentiation of Tr1 cells by means of the activation of the Erk 1/2 pathway (extracellular signal-regulated kinase 1/2), and that the ROR-α receptor acts as a mediator of the effects of melatonin on these cells. In the case of Th17 cells, melatonin blocks their differentiation through the expression of the IL-3-regulated nuclear transcription factor (NFIL3) (Yu et al. 2013; Farez et al. 2015), which suppresses the expression of ROR-γt (Yu et al. 2013).
The effect of melatonin on proinflammatory cytokines
In MS lesions, diverse types of pro-inflammatory cytokines are present, such as: IFN-γ and TNF, produced by cells Th1; IL-17, produced by cells Th17; and IL-22, produced by cells Th22 (Hofman et al. 1989; Lock et al. 2002; Kebir et al. 2007; Álvarez-Sánchez et al. 2017). TNF is one of the most important inflammatory factors, exerting a vital role in damage to oligodendrocytes and the myelin (Ontaneda et al. 2012; Mahad et al. 2015; Yosefifard et al. 2019). Moreover, the TNF level in serum and in cerebrospinal fluid has been related to the advance of the disease (Sharief and Hentges 1991; Álvarez-Sánchez et al. 2017; Yosefifard et al. 2019). IL-17 and IL-22, are involved in the alteration in the BBB and the recruitment of T cells CD4 + and neutrophils to the CNS (Kebir et al. 2007; Álvarez-Sánchez et al. 2015) and the IFN-γ is responsible for the recruitment of macrophages (Kroenke et al. 2008; Álvarez-Sánchez et al. 2015). IL-1, one of the most important pro-inflammatory cytokines is also present in MS; it is expressed in the peripheric tissue of monocytes and macrophages, increasing significantly after damage (Mendiola and Cardona 2018; Yosefifard et al. 2019).
Various studies confirm the effect of melatonin on pro-inflammatory cytokines. It has been seen that it is capable of reducing their production, especially of TNF, IL-1β e IFN-γ (Álvarez-Sánchez et al. 2015, 2017; Sánchez-López et al. 2018; Anderson et al. 2019; Yosefifard et al. 2019) and of increasing the levels of anti-inflammatory cytokines like that of IL-10, by means of an MT1-dependent mechanism (Xu et al. 2018) and IL-4 (Carrillo-Vico et al. 2005; Álvarez-Sánchez et al. 2015; Ghareghani et al. 2019). It also offers a more protective microenvironment for cytokines (Álvarez-Sánchez et al. 2017). In addition, Yosefi-Fard et al. 2020 show in their study that melatonin levels are associated with an increase in IFN-β, which is beneficial against relapses in MS (Yosefi-Fard et al. 2020).
The results of the study made by Xu et al. 2018 find that melatonin inhibits proinflammatory cytokine production seeing that it decreases TNF-α production and TLR9-mediated IL-6, (Toll type Receptor 9) in mouse serum, it regulates the TLR3 and TLR4 signals (Toll type Receptor 3 and Toll type Receptor 4) in macrophages, and causes a significant decline in the production of IL-12, after macrophage activation (Xu et al. 2018).
Effect of melatonin on oxidative stress of multiple sclerosis. Mechanism of action
An increase in proinflammatory cytokines after lymphocyte and macrophage infiltration into the CNS augments the ROS generation, which favors inflammation still more and produces oxidative stress. The latter is a condition under which the organism’s antioxidant defenses are insufficient due to the excessive release of oxidants (Padureanu et al. 2019) Some of its main consequences are: the large increase in lipid peroxidation products (LPO); protein carbonylation or carbonylated proteins (CP); oxidative damage to the nuclear and mitochondrial DNA, as well as disorders related to its own replication mechanisms and damage to cell tissues and walls (Senthil Kumaran et al. 2008; Şimşek et al. 2016; Maes et al. 2019; Holton and Kirkland 2020; Morris et al. 2021).
Reactive species are produced naturally by aerobic metabolism and processes involved in the response to pathogens (Michaličková et al. 2020b). ROS presents unpaired electrons, which makes it more reactive and with a capacity for capturing electrons from other molecules (Holton and Kirkland 2020). Besides, it can react with some unsaturated fatty acids present in the cell membranes, which activates the lipid peroxidation process, triggering the modification of proteins and changes in the membrane gradient, resulting in a loss of integrity and irreversible damage (Senthil Kumaran et al. 2008).
Due to the characteristic antioxidant effect of melatonin, it could be of great assistance in combatting the oxidative stress produced in MS, reducing macromolecular damage in all the organs (Maldonado et al. 2010; Escribano et al. 2014), and reducing the principal oxidative stress biomarkers (Carbonylated proteins (CP), lipid peroxidation products (LPO), Nitric oxide (NO) and MDA (Túnez et al. 2004; Miller et al. 2013; Bahamonde et al. 2014; Adamczyk-Sowa et al. 2017; Soto-Brambila et al. 2017; Yeganeh-Salehpour et al. 2019; AboTaleb and Alghamdi 2020; Alghamdi and AboTaleb 2020) and the oxidative damage to nuclear DNA, both in vivo and in vitro (Túnez et al. 2004). The antioxidant capacity of melatonin in the EAE model has recently been demonstrated in an article published by our research group. In this manuscript, we demonstrate that melatonin has the capacity to restore the body’s antioxidant defenses while decreasing the main oxidative stress biomarkers (LPO, CP and NOx,) which are increased in the EAE model (Escribano et al. 2022).
Glutathione redox cycle
CNS is especially susceptible to ROS damage, due to the brain’s high oxygen demands, the low concentration of antioxidants, and the high concentration of polyunsaturated fatty acids (Gonsette 2008; Miller et al. 2011, 2013). The oxidative damage that occurs in neurodegenerative diseases is an effect mainly due to a severe alteration in the glutathione redox cycle (Sandri et al. 1990; Di Monte et al. 1992; Martín et al. 2000a). In the study carried out by Tasset et al. 2012, they reported that MS patients have an oxidation state and a global antioxidant deficiency (Tasset et al. 2012).
Different studies have shown that melatonin improves antioxidant defense systems by stimulating the activity of antioxidant enzymes, such as superoxide dismutase (SOD), catalase (CAT) and the glutathione redox cycle (Martín et al. 2000a; Miller et al. 2013; Bahamonde et al. 2014; Soto-Brambila et al. 2017; Yeganeh-Salehpour et al. 2019; Zhao et al. 2019; AboTaleb and Alghamdi 2020).
Martín et al., 2000a, b, examined the influence of melatonin on the content of glutathione (GSH) and the activity of the enzymes glutathione peroxidase (GPx) and glutathione reductase (GRd), in mitochondria isolated from the liver and brain of rats treated with t-butyl hydroperoxide. The results of this study suggest that melatonin maintains GSH homeostasis and prevents oxidative damage in mitochondria by counteracting changes in GSH, GPx, and GRd (Martín et al. 2000a). Similar results show Miller et al. 2013, who obtain that melatonin caused a statistically significant increase in SOD and GPx and a decrease in MDA in the erythrocytes of SPMS patients (Miller et al. 2013). Similarly, the results of the study carried out by Bahamonde et al. 2014, show that the elevation of serum melatonin is associated with a reduction in oxidative stress markers, characterized by an increase in GSH levels and a decrease in 8-hydroxy-2’deoxyguanosine (8-OHdG) (Bahamonde et al. 2014). In the recent study published by (AboTaleb and Alghamdi 2020), reported that melatonin exerted beneficial effects through its role as an antioxidant agent, evidenced by the significant increase in the levels of CAT, SOD, GPx and GSH, as well as by the reduction of MDA, during the demyelination stage in mice with MS induced by cuprizone (AboTaleb and Alghamdi 2020). In accordance with what has been described, data from our group, indicate that melatonin increases GSH, GPx and the GSH/GSSG ratio in blood and in all the organs studied (brain, spinal cord, heart, liver, kidneys, small and large intestine) and also reduces the levels of GSSG, in mice with induced EAE (Escribano et al. 2022).
Melatonin and the Nrf2 signaling pathway
Nrf2 is the principal regulator of antioxidant protection mechanisms (Shih 2006). In the absence of oxidative stress, the transcription factor Nrf2, and Keap1 (Protein 1 associated with ECH (epichlorohydrin)) are bound in the cytoplasm (Fukutomi et al. 2014; Long et al. 2018). In the presence of oxidative stress, the Nrf2-Keap 1 bond is broken (Marcus and Andrabi 2018) and Nrf2 does not undergo its normal cytoplasmic degradation (Morris et al. 2021). Instead, it travels to the nucleus, where it is heterodimerized (Katsuoka and Yamamoto 2016) and binds to ARE (antioxidant response element) in the target gene-promoting region. Subsequently, the transcription of antioxidant (Morris et al. 2021), anti-inflammatory and cytoprotective genes begins (Kahroba et al. 2021). The activation of this signaling pathway is vital to cell defense mechanisms (Shah et al. 2017), since it maintains redox homeostasis in the cells (Kahroba et al. 2021).
During the course of MS, the Nrf-2/ARE pathway is activated, but it has been suggested that this activation, and that of other endogenous antioxidant defense mechanisms, might not be sufficient to prevent neuronal degeneration and lesion propagation (Licht-Mayer et al. 2015). Certain studies have reported a decrease in Nrf2 in samples of grey matter from MS patients, correlating this with a reduced expression of genes intervening in oxidative phosphorylation and an increase in oxidative damage (Pandit et al. 2009; Michaličková et al. 2020b). In addition, Johnson et al. 2009, confirmed the existence of Nrf2 deficiency in the EAE model (Johnson et al. 2009). That is why it is important to find drugs that upregulate this antioxidant mechanism as this would attenuate MS pathogenesis (Johnson et al. 2009).
In the study made by Fernández-Ortiz et al. 2020, which investigated the role of the inflammasome NLRP3 in cardiac aging and the actions and targets of melatonin in the aged myocardium of mice, they were able to establish that a melatonin supplementation restored the Nrf2-dependent antioxidant capacity, which had been dysregulated by the activation of NF-κB (Fernández-Ortiz et al. 2020). Different works studying the role of melatonin in oxidative stress have concluded that it is able to improve the antioxidant activity of Nrf2/ARE (Shah et al. 2017; Long et al. 2018; Albazal et al. 2021), reducing oxidative stress (Das et al. 2020). Excessive and prolonged oxidative damage and failure of DNA repair can induce apoptosis (Dizdaroglu 2005; Trachootham et al. 2008). However, if the ability to remove ROS is restored, redox homeostasis would be restored without the damage becoming irreversible, since, after exposure to excess ROS, cell survival depends on the strength of antioxidant defense barriers (Diez et al. 2021). In this sense, some studies have investigated the effect of Nrf2 activation, which promotes cell survival under oxidative stress (Trachootham et al. 2008). An example of this is the study carried out by Kubo et al. 2017, in which they show that an Nrf2 activator, sulforaphane, in the presence of oxidative stress increased the expression of antioxidant enzymes in a dose-dependent manner and stopped the deregulation of Nrf2, restoring the transactivation potential of this factor (Kubo et al. 2017). Melatonin exerts a similar effect on Nrf2, facilitating its nuclear translocation, in the presence of oxidative stress (Das et al. 2020). Likewise, Park et al., 2020 demonstrated that the addition of substance-P (SP) increased cell viability, supporting the possibility that SP can recover cell activity after oxidative stress-induced dysfunction (Park et al. 2020). Based on this, it could be said that there are certain substances, including melatonin, that could recover the cellular redox potential, altered by oxidative stress, preventing apoptosis.
Melatonin, and mitochondrial dysfunction
Mitochondrial dysfunction is another consequence of oxidative stress (Kahroba et al. 2021). An excessive production of ROS leads to an inefficacious oxidative phosphorylation, which increases ROS generation even further, forming a vicious circle of mitochondrial dysfunction and oxidative stress (Haider 2015; Michaličková et al. 2020b). Moreover, mutations or deletions in mitochondrial DNA (mtDNA) could occur due to the damage occasioned by ROS, which affects energy metabolism and ATP production (Campbell et al. 2011; Lassmann and van Horssen 2016; Michaličková et al. 2020b).
MS seems to be associated with mitochondrial dysfunction (Soto-Brambila et al. 2017), and it has been observed that any abnormality occurring in the mitochondria could contribute to the onset and progression of lesions in this disease (Campbell and Mahad 2011). In the progressive stages of MS, a chronic mitochondrial dysfunction is experienced (Michaličková et al. 2020b).
It has been demonstrated that melatonin is produced, in addition to by the pineal gland, by the mitochondria (Reiter et al. 2018). The activators of the aryl hydrocarbon receptor (AhR) interact with the mitochondrial melatonergic pathway through cytochrome P450 (CYP)1b1 and convert the melatonin into N-acetylserotonin (NAS) (Anderson et al. 2019). Evidence has shown that there is an increase in the NAS level in secondary-progressive MS, that means a decrease in melatonin levels and an alteration in the melatonergic pathway of the mitochondria in MS (Anderson et al. 2019).
The administration of melatonin seems to have a protective role in mitochondrial dysfunction (Zhao et al. 2019), because it has been seen to increase oxidative phosphorylation through disinhibition of the pyruvate–dehydrogenase complex, which leads to an increase in Acetyl-CoA, which is necessary for the activation of the melatonergic pathway of the mitochondria (Anderson et al. 2019). In addition, it increases the activity of the enzymes intervening in mitochondrial oxidative phosphorylation, such as NADH–coenzyme Q reductase (Complex 1) and cytochrome C oxidase (Complex IV) (Martín et al. 2000b, 2002; Acuña-Castroviejo et al. 2001; Leon et al. 2004; Túnez et al. 2004), which allow melatonin to optimize mitochondrial function (Anderson et al. 2019).
Under oxidative stress it has been proved that there is a decline in the levels of Sirtuin 3 (SIRT3), the principal mitochondrial deacetylase, responsible for maintaining homeostasis and modulating ROS production (Torrens-Mas et al. 2017; Marcus and Andrabi 2018). However, it was found that melatonin treatment can increase and activate SIRT3 (Song et al. 2017; Reiter et al. 2018; Zhou et al. 2019; Morris et al. 2021). What is more, melatonin is capable of: stabilizing the mitochondrial internal membrane, improving electron transport chain activity, reducing oxygen consumption (Paradies et al. 2010; Escribano et al. 2014). It can also inhibit nitric oxide synthase, re-establish mitochondrial calcium homeostasis (Morris et al. 2021), and restore mtDNA levels (Chang et al. 2012; Feng et al. 2013; Escribano et al. 2014).
Melatonin, and iron metabolism
It is considered that oxidative stress is related to the metabolism of iron, since, with an altered redox signaling, iron is released from the myelin sheath (Siotto et al. 2019; Michaličková et al. 2020b). This metal could have a role in the pathogeny of the inflammation and neurodegeneration in MS, causing microglia activation, mitochondrial dysfunction induction, and an increase in free radicals in the CNS (Siotto et al. 2019). During the breakdown of the myelin, iron is released to the extracellular space, where it is converted into a divalent ferrous form, which generates an increase in ROS toxicity (Mahad et al. 2015; Michaličková et al. 2020b). In MS patients, an increase has been found in iron concentration in white matter lesions and grey matter structures (Haider 2015).
Ceruloplasmin (Cp) is a protein produced in the liver, with a positive acute phase, i.e., its level changes in chronic and acute inflammatory diseases (Kamanli et al. 2004; Walshe 2005; Adamczyk-Sowa et al. 2016b; Siotto et al. 2019). It plays a fundamental role in iron and copper metabolism, presenting an antioxidant function due to its ferroxidase activity (Siotto et al. 2019).
Adamczyk-Sowa et al., 2016a, b affirm that ceruloplasmin has potential importance in MS pathogenesis, as it is significantly increased in MS patients, so that it could be a valuable serum marker of the demyelination process (Adamczyk-Sowa et al. 2016b). Moreover, in that same study, they report that melatonin is able to modulate ceruloplasmin concentrations, thus affecting the serum antioxidant system in MS patients (Adamczyk-Sowa et al. 2016b).
In spite of the above findings, further research is needed on the contribution of melatonin to iron metabolism and ceruloplasmin concentrations in MS patients.
Effect of melatonin on intestinal dysbiosis in multiple sclerosis: mechanism of action
The intestinal microbiota has shown itself to be an essential factor in influencing the cellular and humoral components of the immune system, as well as the latter’s responses (Miyake et al. 2015). An alteration in the microbial equilibrium in intestinal microbiota, dysbiosis, has been associated with various autoimmune diseases, including those that affect the CNS (Noto and Miyake 2020). It was seen in EAE that the alteration in certain bacteria populations in the intestine can cause a proinflammatory condition that triggers the onset of MS (Ochoa-Repáraz et al. 2011; Wekerle et al. 2013; Escribano et al. 2017). Thus, it has been hypothesized that intestinal microbiota alterations could have a leading role in MS pathogeny (Chen et al. 2016). It is believed that they could be implicated in circadian dysregulation (Anderson et al. 2019).
The lipopolysaccharide (LPS) is the majority component of the external membrane of Gram-negative bacteria, and is one of the best-characterized pathogen-associated molecular patterns (PAMPs) (Iannucci et al. 2020). LPS reflects the state of the intestinal microbiota and is related to inflammatory processes, stimulating the production of inflammatory cytokines in the intestinal tissue, the CNS and other organs, and to oxidative stress (Hassanpour-Dehkordi and Jivad 2014; Ghareghani et al. 2018; Conde et al. 2019). LPS is composed of a glucolipid, lipid A, which has an essential role in the inflammatory process and is a heteropolysaccharide (Iannucci et al. 2020). The LPS-binding protein, LBP, is a polypeptide of 50 kD, synthesized and secreted in the liver (Nien et al. 2017), that serves as a biomarker of endotoxemia for LPS (Escribano et al. 2017).
LPS is recognized by LBP and the latter binds to the lipid A portion of LPS (Nien et al. 2017; Ghareghani et al. 2018) to, subsequently, form a complex with the LPS membrane receptor, CD14 (Ghareghani et al. 2018; Iannucci et al. 2020). CD14 is disassociated from LBP and divides the LPS aggregators into monomeric molecules (Gioannini and Weiss 2007; Ryu et al. 2017; Ghareghani et al. 2018; Iannucci et al. 2020), which enables LPS transfer to the complex TLR4/MD2 (Ghareghani et al. 2018) (toll-4 type receptor and myeloid-2 differentiation protein, respectively (Nien et al. 2017)). The binding of Lps to the complex TLR4/MD2, triggers the activation of multiple signaling components, such as NF-κB and the interferon regulatory factor 3 (IRF3) (Iannucci et al. 2020) and the production of pro-inflammatory cytokines, such as TNF-α (Kawai and Akira 2010; Ghareghani et al. 2018).
An increase in intestinal permeability is a key point in the pathophysiology of gastrointestinal disorders, in which there is evidence of demyelination (Camara-Lemarroy et al. 2018). It has been demonstrated that there is an increase in intestinal permeability in EAE models and in MS patients (Camara-Lemarroy et al. 2018; Conde et al. 2019), and this suggests that the intestinal microbiota endotoxins enter the circulation (Camara-Lemarroy et al. 2018), arriving both at the CNS and at different body organs (Conde et al. 2019).
In the study made by Escribano et al., 2017, a significantly higher increase in LPS and LBP was obtained in the brain and spine of EAE rats in comparison with that of the control rats, and a positive correlation between oxidative stress and LBP levels in brain, spine and blood (Escribano et al. 2017). In addition, Conde et al. 2019, reported a positive correlation between CP, LPO, LPS and LBP, so that part of the oxidative effect observed in the nerve tissue and blood is associated with LPS and LBP, this being the sign of a possible modification of the intestinal microbiota (Conde et al. 2019).
Role of melatonin in intestinal dysbiosis
The effect of melatonin on intestinal microbiota and LPS is not yet completely clear (Ghareghani et al. 2018; Kim et al. 2020), but more and more studies are being carried out to clarify melatonin’s action mechanism in this condition.
Carrillo-Vico et al. 2005, performed a study in which they analysed melatonin actions in a septic shock induced by LPS in mice, observing that melatonin was capable of protecting the mice from the effect of the LPS by modulating the increase in proinflammatory cytokines triggered by the latter, and increasing the level of the anti-inflammatory cytokine IL-10; it also afforded protection against oxidative damage and apoptosis (Carrillo-Vico et al. 2005). Another study by Yu et al. 2017, in bovine mammary epithelial cells stimulated with LPS, concluded that melatonin inhibits the signaling pathway LPS–CD14–TLR4 and protects against oxidative damage, upregulating the expression of the transcription factor Nfr2 and of haemo-oxygenase-1 (HO-1) (Yu et al. 2017). Similar results were obtained by Shah et al. 2017, who were able to substantiate that the administration of melatonin in rats with LPS-induced oxidative stress activated the signaling pathway Nfr2, and reduced acute neuroinflammation, and neurodegeneration (Shah et al. 2017). Similarly, Ding et al. 2020 demonstrated for the first time that melatonin can protect human alveolar epithelial cells against oxidative stress, effectively inhibiting the epithelial–mesenchymal transition, induced by LPS, through the positive regulation of the pathway Nrf2 (Ding et al. 2020). The recent study by Kim et al. 2020 reports that melatonin is able to reverse intestinal dysbiosis in mice with induced colitis, controlling the microbiota by means of the differentiation of goblet cells and the detection of bacteria through TLR4. It also induces Reg3β, an antimicrobial peptide against Gram-negative bacteria (Kim et al. 2020). Recently published data from our group indicate that treatment with melatonin significantly decreases LPS and LBP levels in the brain and spine of mice with EAE, in comparison with untreated ones (Escribano et al. 2022).
Synergies of melatonin and vitamin D in multiple sclerosis
Up to a few years ago, the effect of vitamin D was exclusively associated with phosphocalcic metabolism (Mocayar-Marón et al. 2020), but it is now known that vitamin D deficiency is a MS risk factor and is correlated with its seriousness (El-Salem et al. 2021). It has been proved that in regions with high altitudes there is a growing prevalence of MS (Bradshaw et al. 2020). Latitude is strongly correlated with the duration and intensity of ultraviolet radiation (UV), the latter being the main source of vitamin D (Holick 1995; Simon et al. 2012). The study made by Ramagopalan et al. 2011, demonstrates that the variations in the gene CYP27B1, that codifies the enzyme 1-α-hydroxylase, which converts into the precursor of vitamin D, 25-hydroxyvitamin D (25(OH)D), the active form of vitamin D (Bradshaw et al. 2020), are strongly associated with the risk of developing MS, since they cause a reduction in the activation of 25(OH)D (Ramagopalan et al. 2011). Another fact backing up the relationship between vitamin D and MS is the prevention and deceleration of the disease in the EAE model after administration of 1,25(OH)2D (Ascherio et al. 2010). In addition, immunological studies show that vitamin D can modulate the immune system, which could be favorable for MS treatment (Simon et al. 2012).
Research has shown that the enzyme 1-α-hydroxylase is not only found in the kidney but it is also expressed in other tissues including the brain, and is present in the prefrontal cortex, hippocampus and hypothalamus, which suggests that this vitamin is important in the regulation of cognitive processes (Huiberts and Smolders 2021). Vitamin D is a potent immune system modulator, a characteristic that it shares with melatonin, both of them being light-dependent mediators (Golan et al. 2013), although their biosynthesis pathways are opposite (Mocayar-Marón et al. 2020). Vitamin D exerts its effects through interaction with a vitamin D nuclear receptor, VDR (Mocayar-Marón et al. 2020).
Vitamin D and melatonin have many shared underlying mechanisms, modulating the same signaling pathways with anti-inflammatory, immunomodulatory, antioxidant and anti-apoptotic effects (Martín Giménez et al. 2020), so that MS has been the cornerstone for establishing relationships with each other (Mocayar-Marón et al. 2020). Melatonin seems to improve vitamin D signaling, increasing VDR expression, but the latter could have a negative regulatory effect on melatonin (Mocayar-Marón et al. 2020), since, in a randomized and double blind study in MS patients made by Golan et al., 2013, it was obtained that supplementation with a high dose of vitamin D during 3 months produced a diminution in the nocturnal secretion of melatonin. Therefore, it has been hypothesized that vitamin D could have an effect on the pineal gland, reducing the melatonin synthesis (Golan et al. 2013). However, it has been possible to establish that the treatment combination of melatonin and vitamin D produces strong synergic effects, observing cytostatic and apoptotic effects on breast cancer cells, protection against lesions due to apoptotic ischemia in rats’ livers, and counteracting adipogenic differentiation (Proietti et al. 2011; Sezgin et al. 2013; Basoli et al. 2017; Mocayar-Marón et al. 2020).
The same as melatonin, vitamin D also exerts a protective effect on the mitochondrial function on increasing its antioxidant activity (Silvagno and Pescarmona 2017).
Despite all the above, more research is necessary, because it is still not known how vitamin D interacts with melatonin synthesis and secretion.
Sex hormones, multiple sclerosis and melatonin
In certain diseases, the sex chromosomes, epigenetic factors and sex hormones influence the risk of suffering from them (Bove and Gilmore 2018). In the case of MS, women are more susceptible to having it (Gold and Voskuhl 2009), with a current ratio of 3:1 with respect to men (Zeydan et al. 2020). This higher female prevalence leads one to think that sex hormones intervene in MS pathogenesis (Gold and Voskuhl 2009). However, there is much controversy about the role that estrogens play in the MS clinical activity in women. Female MS patients register significant improvements during pregnancy, especially in the third month, the moment at which their estrogen and progesterone levels are very high (Gold and Voskuhl 2009). After childbirth, an exacerbation of the symptoms occurs, and, 3 months later, the relapse frequency returns to levels prior to the pregnancy (Gold and Voskuhl 2009; Zeydan et al. 2020). However, after puberty, the prevalence in women begins to increase significantly compared to the prevalence in men. Based on this, it has been determined that puberty, when estrogen and progesterone increase in girls and testosterone in boys (Grumbach 2002), may be a key risk period for the development of MS (Chitnis 2013). In fact, in women, MS onset peaks 2 years after menarche (Waubant 2018). Nevertheless, although at first it might be thought that the cause of the higher MS prevalence in women is a consequence of sexual hormones, there are studies that refer to leptin as a possible cause of the increased MS prevalence in women. Leptin levels, a hormone that affects both the innate and adaptive immune systems, promoting proliferation and skewing towards proinflammatory Th1 responses, increase significantly during puberty (Loffreda et al. 1998). Leptin continues to increase in postadolescent girls, but not in boys, due to increased secretion of testosterone, suggesting that this hormone, and not estrogen, may play a role in the sexual dimorphism of MS (HorlickK et al. 2000; Chitnis 2013).
In addition, in relation to female fertility, it would seem that the latter is diminished in female MS patients, since they present a reduced ovarian reserve (Thöne et al. 2015). Although there are few studies investigating the relationship between MS and the Anti-Müllerian hormone (AMH), the principal ovarian reserve marker. In the study carried out by Thöne et al. 2015 obtains that women suffering from RRMS displayed very low AMH values (< 0.4 ng/ml) in comparison with healthy ones (Thöne et al. 2015), whose mean AMH concentration is of 3.1 + 2.81 ng/ml (Liebenthron et al. 2019). Likewise, a pilot study performed by Sepúlveda et al. 2016, concludes that those women with MS with a greater disease activity had significantly lower AMH levels, antral follicle counts and ovarian volume than those in which the disease had a lower activity (Sepúlveda et al. 2016).
With regard to steroid hormones, estrogens, progesterone and testosterone, they are seen to have a neuroprotective effect, so that an increasing number of studies are investigating the therapeutic use of these hormones in the EAE (Gold and Voskuhl 2009). Testosterone exhibits anti-inflammatory properties (Bove and Gilmore 2018), protects neurons in the spinal cord, induces neuronal differentiation, protects from oxidative stress (Chisu et al. 2006; Gold and Voskuhl 2009) and has an immunomodulatory effect (Sicotte et al. 2007). It has been reported that 40% of the men with MS have low levels of testosterone (Avila et al. 2018), but a treatment with testosterone gel improves the cognitive function and brain atrophy in these patients, according to a clinical assay carried out by Sicotte et al. 2007 (Sicotte et al. 2007). Progesterone exerts an anti-inflammatory effect and has neuroprotective properties (Bove and Gilmore 2018; De Nicola et al. 2018). In addition, in the EAE model it reduces the severity of the disease by means of the decline in demyelination and in the inflammatory response (Avila et al. 2018). Estrogens are known for being antioxidant hormones (AboTaleb and Alghamdi 2020) and they can also interfere in the inflammatory response in such a way that high estrogen levels trigger a change in a pro-inflammatory immune response towards an anti-inflammatory one, whereas low estrogen levels cause the opposite effect (Cutolo and Wilder 2000; Straub 2007; Dupuis et al. 2021). In addition, they contribute to neuroprotection as they promote neuronal plasticity and remyelination, diminishing astrogliosis, and excitotoxicity, and protecting the mitochondrial function (Zeydan et al. 2020). In the EAE model, it was proved that estrogens are capable of increasing regulatory T cell production and reduce MMP-9, which is accompanied by a decrease in the infiltration of T cells into the CNS (Avila et al. 2018). Due to their properties, it has been proposed to use estrogens as a therapy in women with MS, on observing that the administration of 40 µg of OC-ethynilestradiol and 125 µg of desogestrel, has a beneficial effect on inflammatory activity (Pozzilli et al. 2015; Bove and Gilmore 2018). It has also been established that there is a synergy between estrogens and vitamin D, and it was seen that estrogens improved the function of this vitamin, favoring its accumulation and increasing its receptor’s expression (Dupuis et al. 2021). Thus, vitamin D treatments are more effective in women than in men, showing a stronger anti-inflammatory response in the former (Dupuis et al. 2021).
Estrogens share some of their properties with melatonin, suggesting the possibility that they reduce neuroinflammation and apoptosis in a similar way. However, in female mice, melatonin administration has been associated with a decline in estrogen production (Lopes et al. 2016). Similar results were given by Woo et al. 2001, who conclude that melatonin suppresses the action of estrogens, preventing the binding of estradiol to its receptor (Woo et al. 2001). AboTaleb and Alghamdi, 2020, in their study on mice with MS induced by cuprizone, observed that, during the remyelination stage, the effect of melatonin differed between sexes. It was seen that the male mice experienced protective effects after melatonin administration, whereas in the female ones no effects were noted. They, therefore, suggest that there may be a complex interaction that involves exogenous melatonin, remyelination and female sex hormones (AboTaleb and Alghamdi 2020).
Multiple sclerosis, melatonin and neurotrophic factors, neurogenesis and synaptogenesis
Neurotrophic factors are important regulatory proteins that increase neurogenesis, fortify the neuronal network and enhance regenerative responses to nerve aggression (Cobianchi et al. 2016). Their action is mediated by two different types of receptors, the low affinity P75 neurotrophin receptor, (P75NTR), and tyrosine kinase receptors (Trk) (Curtis et al. 1995; Villanueva 2013; Cobianchi et al. 2016). Much of the current research has focused on the study of BDNF as a potential biomarker of MS (Oraby et al. 2021). In MS lesions, BDNF is present in T and microglial cells and in reactive astrocytes (Stadelmann et al. 2002; Naegelin et al. 2020). The results of the study performed by Stadelmann et al. 2002, show that several types of neurons are immunopositive to BDNF in MS patients, and the amount of cells immunopositive to this neurotrophin is correlated with the demyelination activity of the lesions (Stadelmann et al. 2002). Similar results were obtained by Sarchielli et al. 2007, who find a positive correlation between the BDNF levels and the activity of the disease, confirmed by the presence of gadolinium-enhanced lesions (Sarchielli et al. 2007). BDNF is secreted by immune cells in response to neuroimmune and inflammatory cascades to prevent axonal and neuronal damage, and is implicated in the differentiation, survival and growth of neurons (Oraby et al. 2021) and neurogenesis (Palmer et al. 2020). It is also crucial for synaptic plasticity and neuronal network organization in animals and humans (Oraby et al. 2021), but the alteration in the release of neurotrophins may affect these events, causing an exacerbation of the neurogenerative processes in the CNS (Ogłodek et al. 2016). In the research done by Oraby et al., it was found that BDNF is significantly higher in patients with RRMS in the relapsing phase (Oraby et al. 2021). However, other studies like those by Azoulay et al. 2005 and Comini-Frota et al. 2012, point to a decline in BDNF levels (Azoulay et al. 2005; Comini-Frota et al. 2012), which could be related to a diminution in neuroprotection and in the remission potential of MS, thus inducing the progressive phase of the disease (Azoulay et al. 2008; Knaepen et al. 2010).
The alteration in the release of melatonin can influence the concentration of neurotrophic factors, such as BDNF and NGF (Ogłodek et al. 2016). Diverse studies are investigating the function of melatonin in the regulation of neurotrophic factor levels. Duan et al. 2018 obtain that melatonin administration was efficacious in preventing an increase in NGF in the asthma in rats model (Duan et al. 2018). Conversely, Rateb et al. 2017, in their study on rats with a sciatic nerve lesion, conclude that treatment with melatonin increases NGF activity, reinforcing neural recovery and favoring a better nerve regeneration (Rateb et al. 2017). It has also been verified that melatonin can trigger the expression of the glial cell line-derived neurotrophic factor (GDNF), in neural stem cells, which could encourage the survival of dopaminergic neurons (Niles et al. 2004). With respect to BDNF, it has been proved that melatonin levels increase in the mouse hippocampus and enhance neurogenesis (Sugiyama et al. 2020). However, a study performed on breast cancer patients submitted to chemotherapy reported the neuroprotective effect of melatonin on neuroplasticity processes through the diminution of BDNF and Trk serum levels (Palmer et al. 2020). The work of Tasset et al. 2011 concluded that the administration of melatonin in rats treated with 3-nitropropionic acid reduces the neurotrophic factor levels (Tasset et al. 2011). These contradictory results could be due to the melatonin producing different effects, depending on the type of damage, reducing the neurotrophic factor levels as an indication of returning to normal ones (Tasset et al. 2011). However, in general, melatonin’s potential for modulating in vivo neurotrophic factors, through its receptors, could have important implications for optimizing MS therapeutic strategies (Niles et al. 2004).
Melatonin, COVID-19, and multiple sclerosis
In December, 2019, the first case of what was designated as an acute respiratory syndrome severe-coronavirus 2 (SARS-CoV-2) was described; it was subsequently known as coronavirus 2019 disease (COVID-19) (Palao et al. 2020). The evidence suggests that the inflammation, oxidation and an exaggerated immune response contributed to the COVID-19 pathology (Zhang et al. 2020). This virus, in addition, has neurotrophic and neuroinvasive characteristics, so that it can affect patients with MS, interfering in the MS clinical course, causing a worsening of the symptoms (Kataria et al. 2020). Merad and Martin 2020, speculate that the intense immunological stimulation and the systemic stress caused by COVID-19 in MS patients who have a hyperreactive immune system could be responsible for a greater frequency in relapses and the advance of the disease, even after complete recovery from COVID-19 (Merad and Martin 2020; Di Stadio et al. 2020). It is known that MS patients run a greater risk of contracting infections in comparison with the general population (Luna et al. 2020; Willis and Robertson 2020). This could differ depending on the treatment followed by these patients (Luna et al. 2020), since it would appear that those receiving disease-modifying therapy (DMT) are more prone to infections (Kataria et al. 2020).
Taking into account the effects of this virus, and the potentially beneficial effects of melatonin described here, its use as an adjuvant, as well as for the prevention of contagion in MS sufferers, could be proposed (Zhang et al. 2020).
At a prophylaxis level, melatonin can improve the tolerance of the host against invasions of pathogens, including COVID-19 (Tan and Hardeland 2020). One study performed on over 11,000 people indicated that the intake of melatonin reduced the risk of infection (Jehi et al. 2020) and Zhou et al. 2020 reported that melatonin diminished the risk of infection by 64% (Zhou et al. 2020).
Once the infection has been produced, melatonin has shown itself to have effects against neurotropic and non-neurotropic viruses, diminishing the viral title and reducing the production of new progeny or target cells as it inhibits the viral replication processes (Crespo et al. 2016; Huang et al. 2019; Wongchitrat et al. 2021).
COVID-19 can enter the lungs through the dipeptidylpeptidase (DPP4), that is expressed to a great extent in the pulmonary epithelial cells, but it has been found that melatonin can inhibit DPP4, preventing the entry of the virus at a pulmonary level (Wang et al. 2020; Anderson et al. 2020).
Another of the effects triggered by COVID-19 is the activation of the inflammasome NLRP3, which sets off the so-called “cytokine storm” (Fatima et al. 2020), that causes lung inflammation, lesions, and the acute breathing difficulty syndrome (Wu et al. 2019; Fatima et al. 2020). Soares et al. 2019 confirmed that these mechanisms entail a serious risk of developing MS and a progression towards more serious forms of the disease (Soares et al. 2019). Melatonin can inhibit the inflammasomes activated by COVID-19 (Wu et al. 2019; Fatima et al. 2020), so that it would prevent the secretion of the proinflammatory cytokines IL-1β and IL-18 (Lahooti et al. 2021) and reduce the lung condition caused by the virus.
Melatonin is also a promising candidate against the neuroinvasion caused by COVID-19, since it reduces the damage in the CNS (Romero et al. 2020), prevents permeability (Wongchitrat et al. 2021) and restores the homeostasis of the BBB by means of the activation of its receptor MT2 (Romero et al. 2020).
Use of melatonin as an adjuvant in therapies against multiple sclerosis
At present, the objective of MS treatment is to focus on the inflammatory cascade, suppressing the proinflammatory cytokines, as well as reducing the number of relapses and inflammation lesions (Oraby et al. 2021). However, despite important advances, the disease-modifying drugs (DMT) used today for MS do diminish relapse rates but are ineffective for the progressive phase of the disease. So that, research on therapies for that phase is highly necessary (Pegoretti et al. 2020; Martinez and Peplow 2020). 12 immunomodulatory agents have been approved as DMT but many of these therapies have limited or serious side effects (Pegoretti et al. 2020). So that, a combined therapy could be more effective, especially if agents targeting neuroinflammation and neurodegeneration are employed, since they can provide synergic actions (Martinez and Peplow 2020). Melatonin could be used as an adjuvant in MS treatments, due to its properties and its high safety profile (Anderson and Reiter 2020; Anderson et al. 2020).
It is known that the use of drugs such as Natalizumab or Fingolimob increases the risk of infection in MS patients (Wijnands et al. 2018; Luna et al. 2020) but their combination with melatonin could signify a decrease in infections in these patients as melatonin has been demonstrated to have an antiviral effect, regulating the entry of virus (Anderson and Reiter 2020; Anderson et al. 2020) and thus reducing that risk (Jehi et al. 2020).
The data from our group show that transcranial magnetic stimulation (TMS) in EAE rats causes a symptomatic improvement in the mobility scale, as well as oxidative and cellular damage, reducing the degree of cerebral astrocytosis. (Medina-Fernández et al. 2017, 2018; Medina-Fernandez et al. 2017, 2018; Agüera et al. 2020). Prior studies in rats with depression induced by olfactory bulbectomy conclude that the application of TMS improved oxidative stress (Tasset et al. 2010), and increased the serotonin and brain cellularity levels (Medina and Túnez 2013; Estrada et al. 2015). Based on the above, TMS, in combination with melatonin administration, could be proposed for enhancing the beneficial effects of TMS on oxidative damage.
Castro et al., 2005, suggest that a combination of melatonin and valproic acid (VPA), a strong stabilizer of the state of mind, could provide new strategies in neurological diseases, since the neuroprotective properties of VPA implicate a modulation of neurotrophic factors and melatonin receptors (Castro et al. 2005).
Conclusions
Studies relating melatonin to MS have shown that this hormone, due to its antioxidant function, can combat oxidative stress produced by the disease, reducing the main biomarkers of oxidative stress (CP, LPO, NO and MDA), restoring the antioxidant capacity of Nrf2, through the activation of the Nrf2/ARE signaling pathway and protecting against mitochondrial dysfunction. In addition, melatonin could prevent apoptosis, recovering the cellular redox potential, through the induction of Nrf2. Although, perhaps, it would be necessary to start therapy in the early stages of oxidative stress, so that the excess of ROS does not cause irreversible damage. It is important to highlight the evidence that melatonin causes a significant increase in the levels of CAT, SOD, GPx, GSH during the demyelination stage in mice.
Due to its immunomodulatory and anti-inflammatory function, melatonin can control the response of regulatory and effector T cells and decreases the amount of pro-inflammatory cytokines, promoting a more protective cytokine microenvironment. In addition, it has recently been proven that melatonin can counteract and inhibit the effects of the NLRP3 inflammasome, which would also be beneficial during SARS-CoV-2 infection, since NLRP3 is responsible for triggering the cytokine storm, characteristic of COVID-19.
Regarding intestinal dysbiosis, melatonin decreases the levels of LPS and LBP in the EAE model, also showing that melatonin increases antimicrobial peptides, especially Reg3β, which could be useful in controlling the microbiota. In addition, it increases vitamin D signaling and affects neurotrophic factors, modulating their levels depending on the type of damage.
For all that has been described, we can say that in general, melatonin could exert a beneficial effect in people suffering from MS (Fig. 2), running as a promising candidate for the treatment of this disease, either alone or as an adjunct to new treatments that are developed. However, more human studies are needed to confirm the benefits of melatonin treatment in people with MS. Likewise, more research is needed to help understand the possible interaction between melatonin and certain sex hormones, such as estrogens, to know the potential therapeutic efficacy in both men and women.
Mechanisms of action of melatonin on Multiple Sclerosis CNS central nervous system, GDNF glial derivate neurotrophic factor, BDNF brain-derived neurotrophic factor, NGF nerve growth factor, ICAM-1 intercellular adhesion molecule 1, Th1,Th17 Cells T helper 1, T helper 17, Tr1 cells T regulatory 1, IL-10 Interleukin 10, IL-4 Interleukin 4, IL-1 β Interleukin 1 β, TNF tumor necrosis factor, IFN Interferón, VDR vitamin D receptor, LPS lipopolysaccharide, LBP LPS-binding protein, CP Carbonylated proteins, LPO Lipid peroxidation products, NO Nitric oxide, MDA malondialdehyde, GSSG oxidized glutathione, GPx glutathione peroxidase, GSH reduced glutathione, SIRT3 sirtuin 3, NF-κB factor nuclear kappa B, mtDNA mitochondrial DNA, Nrf2 Factor 2 related to nuclear erythroid 2, ROS reactive oxygen species
Data availability
Enquiries about data availability should be directed to the authors.
References
AboTaleb HA, Alghamdi BS (2020) Neuroprotective effects of melatonin during demyelination and remyelination stages in a mouse model of multiple sclerosis. J Mol Neurosci 70:386–402. https://doi.org/10.1007/s12031-019-01425-6
Acuña-Castroviejo D, Martín M, Macías M et al (2001) Melatonin, mitochondria, and cellular bioenergetics. J Pineal Res 30:65–74. https://doi.org/10.1034/J.1600-079X.2001.300201.X
Adamczyk-Sowa M, Sowa P, Adamczyk J et al (2016a) Effect of melatonin supplementation on plasma lipid hydroperoxides, homocysteine concentration and chronic fatigue syndrome in multiple sclerosis patients treated with interferons-beta and mitoxantrone. J Physiol Pharmacol 67:235–242
Adamczyk-Sowa M, Sowa P, Mucha S et al (2016) Changes in serum ceruloplasmin levels based on immunomodulatory treatments and melatonin supplementation in multiple sclerosis patients. Med Sci Monit. https://doi.org/10.12659/MSM.895702
Adamczyk-Sowa M, Galiniak S, Zyracka E et al (2017) Oxidative modification of blood serum proteins in multiple sclerosis after interferon beta and melatonin treatment. Oxid Med Cell Longev. https://doi.org/10.1155/2017/7905148
Agüera E, Caballero-Villarraso J, Feijóo M et al (2020) Clinical and neurochemical effects of transcranial magnetic stimulation (TMS) in multiple sclerosis: a study protocol for a randomized clinical trial. Front Neurol. https://doi.org/10.3389/fneur.2020.00750
Akpinar Z, Tokgöz S, Gökbel H et al (2008) The association of nocturnal serum melatonin levels with major depression in patients with acute multiple sclerosis. Psychiatry Res 161:253–257. https://doi.org/10.1016/j.psychres.2007.11.022
Albazal A, Delshad AA, Roghani M (2021) Melatonin reverses cognitive deficits in streptozotocin-induced type 1 diabetes in the rat through attenuation of oxidative stress and inflammation. J Chem Neuroanat. https://doi.org/10.1016/j.jchemneu.2020.101902
Alghamdi BS, AboTaleb HA (2020) Melatonin improves memory defects in a mouse model of multiple sclerosis by up-regulating cAMP-response element-binding protein and synapse-associated proteins in the prefrontal cortex. J Integr Neurosci 19:229–237. https://doi.org/10.31083/j.jin.2020.02.32
Álvarez-Sánchez N, Cruz-Chamorro I, López-González A et al (2015) Melatonin controls experimental autoimmune encephalomyelitis by altering the T effector/regulatory balance. Brain Behav Immun 50:101–114. https://doi.org/10.1016/j.bbi.2015.06.021
Álvarez-Sánchez N, Cruz-Chamorro I, Díaz-Sánchez M et al (2017) Melatonin reduces inflammatory response in peripheral T helper lymphocytes from relapsing-remitting multiple sclerosis patients. J Pineal Res. https://doi.org/10.1111/jpi.12442
Anderson G, Reiter RJ (2020) Melatonin: roles in influenza, Covid-19, and other viral infections. Rev Med Virol. https://doi.org/10.1002/rmv.2109
Anderson G, Rodriguez M, Reiter RJ (2019) Multiple sclerosis: melatonin, orexin, and ceramide interact with platelet activation coagulation factors and gut-microbiome-derived butyrate in the circadian dysregulation of mitochondria in glia and immune cells. Int J Mol Sci 20(21):5500. https://doi.org/10.3390/ijms20215500
Anderson G, Carbone A, Mazzoccoli G (2020) Aryl hydrocarbon receptor role in co-ordinating sars-cov-2 entry and symptomatology: linking cytotoxicity changes in covid-19 and cancers; modulation by racial discrimination stress. Biology (basel) 9:1–31. https://doi.org/10.3390/biology9090249
Ascherio A (2013) Environmental factors in multiple sclerosis. Expert Rev Neurother 13(12 Suppl):3–9. https://doi.org/10.1586/14737175.2013.865866
Ascherio A, Munger KL, Simon KC (2010) Vitamin D and multiple sclerosis. Lancet Neurol 9:599–612
Avila M, Bansal A, Culberson J, Peiris ANN (2018) The role of sex hormones in multiple sclerosis. Eur Neurol 80:93–99. https://doi.org/10.1159/000494262
Azoulay D, Vachapova V, Shihman B et al (2005) Lower brain-derived neurotrophic factor in serum of relapsing remitting MS: reversal by glatiramer acetate. J Neuroimmunol 167:215–218. https://doi.org/10.1016/j.jneuroim.2005.07.001
Azoulay D, Urshansky N, Karni A (2008) Low and dysregulated BDNF secretion from immune cells of MS patients is related to reduced neuroprotection. J Neuroimmunol 195:186–193. https://doi.org/10.1016/j.jneuroim.2008.01.010
Bahamonde C, Conde C, Agüera E et al (2014) Elevated melatonin levels in natalizumab-treated female patients with relapsing-remitting multiple sclerosis: relationship to oxidative stress. Eur J Pharmacol 730:26–30. https://doi.org/10.1016/j.ejphar.2014.02.020
Basoli V, Santaniello S, Cruciani S et al (2017) Melatonin and vitamin D interfere with the adipogenic fate of adipose-derived stem cells. Int J Mol Sci 18:981. https://doi.org/10.3390/ijms18050981
Beriwal N, Namgyal T, Sangay P, Al Quraan AM (2019) Role of immune-pineal axis in neurodegenerative diseases, unraveling novel hybrid dark hormone therapies. Heliyon. https://doi.org/10.1016/j.heliyon.2019.e01190
Bove R, Gilmore W (2018) Hormones and MS: Risk factors, biomarkers, and therapeutic targets. Mult Scler. https://doi.org/10.1177/1352458517737396
Bradshaw MJ, Holick MF, Stankiewicz JM (2020) Vitamin D and multiple sclerosis. Curr Clin Neurol. https://doi.org/10.1007/978-3-030-24436-1_10
Camara-Lemarroy CR, Metz L, Meddings JB et al (2018) The intestinal barrier in multiple sclerosis: implications for pathophysiology and therapeutics. Brain 141:1900–1916. https://doi.org/10.1093/brain/awy131
Campbell GR, Mahad DJ (2011) Mitochondria as crucial players in demyelinated axons: lessons from neuropathology and experimental demyelination. Autoimmune Dis. https://doi.org/10.4061/2011/262847
Campbell GR, Ziabreva I, Reeve AK et al (2011) Mitochondrial DNA deletions and neurodegeneration in multiple sclerosis. Ann Neurol. https://doi.org/10.1002/ana.22109
Cardinali DP (2019) Melatonin: clinical perspectives in neurodegeneration. Front Endocrinol (Lausanne). https://doi.org/10.3389/fendo.2019.00480
Carrascal L, Nunez-Abades P, Ayala A, Cano M (2018) Role of melatonin in the inflammatory process and its therapeutic potential. Curr Pharm Des 24:1563–1588. https://doi.org/10.2174/1381612824666180426112832
Carrillo-Vico A, Lardone PJ, Naji L et al (2005) Beneficial pleiotropic actions of melatonin in an experimental model of septic shock in mice: regulation of pro-/anti-inflammatory cytokine network, protection against oxidative damage and anti-apoptotic effects. J Pineal Res 39:400–408. https://doi.org/10.1111/j.1600-079X.2005.00265.x
Carvalho AN, Lim JL, Nijland PG et al (2014) Glutathione in multiple sclerosis: more than just an antioxidant? Mult Scler J 20:1425–1431. https://doi.org/10.1177/1352458514533400
Castro LMR, Gallant M, Niles LP (2005) Novel targets for valproic acid: up-regulation of melatonin receptors and neurotrophic factors in C6 glioma cells. J Neurochem 95:1227–1236. https://doi.org/10.1111/j.1471-4159.2005.03457.x
Chang C, Huang H, Lee H et al (2012) Melatonin attenuates kainic acid-induced neurotoxicity in mouse hippocampus via inhibition of autophagy and α-synuclein aggregation. J Pineal Res 52:312–321. https://doi.org/10.1111/J.1600-079X.2011.00945.X
Chang T, Niu C, Sun C et al (2020) Melatonin exerts immunoregulatory effects by balancing peripheral effector and regulatory T helper cells in myasthenia gravis. Aging (Albany NY) 12:21147–21160. https://doi.org/10.18632/aging.103785
Chen J, Chia N, Kalari KR et al (2016) Multiple sclerosis patients have a distinct gut microbiota compared to healthy controls. Sci Rep. https://doi.org/10.1038/srep28484
Chen D, Zhang T, Lee TH (2020) Cellular mechanisms of melatonin: Insight from neurodegenerative diseases. Biomolecules 10:1–26. https://doi.org/10.3390/biom10081158
Chisu V, Manca P, Lepore G et al (2006) Testosterone induces neuroprotection from oxidative stress. Effects on catalase activity and 3-nitro-L-tyrosine incorporation into α-tubulin in a mouse neuroblastoma cell line. Arch Ital Biol 144:63–73. https://doi.org/10.4449/aib.v144i2.882
Chitimus DM, Popescu MR, Voiculescu SE et al (2020) Melatonin’s impact on antioxidative and anti-inflammatory reprogramming in homeostasis and disease. Biomolecules 10:1–28. https://doi.org/10.3390/biom10091211
Chitnis T (2013) Role of puberty in multiple sclerosis risk and course. Clin Immunol 149:192–200. https://doi.org/10.1016/J.CLIM.2013.03.014
Claustrat B, Leston J (2015) Melatonin: physiological effects in humans. Neurochirurgie 61:77–84. https://doi.org/10.1016/J.NEUCHI.2015.03.002
Claustrat B, Brun J, Chazot G (2005) The basic physiology and pathophysiology of melatonin. Sleep Med Rev 9:11–24. https://doi.org/10.1016/j.smrv.2004.08.001
Cobianchi S, Arbat-Plana A, Lopez-Alvarez VM, Navarro X (2016) Neuroprotective effects of exercise treatments after injury: the dual role of neurotrophic factors. Curr Neuropharmacol 15:495–518. https://doi.org/10.2174/1570159x14666160330105132
Comai S, Gobbi G (2014) Unveiling the role of melatonin MT2 receptors in sleep, anxiety and other neuropsychiatric diseases: a novel target in psychopharmacology. J Psychiatry Neurosci 39(1):6–21. https://doi.org/10.1503/jpn.130009
Comini-Frota ER, Rodrigues DH, Miranda EC et al (2012) Serum levels of brain-derived neurotrophic factor correlate with the number of T2 MRI lesions in multiple sclerosis. Brazilian J Med Biol Res 45:68–71. https://doi.org/10.1590/S0100-879X2011007500165
Compston A, Coles A (2002) Multiple sclerosis. Lancet 359:1221–1231. https://doi.org/10.1016/S0140-6736(02)08220-X
Compston A, Coles A (2008) Multiple sclerosis. Lancet 372:1502–1517. https://doi.org/10.1016/S0140-6736(08)61620-7
Conde C, Escribano BM, Luque E et al (2019) Extra-virgin olive oil modifies the changes induced in non-nervous organs and tissues by experimental autoimmune encephalomyelitis models. Nutrients. https://doi.org/10.3390/nu11102448
Constantinescu CS, Hilliard B, Ventura E, Rostami A (1997) Luzindole, a melatonin receptor antagonist, suppresses experimental autoimmune encephalomyelitis. Pathobiology. https://doi.org/10.1159/000164122
Crespo I, San-Miguel B, Sánchez DI et al (2016) Melatonin inhibits the sphingosine kinase 1/sphingosine-1-phosphate signaling pathway in rabbits with fulminant hepatitis of viral origin. J Pineal Res. https://doi.org/10.1111/jpi.12335
Curtis R, Adryan KM, Stark JL et al (1995) Differential role of the low affinity neurotrophin receptor (p75) in retrograde axonal transport of the neurotrophins. Neuron 14:1201–1211. https://doi.org/10.1016/0896-6273(95)90267-8
Cutolo M, Wilder RL (2000) Different roles for androgens and estrogens in the susceptibility to autoimmune rheumatic diseases. Rheum Dis Clin North Am 26:825–839. https://doi.org/10.1016/S0889-857X(05)70171-X
Das R, Balmik AA, Chinnathambi S (2020) Melatonin reduces GSK3β-mediated Tau phosphorylation, enhances Nrf2 nuclear translocation and anti-inflammation. ASN Neuro. https://doi.org/10.1177/1759091420981204
De Nicola AF, Garay LI, Meyer M et al (2018) Neurosteroidogenesis and progesterone anti-inflammatory/neuroprotective effects. J Neuroendocrinol 30:e12502. https://doi.org/10.1111/jne.12502
Di Monte D, Chan P, Sandy M (1992) Glutathione in Parkinson’s disease: a link between oxidative stress and mitochondrial damage? Ann Neurol 32(Suppl):S111–S115. https://doi.org/10.1002/ANA.410320719
Di Stadio A, Romani L, Bernitsas E (2020) Could sars-Cov2 affect MS progression? Mult Scler Relat Disord. https://doi.org/10.1016/j.msard.2020.102540
Diez V, Traikov S, Schmeisser K et al (2021) Glycolate combats massive oxidative stress by restoring redox potential in caenorhabditis elegans. Commun Biol 4:1–13. https://doi.org/10.1038/s42003-021-01669-2
Ding Z, Wu X, Wang Y et al (2020) Melatonin prevents LPS-induced epithelial-mesenchymal transition in human alveolar epithelial cells via the GSK-3β/Nrf2 pathway. Biomed Pharmacother. https://doi.org/10.1016/j.biopha.2020.110827
Dizdaroglu M (2005) Base-excision repair of oxidative DNA damage by DNA glycosylases. Mutat Res 591:45–59. https://doi.org/10.1016/J.MRFMMM.2005.01.033
Duan J, Kang J, Qin W et al (2018) Exposure to formaldehyde and diisononyl phthalate exacerbate neuroinflammation through NF-κB activation in a mouse asthma model. Ecotoxicol Environ Saf 163:356–364. https://doi.org/10.1016/j.ecoenv.2018.07.089
Dupuis ML, Pagano MT, Pierdominici M, Ortona E (2021) The role of vitamin D in autoimmune diseases: could sex make the difference? Biol Sex Differ. https://doi.org/10.1186/s13293-021-00358-3
El-Salem K, Khalil H, Al-Sharman A et al (2021) Serum vitamin d inversely correlates with depression scores in people with multiple sclerosis. Mult Scler Relat Disord. https://doi.org/10.1016/j.msard.2020.102732
Escribano BM, Colin-Gonzalez A, Santamaria A, Tunez I (2014) The role of melatonin in multiple sclerosis, Huntington’s disease and cerebral ischemia. CNS Neurol Disord - Drug Targets 13:1096–1119. https://doi.org/10.2174/1871527313666140806160400
Escribano BM, Medina-Fernández FJ, Aguilar-Luque M et al (2017) Lipopolysaccharide binding protein and oxidative stress in a multiple sclerosis model. Neurotherapeutics. https://doi.org/10.1007/s13311-016-0480-0
Escribano BM, Muñoz-Jurado A, Caballero-Villarraso J et al (2022) Protective effects of melatonin on changes occurring in the experimental autoimmune encephalomyelitis model of multiple sclerosis. Mult Scler Relat Disord 58:103520. https://doi.org/10.1016/J.MSARD.2022.103520
Esposito E, Cuzzocrea S (2010) Antiinflammatory activity of melatonin in central nervous system. Curr Neuropharmacol 8:228–242. https://doi.org/10.2174/157015910792246155
Estrada C, López D, Conesa A et al (2015) Cognitive impairment after sleep deprivation rescued by transcranial magnetic stimulation application in octodon degus. Neurotox Res 28:361–371. https://doi.org/10.1007/s12640-015-9544-x
Faissner S, Plemel JR, Gold R, Yong VW (2019) Progressive multiple sclerosis: from pathophysiology to therapeutic strategies. Nat Rev Drug Discov 18:905–922. https://doi.org/10.1038/s41573-019-0035-2
Farez MF, Mascanfroni ID, Méndez-Huergo SP et al (2015) Melatonin contributes to the seasonality of multiple sclerosis relapses. Cell 162:1338–1352. https://doi.org/10.1016/j.cell.2015.08.025
Farez MF, Calandri IL, Correale J, Quintana FJ (2016) Anti-inflammatory effects of melatonin in multiple sclerosis. BioEssays 38:1016–1026. https://doi.org/10.1002/bies.201600018
Fatima S, Zaidi SS, Alsharidah AS et al (2020) Possible prophylactic approach for SARS-CoV-2 infection by combination of melatonin, vitamin C and Zinc in animals. Front Vet Sci. https://doi.org/10.3389/fvets.2020.585789
Feng Y, Jia Y, Su L et al (2013) Decreased mitochondrial DNA copy number in the hippocampus and peripheral blood during opiate addiction is mediated by autophagy and can be salvaged by melatonin. Autophagy 9:1395–1406. https://doi.org/10.4161/AUTO.25468
Feng YS, Tan ZX, Wu LY et al (2021) The involvement of NLRP3 inflammasome in the treatment of neurodegenerative diseases. Biomed Pharmacother. https://doi.org/10.1016/j.biopha.2021.111428
Fernández-Ortiz M, Sayed RKA, Fernández-Martínez J et al (2020) Melatonin/Nrf2/NLRP3 connection in mouse heart mitochondria during aging. Antioxidants 9:1–22. https://doi.org/10.3390/antiox9121187
Fukutomi T, Takagi K, Mizushima T et al (2014) Kinetic, thermodynamic, and structural characterizations of the association between Nrf2-DLGex degron and keap1. Mol Cell Biol. https://doi.org/10.1128/mcb.01191-13
García JA, Volt H, Venegas C et al (2015) Disruption of the NF-κB/NLRP3 connection by melatonin requires retinoid-related orphan receptor-a and blocks the septic response in mice. FASEB J 29:3863–3875. https://doi.org/10.1096/fj.15-273656
Ghareghani M, Dokoohaki S, Ghanbari A et al (2017a) Melatonin exacerbates acute experimental autoimmune encephalomyelitis by enhancing the serum levels of lactate: a potential biomarker of multiple sclerosis progression. Clin Exp Pharmacol Physiol 44:52–61. https://doi.org/10.1111/1440-1681.12678
Ghareghani M, Sadeghi H, Zibara K et al (2017b) Melatonin increases oligodendrocyte differentiation in cultured neural stem cells. Cell Mol Neurobiol 37:1319–1324. https://doi.org/10.1007/S10571-016-0450-4
Ghareghani M, Reiter RJ, Zibara K, Farhadi N (2018) Latitude, vitamin D, melatonin, and gut microbiota act in concert to initiate multiple sclerosis: a new mechanistic pathway. Front Immunol 9:2484. https://doi.org/10.3389/fimmu.2018.02484
Ghareghani M, Scavo L, Jand Y et al (2019) Melatonin therapy modulates cerebral metabolism and enhances remyelination by increasing PDK4 in a mouse model of multiple sclerosis. Front Pharmacol. https://doi.org/10.3389/fphar.2019.00147
Giannoulia-Karantana A, Vlachou A, Polychronopoulou S et al (2007) Melatonin and immunomodulation: connections and potential clinical applications. NeuroImmunoModulation 13:133–144. https://doi.org/10.1159/000097258
Gioannini TL, Weiss JP (2007) Regulation of interactions of Gram-negative bacterial endotoxins with mammalian cells. Immunol Res 39:249–260. https://doi.org/10.1007/s12026-007-0069-0
Golan D, Staun-Ram E, Glass-Marmor L et al (2013) The influence of vitamin D supplementation on melatonin status in patients with multiple sclerosis. Brain Behav Immun. https://doi.org/10.1016/j.bbi.2013.04.010
Gold SM, Voskuhl RR (2009) Estrogen and testosterone therapies in multiple sclerosis. Prog Brain Res 175:239–251. https://doi.org/10.1016/S0079-6123(09)17516-7
Gold SM, Schulz KH, Hartmann S et al (2003) Basal serum levels and reactivity of nerve growth factor and brain-derived neurotrophic factor to standardized acute exercise in multiple sclerosis and controls. J Neuroimmunol 138:99–105. https://doi.org/10.1016/S0165-5728(03)00121-8
Goldenberg MM (2012) Multiple sclerosis review. PT 37:175–184
Gonsette R (2008) Oxidative stress and excitotoxicity: a therapeutic issue in multiple sclerosis? Mult Scler 14:22–34. https://doi.org/10.1177/1352458507080111
Grumbach MM (2002) The neuroendocrinology of human puberty revisited. Horm Res Paediatr 57:2–14. https://doi.org/10.1159/000058094
Gunata M, Parlakpinar H, Acet HA (2020) Melatonin: a review of its potential functions and effects on neurological diseases. Rev Neurol (paris) 176:148–165. https://doi.org/10.1016/j.neurol.2019.07.025
Haider L (2015) Inflammation, iron, energy failure, and oxidative stress in the pathogenesis of multiple sclerosis. Oxid Med Cell Longev. https://doi.org/10.1155/2015/725370
Harbo HF, Gold R, Tintora M (2013) Sex and gender issues in multiple sclerosis. Ther Adv Neurol Disord. https://doi.org/10.1177/1756285613488434
Hassanpour-Dehkordi A, Jivad N (2014) Comparison of regular aerobic and yoga on the quality of life in patients with multiple sclerosis. Med J Islam Repub Iran 28:141
Hauser S, Goodwin D (2008) Multiple sclerosis and other demyelinating diseases. Harrison’s principles of internal medicine, 17th edn. McGraw-Hill Medical, New York, pp 2611–2621
Hofman FM, Hinton DR, Johnson K, Merrill JE (1989) Tumor necrosis factor identified in multiple sclerosis brain. J Exp Med. https://doi.org/10.1084/jem.170.2.607
Holick MF (1995) Environmental factors that influence the cutaneous production of vitamin D. Am J Clin Nutr. https://doi.org/10.1093/ajcn/61.3.638S
Holton KF, Kirkland AE (2020) Moving past antioxidant supplementation for the dietary treatment of multiple sclerosis. Mult Scler J 26:1012–1023. https://doi.org/10.1177/1352458519893925
HorlickK MB, Rosenbaum M, Nicholson M et al (2000) Effect of puberty on the relationship between circulating leptin and body composition. J Clin Endocrinol Metab 85:2509–2518. https://doi.org/10.1210/JCEM.85.7.6689
Huang WJ, Chen WW, Zhang X (2017) Multiple sclerosis: pathology, diagnosis and treatments (review). Exp Ther Med 13:3163–3166. https://doi.org/10.3892/etm.2017.4410
Huang SH, Liao CL, Chen SJ et al (2019) Melatonin possesses an anti-influenza potential through its immune modulatory effect. J Funct Foods. https://doi.org/10.1016/j.jff.2019.04.062
Huiberts LM, Smolders KCHJ (2021) Effects of vitamin D on mood and sleep in the healthy population: interpretations from the serotonergic pathway. Sleep Med Rev. https://doi.org/10.1016/j.smrv.2020.101379
Iannucci A, Caneparo V, Raviola S et al (2020) Toll-like receptor 4-mediated inflammation triggered by extracellular IFI16 is enhanced by lipopolysaccharide binding. PLoS Pathog. https://doi.org/10.1371/JOURNAL.PPAT.1008811
Jehi L, Ji X, Milinovich A et al (2020) Individualizing risk prediction for positive coronavirus disease 2019 testing: results from 11,672 patients. Chest. https://doi.org/10.1016/j.chest.2020.05.580
Jin YP, De Pedro-Cuesta J, Söderström M et al (2000) Seasonal patterns in optic neuritis and multiple sclerosis: a meta-analysis. J Neurol Sci 181:56–64. https://doi.org/10.1016/S0022-510X(00)00408-1
Johnson DA, Amirahmadi S, Ward C et al (2009) The absence of the pro-antioxidant transcription factor Nrf2 exacerbates experimental autoimmune encephalomyelitis. Toxicol Sci. https://doi.org/10.1093/toxsci/kfp274
Kahroba H, Ramezani B, Maadi H et al (2021) The role of Nrf2 in neural stem/progenitors cells: from maintaining stemness and self-renewal to promoting differentiation capability and facilitating therapeutic application in neurodegenerative disease. Ageing Res Rev. https://doi.org/10.1016/j.arr.2020.101211
Kamanli A, Naziroǧlu M, Aydilek N, Hacievliyagil C (2004) Plasma lipid peroxidation and antioxidant levels in patients with rheumatoid arthritis. Cell Biochem Funct. https://doi.org/10.1002/cbf.1055
Kang JC, Ahn M, Kim YS et al (2001) Melatonin ameliorates autoimmune encephalomyelitis through suppression of intercellular adhesion molecule-1. J Vet Sci (Suwon-si, Korea). https://doi.org/10.4142/jvs.2001.2.2.85
Kataria S, Tandon M, Melnic V, Sriwastava S (2020) A case series and literature review of multiple sclerosis and COVID-19: clinical characteristics, outcomes and a brief review of immunotherapies. eNeurologicalSci. https://doi.org/10.1016/j.ensci.2020.100287
Katsuoka F, Yamamoto M (2016) Small maf proteins (MafF, MafG, MafK): history, structure and function. Gene 586:197–205. https://doi.org/10.1016/j.gene.2016.03.058
Kawai T, Akira S (2010) The role of pattern-recognition receptors in innate immunity: update on toll-like receptors. Nat Immunol 11:373–384. https://doi.org/10.1038/ni.1863
Kebir H, Kreymborg K, Ifergan I et al (2007) Human TH17 lymphocytes promote blood-brain barrier disruption and central nervous system inflammation. Nat Med. https://doi.org/10.1038/nm1651
Kern S, Geiger M, Paucke M et al (2019) Clinical relevance of circadian melatonin release in relapsing-remitting multiple sclerosis. J Mol Med 97:1547–1555. https://doi.org/10.1007/s00109-019-01821-w
Kim SW, Kim S, Son M et al (2020) Melatonin controls microbiota in colitis by goblet cell differentiation and antimicrobial peptide production through Toll-like receptor 4 signalling. Sci Rep. https://doi.org/10.1038/s41598-020-59314-7
Knaepen K, Goekint M, Heyman EM, Meeusen R (2010) Neuroplasticity exercise-induced response of peripheral brain-derived neurotrophic factor: a systematic review of experimental studies in human subjects. Sport Med 40:765–801. https://doi.org/10.2165/11534530-000000000-00000
Kroenke MA, Carlson TJ, Andjelkovic AV, Segal BM (2008) IL-12- and IL-23-modulated T cells induce distinct types of EAE based on histology, CNS chemokine profile, and response to cytokine inhibition. J Exp Med. https://doi.org/10.1084/jem.20080159
Kubo E, Chhunchha B, Singh P et al (2017) Sulforaphane reactivates cellular antioxidant defense by inducing Nrf2/ARE/Prdx6 activity during aging and oxidative stress. Sci Rep 7:1–17. https://doi.org/10.1038/s41598-017-14520-8
Lahooti B, Chhibber T, Bagchi S et al (2021) Therapeutic role of inflammasome inhibitors in neurodegenerative disorders. Brain Behav Immun 91:771–783. https://doi.org/10.1016/j.bbi.2020.11.004
Langhnoja J, Buch L, Pillai P (2021) Potential role of NGF, BDNF, and their receptors in oligodendrocytes differentiation from neural stem cell: an in vitro study. Cell Biol Int 45:432–446. https://doi.org/10.1002/cbin.11500
Lassmann H, van Horssen J (2016) Oxidative stress and its impact on neurons and glia in multiple sclerosis lesions. Biochim Biophys Acta - Mol Basis Dis. https://doi.org/10.1016/j.bbadis.2015.09.018
Lassmann H, Brück W, Lucchinetti CF (2007) The immunopathology of multiple sclerosis: an overview. Brain Pathol 17:210–218. https://doi.org/10.1111/j.1750-3639.2007.00064.x
Lassmann H, van Horssen J, Mahad D (2012) Progressive multiple sclerosis: pathology and pathogenesis. Nat Rev Neurol 8:647–656. https://doi.org/10.1038/NRNEUROL.2012.168
Leon J, Acuña-Castroviejo D, Sainz R et al (2004) Melatonin and mitochondrial function. Life Sci 75:765–790. https://doi.org/10.1016/J.LFS.2004.03.003
Li DY, Smith DG, Hardel R et al (2013) Melatonin receptor genes in vertebrates. Int J Mol Sci 14:11208–11223. https://doi.org/10.3390/ijms140611208
Licht-Mayer S, Wimmer I, Traffehn S et al (2015) Cell type-specific Nrf2 expression in multiple sclerosis lesions. Acta Neuropathol 130:263–277. https://doi.org/10.1007/s00401-015-1452-x
Liebenthron J, Reinsberg J, Van Der Ven K et al (2019) Serum anti-müllerian hormone concentration and follicle density throughout reproductive life and in different diseases - implications in fertility preservation. Hum Reprod 34:2513–2522. https://doi.org/10.1093/humrep/dez215
Lin GJ, Huang SH, Chen SJ et al (2013) Modulation by melatonin of the pathogenesis of inflammatory autoimmune diseases. Int J Mol Sci 14:11742–11766. https://doi.org/10.3390/ijms140611742
Lock C, Hermans G, Pedotti R et al (2002) Gene-microarray analysis of multiple sclerosis lesions yields new targets validated in autoimmune encephalomyelitis. Nat Med. https://doi.org/10.1038/nm0502-500
Loffreda S, Yang SQ, Lin HZ et al (1998) Leptin regulates proinflammatory immune responses. FASEB J 12:57–65. https://doi.org/10.1096/FSB2FASEBJ.12.1.57
Long T, Yang Y, Peng L, Li Z (2018) Neuroprotective effects of melatonin on experimental allergic encephalomyelitis mice via anti-oxidative stress activity. J Mol Neurosci 64:233–241. https://doi.org/10.1007/s12031-017-1022-x
Lopes J, Arnosti D, Trosko JE et al (2016) Melatonin decreases estrogen receptor binding to estrogen response elements sites on the oct4 gene in human breast cancer stem cells. Genes and Cancer 7:209–217. https://doi.org/10.18632/genesandcancer.107
Luna G, Alping P, Burman J et al (2020) Infection risks among patients with multiple sclerosis treated with fingolimod, natalizumab, rituximab, and injectable therapies. JAMA Neurol. https://doi.org/10.1001/jamaneurol.2019.3365
Luo J, Zhang Z, Sun H et al (2020) Effect of melatonin on T/B cell activation and immune regulation in pinealectomy mice. Life Sci. https://doi.org/10.1016/j.lfs.2019.117191
Maes M, Landucci Bonifacio K, Morelli NR et al (2019) Major differences in neurooxidative and neuronitrosative stress pathways between major depressive disorder and types I and II bipolar disorder. Mol Neurobiol 56:141–156. https://doi.org/10.1007/S12035-018-1051-7/TABLES/5
Mahad DH, Trapp BD, Lassmann H (2015) Pathological mechanisms in progressive multiple sclerosis. Lancet Neurol 14:183–193. https://doi.org/10.1016/S1474-4422(14)70256-X
Maldonado MD, Mora-Santos M, Naji L et al (2010) Evidence of melatonin synthesis and release by mast cells. Possible modulatory role on inflammation. Pharmacol Res 62:282–287. https://doi.org/10.1016/j.phrs.2009.11.014
Marcus JM, Andrabi SA (2018) SIRT3 Regulation under cellular stress: making sense of the ups and downs. Front Neurosci 12:799. https://doi.org/10.3389/fnins.2018.00799
Martín M, Macías M, Escames G et al (2000a) Melatonin but not vitamins C and E maintains glutathione homeostasis in t-butyl hydroperoxide-induced mitochondrial oxidative stress. FASEB J 14:1677–1679. https://doi.org/10.1096/FJ.99-0865FJE
Martín M, Macías M, Escames G et al (2000b) Melatonin-induced increased activity of the respiratory chain complexes I and IV can prevent mitochondrial damage induced by ruthenium red in vivo. J Pineal Res 28:242–248. https://doi.org/10.1034/J.1600-079X.2000.280407.X
Martín M, Macías M, León J et al (2002) Melatonin increases the activity of the oxidative phosphorylation enzymes and the production of ATP in rat brain and liver mitochondria. Int J Biochem Cell Biol 34:348–357. https://doi.org/10.1016/S1357-2725(01)00138-8
Martín Giménez VM, Inserra F, Tajer CD et al (2020) Lungs as target of COVID-19 infection: protective common molecular mechanisms of vitamin D and melatonin as a new potential synergistic treatment. Life Sci. https://doi.org/10.1016/j.lfs.2020.117808
Martinez B, Peplow PV (2020) Protective effects of pharmacological therapies in animal models of multiple sclerosis: a review of studies 2014–2019. Neural Regen Res 15:1220–1234. https://doi.org/10.4103/1673-5374.272572
Matías-Guiu J, Gomez-Pinedo U, Montero-Escribano P et al (2020) Should we expect neurological symptoms in the SARS-CoV-2 epidemic? Neurologia 35:170–175. https://doi.org/10.1016/j.nrl.2020.03.001
Medina FJ, Túnez I (2013) Mechanisms and pathways underlying the therapeutic effect of transcranial magnetic stimulation. Rev Neurosci 24:507–525. https://doi.org/10.1515/revneuro-2013-0024
Medina-Fernandez F, Escribano B, Agüera E et al (2017) Effects of transcranial magnetic stimulation on oxidative stress in experimental autoimmune encephalomyelitis. Free Radic Res 51:460–469. https://doi.org/10.1080/10715762.2017.1324955
Medina-Fernandez F, Escribano B, Luque E et al (2018) Comparative of transcranial magnetic stimulation and other treatments in experimental autoimmune encephalomyelitis. Brain Res Bull 137:140–145. https://doi.org/10.1016/J.BRAINRESBULL.2017.11.018
Medina-Fernández FJ, Luque E, Aguilar-Luque M et al (2017) Transcranial magnetic stimulation modifies astrocytosis, cell density and lipopolysaccharide levels in experimental autoimmune encephalomyelitis. Life Sci. https://doi.org/10.1016/j.lfs.2016.11.011
Medina-Fernández F, Escribano B, Padilla-Del-Campo C et al (2018) Transcranial magnetic stimulation as an antioxidant. Free Radic Res 52:381–389. https://doi.org/10.1080/10715762.2018.1434313
Melatonin in Patients With Multiple Sclerosis (MS). - Full Text View - ClinicalTrials.gov. https://clinicaltrials.gov/ct2/show/NCT3498131/. Accessed 3 Sep 2021
Mendiola AS, Cardona AE (2018) The IL-1β phenomena in neuroinflammatory diseases. J Neural Transm 125:781–795. https://doi.org/10.1007/s00702-017-1732-9
Merad M, Martin JC (2020) Pathological inflammation in patients with COVID-19: a key role for monocytes and macrophages. Nat Rev Immunol 20:355–362. https://doi.org/10.1038/s41577-020-0331-4
Michaličková D, Hrnčíř T, Canová NK, Slanař O (2020a) Targeting Keap1/Nrf2/ARE signaling pathway in multiple sclerosis. Eur J Pharmacol. https://doi.org/10.1016/j.ejphar.2020.172973
Michaličková D, Šíma M, Slanař O (2020) New insights in the mechanisms of impaired redox signaling and its interplay with inflammation and immunity in multiple sclerosis. Physiol Res 69:1–19. https://doi.org/10.33549/physiolres.934276
Miller E, Mrowicka M, Malinowska K et al (2011) Effects of whole-body cryotherapy on a total antioxidative status and activities of antioxidative enzymes in blood of depressive multiple sclerosis patients. World J Biol Psychiatry 12:223–227. https://doi.org/10.3109/15622975.2010.518626
Miller E, Walczak A, Majsterek I, Kędziora J (2013) Melatonin reduces oxidative stress in the erythrocytes of multiple sclerosis patients with secondary progressive clinical course. J Neuroimmunol 257:97–101. https://doi.org/10.1016/J.JNEUROIM.2013.02.012
Miyake S, Kim S, Suda W et al (2015) Dysbiosis in the gut microbiota of patients with multiple sclerosis, with a striking depletion of species belonging to clostridia XIVa and IV clusters. PLoS ONE. https://doi.org/10.1371/journal.pone.0137429
Mocayar-Marón FJ, Ferder L, Reiter RJ, Manucha W (2020) Daily and seasonal mitochondrial protection: unraveling common possible mechanisms involving vitamin D and melatonin. J Steroid Biochem Mol Biol. https://doi.org/10.1016/j.jsbmb.2020.105595
Morris G, Walker AJ, Walder K et al (2021) Increasing Nrf2 activity as a treatment approach in neuropsychiatry. Mol Neurobiol 58:2158–2182. https://doi.org/10.1007/s12035-020-02212-w
Musshoff U, Riewenherm D, Berger E et al (2002) Melatonin receptors in rat hippocampus: molecular and functional investigations. Hippocampus. https://doi.org/10.1002/hipo.1105
Naegelin Y, Saeuberli K, Schaedelin S et al (2020) Levels of brain-derived neurotrophic factor in patients with multiple sclerosis. Ann Clin Transl Neurol 7:2251–2261. https://doi.org/10.1002/acn3.51215
Nien HC, Hsu SJ, Su TH et al (2017) High serum lipopolysaccharide-binding protein level in chronic hepatitis C viral infection is reduced by anti-viral treatments. PLoS ONE. https://doi.org/10.1371/journal.pone.0170028
Niles LP, Armstrong KJ, Rincón Castro LM et al (2004) Neural stem cells express melatonin receptors and neurotrophic factors: colocalization of the MT1 receptor with neuronal and glial markers. BMC Neurosci. https://doi.org/10.1186/1471.2202-5-41
Noto D, Miyake S (2020) Gut dysbiosis and multiple sclerosis. Clin Immunol. https://doi.org/10.1016/j.clim.2020.108380
Ochoa-Repáraz J, Mielcarz DW, Begum- Haque S, Kasper LH (2011) Gut, bugs, and brain: role of commensal bacteria in the control of central nervous system disease. Ann Neurol. https://doi.org/10.1002/ana.22344
Ogłodek EA, Just MJ, Szromek AR, Araszkiewicz A (2016) Melatonin and neurotrophins NT-3, BDNF, NGF in patients with varying levels of depression severity. Pharmacol Reports 68:945–951. https://doi.org/10.1016/j.pharep.2016.04.003
Onaolapo OJ, Onaolapo AY, Olowe OA et al (2019) Melatonin and melatonergic influence on neuronal transcription factors: implications for the development of novel therapies for neurodegenerative disorders. Curr Neuropharmacol 18:563–577. https://doi.org/10.2174/1570159x18666191230114339
Ontaneda D, Hyland M, Cohen JA (2012) Multiple sclerosis: new insights in pathogenesis and novel therapeutics. Annu Rev Med 63:389–404. https://doi.org/10.1146/annurev-med-042910-135833
Oraby MI, El Masry HA, Abd El Shafy SS, Abdul Galil EM (2021) Serum level of brain-derived neurotrophic factor in patients with relapsing–remitting multiple sclerosis: a potential biomarker for disease activity. Egypt J Neurol Psychiatry Neurosurg. https://doi.org/10.1186/s41983-021-00296-2
Padureanu R, Albu CV, Mititelu RR et al (2019) Oxidative stress and inflammation interdependence in multiple sclerosis. J Clin Med 8:1815. https://doi.org/10.3390/JCM8111815
Palao M, Fernández-Díaz E, Gracia-Gil J et al (2020) Multiple sclerosis following SARS-CoV-2 infection. Mult Scler Relat Disord. https://doi.org/10.1016/j.msard.2020.102377
Palmer ACS, Zortea M, Souza A et al (2020) Clinical impact of melatonin on breast cancer patients undergoing chemotherapy; effects on cognition, sleep and depressive symptoms: a randomized, double-blind, placebo-controlled trial. PLoS ONE. https://doi.org/10.1371/journal.pone.0231379
Pandit A, Vadnal J, Houston S et al (2009) Impaired regulation of electron transport chain subunit genes by nuclear respiratory factor 2 in multiple sclerosis. J Neurol Sci. https://doi.org/10.1016/j.jns.2009.01.009
Paradies G, Petrosillo G, Paradies V et al (2010) Melatonin, cardiolipin and mitochondrial bioenergetics in health and disease. J Pineal Res 48:297–310. https://doi.org/10.1111/j.1600-079X.2010.00759.x
Park JS, Piao J, Park G, Hong HS (2020) Substance-P restores cellular activity of adsc impaired by oxidative stress. Antioxidants 9:1–10. https://doi.org/10.3390/ANTIOX9100978
Patsopoulos NA, Barcellos LF, Hintzen RQ et al (2013) Fine-mapping the genetic association of the major histocompatibility complex in multiple sclerosis: HLA and Non-HLA effects. PLoS Genet. https://doi.org/10.1371/journal.pgen.1003926
Pegoretti V, Swanson KA, Bethea JR et al (2020) Inflammation and oxidative stress in multiple sclerosis: consequences for therapy development. Oxid Med Cell Longev. https://doi.org/10.1155/2020/7191080
Pozzilli C, De Giglio L, Barletta VT et al (2015) Oral contraceptives combined with interferon b in multiple sclerosis. Neurol Neuroimmunol NeuroInflammation. https://doi.org/10.1212/NXI.0000000000000120
Proietti S, Cucina A, D’Anselmi F et al (2011) Melatonin and vitamin D 3 synergistically down-regulate Akt and MDM2 leading to TGFβ-1-dependent growth inhibition of breast cancer cells. J Pineal Res 50:150–158. https://doi.org/10.1111/j.1600-079X.2010.00824.x
Ramagopalan SV, Dyment DA, Cader MZ et al (2011) Rare variants in the CYP27B1 gene are associated with multiple sclerosis. Ann Neurol 70:881–886. https://doi.org/10.1002/ana.22678
Ramirez-Ramirez V, Macias-Islas MA, Ortiz GG et al (2013) Efficacy of fish oil on serum of TNF α, IL-1 β, and IL-6 oxidative stress markers in multiple sclerosis treated with interferon beta-1b. Oxid Med Cell Longev. https://doi.org/10.1155/2013/709493
Ramos González EJ, Ramirez Jirano LJ, García Martínez DZ et al (2018) Estudio comparativo de melatonina contra los tratamientos inmunomoduladores (interferón beta y acetato de glatirámero) en un modelo murino de esclerosis múltiple. Neurologia. https://doi.org/10.1016/j.nrl.2018.01.007
Rateb EE, Amin SN, El-Tablawy N et al (2017) Effect of melatonin supplemented at the light or dark period on recovery of sciatic nerve injury in rats. EXCLI J 16:138–150. https://doi.org/10.1779/excli2016-763
Reiter R, Calvo J, Karbownik M et al (2000) Melatonin and its relation to the immune system and inflammation. Ann N Y Acad Sci 917:376–386. https://doi.org/10.1111/J.1749-6632.2000.TB05402.X
Reiter RJ, Tan DX, Rosales-Corral S et al (2018) Melatonin mitigates mitochondrial meltdown: Interactions with SIRT3. Int J Mol Sci. https://doi.org/10.3390/ijms19082439
Ribbons KA, McElduff P, Boz C et al (2015) Male sex is independently associated with faster disability accumulation in relapse-onset MS but not in primary progressive MS. PLoS ONE. https://doi.org/10.1371/journal.pone.0122686
Romero A, Ramos E, López-Muñoz F et al (2020) Coronavirus disease 2019 (COVID-19) and Its neuroinvasive capacity: is it time for melatonin? Cell Mol Neurobiol 42:489–500. https://doi.org/10.1007/s10571-020-00938-8
Roostaei T, Sahraian MA, Hajeaghaee S et al (2015) Impact of melatonin on motor, cognitive and neuroimaging indices in patients with multiple sclerosis. Iran J Allergy, Asthma Immunol 14(6):589–95
Roostaei T, Klein H-U, Ma Y et al (2021) Proximal and distal effects of genetic susceptibility to multiple sclerosis on the T cell epigenome. Nat Commun. https://doi.org/10.1038/S41467-021-27427-W
Rosales-Corral S, Acuña-Castroviejo D, Coto-Montes A et al (2012) Alzheimer’s disease: pathological mechanisms and the beneficial role of melatonin. J Pineal Res 52:167–202. https://doi.org/10.1111/J.1600-079X.2011.00937.X
Ryu JK, Kim SJ, Rah SH et al (2017) Reconstruction of LPS transfer cascade reveals structural determinants within LBP, CD14, and TLR4-MD2 for efficient LPS recognition and transfer. Immunity 46:38–50. https://doi.org/10.1016/j.immuni.2016.11.007
Sakkas GK, Giannaki CD, Karatzaferi C, Manconi M (2019) Sleep abnormalities in multiple sclerosis. Curr Treat Options Neurol 21:4. https://doi.org/10.1007/s11940-019-0544-7
Sánchez-López AL, Ortiz GG, Pacheco-Moises FP et al (2018) Efficacy of melatonin on serum pro-inflammatory cytokines and oxidative stress markers in relapsing remitting multiple sclerosis. Arch Med Res 49:391–398. https://doi.org/10.1016/j.arcmed.2018.12.004
Sandri G, Panfili E, Ernster L (1990) Hydrogen peroxide production by monoamine oxidase in isolated rat-brain mitochondria: its effect on glutathione levels and Ca2+ efflux. Biochim Biophys Acta 1035:300–305. https://doi.org/10.1016/0304-4165(90)90092-B
Sarchielli P, Zaffaroni M, Floridi A et al (2007) Production of brain-derived neurotrophic factor by mononuclear cells of patients with multiple sclerosis treated with glatiramer acetate, interferon-β 1a, and high doses of immunoglobulins. Mult Scler 13:313–331. https://doi.org/10.1177/1352458506070146
Senthil Kumaran V, Arulmathi K, Srividhya R, Kalaiselvi P (2008) Repletion of antioxidant status by EGCG and retardation of oxidative damage induced macromolecular anomalies in aged rats. Exp Gerontol 43:176–183. https://doi.org/10.1016/J.EXGER.2007.10.017
Sepúlveda M, Ros C, Martínez-Lapiscina EH et al (2016) Pituitary-ovary axis and ovarian reserve in fertile women with multiple sclerosis: a pilot study. Mult Scler 22:564–568. https://doi.org/10.1177/1352458515602339
Sezgin G, Öztürk G, Güney Ş et al (2013) Protective effect of melatonin and 1,25-dihydroxyvitamin d3 on renal ischemia-reperfusion injury in rats. Ren Fail 35:374–379. https://doi.org/10.3109/0886022X.2012.760409
Shah SA, Khan M, Jo MH et al (2017) Melatonin stimulates the SIRT1/Nrf2 signaling pathway counteracting lipopolysaccharide (LPS)-induced oxidative stress to rescue postnatal rat brain. CNS Neurosci Ther 23:33–44. https://doi.org/10.1111/cns.12588
Sharief MK, Hentges R (1991) Association between tumor Necrosis factor-α and disease progression in patients with multiple sclerosis. N Engl J Med. https://doi.org/10.1056/nejm199108153250704
Shih PH (2006) Yen GC (2006) differential expressions of antioxidant status in aging rats: the role of transcriptional factor Nrf2 and MAPK signaling pathway. Biogerontology 82(8):71–80. https://doi.org/10.1007/S10522-006-9033-Y
Sicotte NL, Giesser BS, Tandon V et al (2007) Testosterone treatment in multiple sclerosis: a pilot study. Arch Neurol 64:683–688. https://doi.org/10.1001/archneur.64.5.683
Silvagno F, Pescarmona G (2017) Spotlight on vitamin D receptor, lipid metabolism and mitochondria: some preliminary emerging issues. Mol Cell Endocrinol 450:24–31. https://doi.org/10.1016/j.mce.2017.04.013
Simon KC, Munger KL, Ascherio A (2012) Vitamin D and multiple sclerosis: epidemiology, immunology, and genetics. Curr Opin Neurol 25:246–251. https://doi.org/10.1097/WCO.0b013e3283533a7e
Şimşek Ş, Gençoǧlan S, Yüksel T et al (2016) Oxidative stress and DNA damage in untreated first-episode psychosis in adolescents. Neuropsychobiology 73:92–97. https://doi.org/10.1159/000444488
Siotto M, Filippi MM, Simonelli I et al (2019) Oxidative stress related to iron metabolism in relapsing remitting multiple sclerosis patients with low disability. Front Neurosci. https://doi.org/10.3389/fnins.2019.00086
Skarlis C, Anagnostouli M (2020) The role of melatonin in multiple sclerosis. Neurol Sci 41:769–781
Soares JL, Oliveira EM, Pontillo A (2019) Variants in NLRP3 and NLRC4 inflammasome associate with susceptibility and severity of multiple sclerosis. Mult Scler Relat Disord 29:26–34. https://doi.org/10.1016/j.msard.2019.01.023
Song C, Zhao J, Fu B et al (2017) Melatonin-mediated upregulation of Sirt3 attenuates sodium fluoride-induced hepatotoxicity by activating the MT1-PI3K/AKT-PGC-1α signaling pathway. Free Radic Biol Med 112:616–630. https://doi.org/10.1016/J.FREERADBIOMED.2017.09.005
Soto-Brambila AP, Gabriel Ortiz G, Rivero-Moragrega P et al (2017) Relapsing remitting multiple sclerosis and its relationship with the immune system and oxidative stress. Curr Immunol Rev 14:15–23. https://doi.org/10.2174/1573395514666171226154300
Spelman T, Gray O, Trojano M et al (2014) Seasonal variation of relapse rate in multiple sclerosis is latitude dependent. Ann Neurol 76:880–890. https://doi.org/10.1002/ANA.24287
Stadelmann C, Kerschensteiner M, Misgeld T et al (2002) BDNF and gp145trkB in multiple sclerosis brain lesions: neuroprotective interactions between immune and neuronal cells? Brain 125:75–85. https://doi.org/10.1093/brain/awf015
Straub RH (2007) The complex role of estrogens in inflammation. Endocr Rev 28:521–574. https://doi.org/10.1210/er.2007-0001
Sugiyama A, Kato H, Takakura H et al (2020) Effects of physical activity and melatonin on brain-derived neurotrophic factor and cytokine expression in the cerebellum of high-fat diet-fed rats. Neuropsychopharmacol Reports 40:291–296. https://doi.org/10.1002/npr2.12125
Tan DX, Hardeland R (2020) Targeting host defense system and rescuing compromised mitochondria to increase tolerance against pathogens by melatonin may impact outcome of deadly virus infection pertinent to COVID-19. Molecules 25:4410. https://doi.org/10.3390/molecules25194410
Tan DX, Xu B, Zhou X, Reiter RJ (2018) Pineal calcification, melatonin production, aging, associated health consequences and rejuvenation of the pineal gland. Mol A J Synth Chem Nat Prod Chem. https://doi.org/10.3390/MOLECULES23020301
Tasset I, Drucker-Colín R, Peña J et al (2010) Antioxidant-like effects and protective action of transcranial magnetic stimulation in depression caused by olfactory bulbectomy. Neurochem Res. https://doi.org/10.1007/s11064-010-0172-9
Tasset I, Agüera E, Olmo-Camacho R et al (2011) Melatonin improves 3-nitropropionic acid induced behavioral alterations and neurotrophic factors levels. Prog Neuro-Psychopharmacology Biol Psychiatry 35:1944–1949. https://doi.org/10.1016/j.pnpbp.2011.09.005
Tasset I, Agüera E, Sánchez-López F et al (2012) Peripheral oxidative stress in relapsing-remitting multiple sclerosis. Clin Biochem 45:440–444. https://doi.org/10.1016/J.CLINBIOCHEM.2012.01.023
Thöne J, Kollar S, Nousome D et al (2015) Serum anti-Müllerian hormone levels in reproductive-age women with relapsing-remitting multiple sclerosis. Mult Scler J 21:41–47. https://doi.org/10.1177/1352458514540843
Torrens-Mas M, Roca P, Sastre-Serra J, Margalida Torrens-Mas C (2017) Importancia de la sirtuina 3 en el estrés oxidativo y el cáncer Role of sirtuin 3 in oxidative stress and cancer. Med Balear 32:47–52. https://doi.org/10.3306/MEDICINABALEAR.32.02.47
Trachootham D, Lu W, Ogasawara MA et al (2008) Redox regulation of cell survival. Antioxid Redox Signal 10:1343. https://doi.org/10.1089/ARS.2007.1957
Túnez I, Montilla P, Muñoz MDC et al (2004) Protective effect of melatonin on 3-nitropropionic acid-induced oxidative stress in synaptosomes in an animal model of Huntington’s disease. J Pineal Res 37:252–256. https://doi.org/10.1111/j.1600-079X.2004.00163.x
Valacchi G, Virgili F, Cervellati C, Pecorelli A (2018) OxInflammation: from subclinical condition to pathological biomarker. Front Physiol 9:858. https://doi.org/10.3389/fphys.2018.00858
van den Hoogen WJ, Laman JD, Hart T, BA, (2017) Modulation of multiple sclerosis and its animal model experimental autoimmune encephalomyelitis by food and gut microbiota. Front Immunol. https://doi.org/10.3389/fimmu.2017.01081
Villanueva R (2013) Neurobiology of major depressive disorder. Neural Plast. https://doi.org/10.1155/2013/873278
Walshe JM (2005) Diagnostic significance of reduced serum caeruloplasmin concentration in neurological disease. Mov Disord. https://doi.org/10.1002/mds.20628
Wang X (2009) The antiapoptotic activity of melatonin in neurodegenerative diseases. CNS Neurosci Ther 15:345. https://doi.org/10.1111/j.1755-5949.2009.00105.x
Wang Y, Liu X, Wang W et al (2013) The expression of inflammatory cytokines on the aorta endothelia are up-regulated in pinealectomized rats. Inflammation 36:1363–1373. https://doi.org/10.1007/S10753-013-9676-1
Wang Y, Han D, Zhou T et al (2020) Melatonin ameliorates aortic valve calcification via the regulation of circular RNA CircRIC3/miR-204-5p/DPP4 signaling in valvular interstitial cells. J Pineal Res. https://doi.org/10.1111/jpi.12666
Waubant E (2018) Effect of puberty on multiple sclerosis risk and course. Mult Scler 24:32–35. https://doi.org/10.1177/1352458517737393
Wekerle H, Berer K, Krishnamoorthy G (2013) Remote control-triggering of brain autoimmune disease in the gut. Curr Opin Immunol 25:683–689. https://doi.org/10.1016/j.coi.2013.09.009
Wijnands JMA, Zhu F, Kingwell E et al (2018) Disease-modifying drugs for multiple sclerosis and infection risk: a cohort study. J Neurol Neurosurg Psychiatry. https://doi.org/10.1136/jnnp-2017-317493
Willis MD, Robertson NP (2020) Multiple sclerosis and the risk of infection: considerations in the threat of the novel coronavirus, COVID-19/SARS-CoV-2. J Neurol. https://doi.org/10.1007/s00415-020-09822-3
Wongchitrat P, Shukla M, Sharma R et al (2021) Role of melatonin on virus-induced neuropathogenesis—a concomitant therapeutic strategy to understand SARS-CoV-2 infection. Antioxidants 10:1–31. https://doi.org/10.3390/antiox10010047
Woo MMM, Tai CJ, Kang SK et al (2001) Direct action of melatonin in human granulosa-luteal cells. J Clin Endocrinol Metab 86:4789–4797. https://doi.org/10.1210/jcem.86.10.7912
Wu HHM, Xie QQM, Zhao CCC et al (2019) Melatonin biosynthesis restored by CpG oligodeoxynucleotides attenuates allergic airway inflammation via regulating NLRP3 inflammasome. Life Sci. https://doi.org/10.1016/j.lfs.2019.117067
Xu X, Wang G, Ai L et al (2018) Melatonin suppresses TLR9-triggered proinflammatory cytokine production in macrophages by inhibiting ERK1/2 and AKT activation. Sci Rep. https://doi.org/10.1038/s41598-018-34011-8
Yeganeh-Salehpour M, Mollica A, Momtaz S et al (2019) Melatonin and multiple sclerosis: from plausible neuropharmacological mechanisms of action to experimental and clinical evidence. Clin Drug Investig 39:607–624. https://doi.org/10.1007/s40261-019-00793-6
Yi S, Yang Y (2021) Melatonin attenuates low shear stress-induced pyroptosis and endothelial cell dysfunction via the RORα/miR-223/STAT-3 signalling pathway. Exp Ther Med. https://doi.org/10.3892/ETM.2021.10828
Yosefifard M, Vaezi G, Malekirad AA et al (2019) A randomized control trial study to determine the effect of melatonin on serum levels of IL-1β and TNF-α in patients with multiple sclerosis. Iran J Allergy, Asthma Immunol 18:649–654. https://doi.org/10.18502/ijaai.v18i6.2177
Yosefi-Fard M, Vaezi G, Maleki-Rad AA et al (2020) Effect of melatonin on serum levels of inf-1ß and vitamin b12 in patients with multiple sclerosis: a randomized controlled trial. Iran J Toxicol 14:19–24. https://doi.org/10.32598/ijt.14.1.19
Yu X, Rollins D, Ruhn KA et al (2013) TH17 cell differentiation is regulated by the circadian clock. Science (80-). https://doi.org/10.1126/science.1243884
Yu GM, Kubota H, Okita M, Maeda T (2017) The anti-inflammatory and antioxidant effects of melatonin on LPS-stimulated bovine mammary epithelial cells. PLoS ONE. https://doi.org/10.1371/journal.pone.0178525
Yue Y, Stone S, Lin W (2018) Role of nuclear factor κb in multiple sclerosis and experimental autoimmune encephalomyelitis. Neural Regen Res 13:1507–1515. https://doi.org/10.4103/1673-5374.237109
Zeydan B, Atkinson EJ, Weis DM et al (2020) Reproductive history and progressive multiple sclerosis risk in women. Brain Commun. https://doi.org/10.1093/braincomms/fcaa185
Zhang L, Zhang H, Liang X et al (2013) Melatonin ameliorates cognitive impairment induced by sleep deprivation in rats: role of oxidative stress, BDNF and CaMKII. Behav Brain Res 256:72–81. https://doi.org/10.1016/J.BBR.2013.07.051
Zhang R, Wang X, Ni L et al (2020) COVID-19: melatonin as a potential adjuvant treatment. Life Sci 250:117583. https://doi.org/10.1016/j.lfs.2020.117583
Zhao C, Wang P, Mao YM et al (2019) Potential role of melatonin in autoimmune diseases. Cytokine Growth Factor Rev 48:1–10. https://doi.org/10.1016/j.cytogfr.2019.07.002
Zhou W, Liu Y, Shen J et al (2019) Melatonin increases bone mass around the prostheses of OVX rats by ameliorating mitochondrial oxidative stress via the SIRT3/SOD2 signaling pathway. Oxid Med Cell Longev. https://doi.org/10.1155/2019/4019619
Zhou Y, Hou Y, Shen J et al (2020) A network medicine approach to investigation and population-based validation of disease manifestations and drug repurposing for COVID-19. PLoS Biol. https://doi.org/10.1371/journal.pbio.3000970
Acknowledgements
Not applicable.
Funding
The authors declare that no funds, grants, or other support were received during the preparation of this manuscript.
Author information
Authors and Affiliations
Contributions
AMJ: literature search, drafted the work; BME: literature search, drafted the work; JCV: literature search; AG: literature search; EA, literature search; AS: literature search; IT: idea for the article, critically revised the work.
Corresponding authors
Ethics declarations
Conflict of interest
The authors have no relevant financial or non-financial interests to disclose.
Additional information
Publisher's Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Rights and permissions
About this article
Cite this article
Muñoz-Jurado, A., Escribano, B.M., Caballero-Villarraso, J. et al. Melatonin and multiple sclerosis: antioxidant, anti-inflammatory and immunomodulator mechanism of action. Inflammopharmacol 30, 1569–1596 (2022). https://doi.org/10.1007/s10787-022-01011-0
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s10787-022-01011-0