Abstract
1,8-Cineol is a major monoterpene principally from eucalyptus essential oils and has been shown to exert anti-inflammatory, antiviral, and inhibitory of nuclear factor (NF)-kB effect. In the present study, we evaluated the effect of 1,8-cineol on mice infected with influenza A virus. We found that 1,8-cineol protects against influenza viral infection in mice. Moreover, 1,8-cineol efficiently decreased the level of IL-4, IL-5, IL-10, and MCP-1 in nasal lavage fluids and the level of IL-1β, IL-6, TNF-α, and IFN-γ in lung tissues of mice infected with influenza virus. The results also showed that 1,8-cineol reduced the expression of NF-kB p65, intercellular adhesion molecule (ICAM)-1, and vascular cell adhesion molecule (VCAM)-1 in lung tissues. Thus, 1,8-cineol appears to be able to augment protection against IFV infection in mice via attenuation of pulmonary inflammatory responses.
Similar content being viewed by others
INTRODUCTION
Influenza A viruses cause pandemic outbreaks and respiratory tract infections in animals and humans every year with high mortality and morbidity [1]. Viral pneumonia is a common complication of influenza virus (IFV) infection and leads to higher mortality. Upon IFV infection of the respiratory tract, epithelial cells and leukocytes activate transcription factors that induce both innate and adaptive immune responses, with production of cytokines and chemokines [2–4]. The excessive proinflammatory cytokines and chemokines and recruitment of innate immune cells into the lungs are hallmarks of influenza virus infection [5]. Current therapeutic strategies for influenza include M2 ion channel inhibitors (e.g., amantadine and rimantadine) [6, 7], neuraminidase (NA) inhibitors (e.g., oseltamivir and zanamivir) [8], and RNA polymerase inhibitors (e.g., ribavirin) [8]. However, the emergence of influenza virus strains resistant to these antivirals has become a global health concern [9]. Modulation of the host proinflammatory response might thus represent a complementary therapeutic strategy, with an advantage over antivirals in terms of avoiding the emergence of drug-resistant variants [10].
1,8-Cineol (eucalyptol, C10H18O), the chemical structure of which is shown in Fig. 1, a major monoterpene principally from eucalyptus essential oils [11], is traditionally used to treat upper and lower airway diseases, such as chronic sinusitis, bronchitis, chronic obstructive pulmonary disease, and bronchial asthma [12–14]. Research has demonstrated that 1,8-cineol has a variety of pharmacological activities, including antiviral [15], anti-inflammatory [16], antinociceptive [16], and antimicrobial [17, 18] actions.
Notably, 1,8-cineol has been paid more attention due to its anti-inflammatory activity and inhibition of nuclear factor (NF)-kB. 1,8-cineol has been identified as an active substance with anti-inflammatory and antioxidant properties [19, 20]. 1,8-cineol strongly inhibits tumor necrosis factor (TNF)-α and IL-1β level [12, 21]. Likewise, 1,8-cineol is also known to inhibit directly signaling via NF-kB [22]. Previous studies have shown that proinflammatory cytokines are markedly elevated during influenza virus infection, and this “cytokine storm” is hypothesized to be the main cause of mortality [23, 24]. NF-kB is the main regulator of cytokine and chemokine production in influenza [2, 25]. Inhibitors of NF-kB can block virus replication as well as inhibiting host inflammatory responses [26]. The ability of 1,8-cineol to inhibit cytokine production and NF-kB led to the hypothesis that 1,8-cineol could be a therapy against pulmonary inflammation caused by influenza virus infection.
In the present study, we evaluated the effect of 1,8-cineol on mice infected with influenza H1N1 (A/FM/1/47). The effects of 1, 8-cineol on the expression of NF-kB, intercellular adhesion molecule (ICAM)-1, and vascular cell adhesion molecule (VCAM)-1 in lungs and the levels of proinflammatory cytokines in nasal lavage fluids and lung were also investigated in IFV-infected mice.
MATERIALS AND METHODS
Animals and Virus
Specific-pathogen-free (SPF), 8-week-old female BALB/c mice (Medical Experiment Center of Guangdong Province, Guangzhou, China) were used after 24 h quarantine and were fed standard mouse chow and tap water ad libitum for the duration of the studies. The study was approved by the Animal Care and Use Committee of the Guangzhou University of Chinese Medicine (Guangzhou, China). Humane endpoints are chosen in the experimental animals (e.g., survival study) via euthanasia and use of anesthesia.
The strain of influenza virus, A/Font Monmouth/47(H1N1, FM1), mouse adapted, was originally obtained from Chinese Center for Disease Control and Prevention (CDC). The virus was adapted to replication in the lungs of BALB/c mice by eight sequential passages through mouse lungs. The received virus had been plaque purified in MDCK cells followed by replication in 9-day-old chicken embryos and then in MDCK cells. The virus pool was pretitrated in mice prior to performing these studies to determine an appropriate challenge dose.
Compounds
1,8-Cineol was acquired from Shanghai yuanye Bio-Technology Co., Ltd. (Shanghai, China; Purity ≥99 % by high-performance liquid chromatography (HPLC); Lot: Y16D5S1) and diluted with sterile saline (suspended in 0.5 % Tween 80) to the desired concentrations. Oseltamivir was purchased as Tamiflu capsules from Hoffmann-La Roche Ltd. (Basel, Switzerland; Lot: B3014) and diluted with sterile saline.
Murine Model of Influenza Infection
Mice were randomly divided into 6 groups of 10: negative control group (NC); IFV control group (IFV-C + sterile saline, suspended in 0.5 % Tween 80); 1, 8-cineol groups (H1N1 virus + 1,8-cineol 30, 60, and 120 mg/kg); and positive control oseltamivir (10 mg/kg). The dose of influenza virus used to induce infection was performed as described previously [27]. The challenge inoculation of approximately 105.0 cell culture infectious doses (CCID50)/mouse equated to five 50 % mouse lethal challenge doses (MLD50). Mice (excluding NC group) were infected intranasally with 50 μL of 15 MLD50 of influenza virus in sterile phosphate-buffered saline (PBS), pH 7.2 under light anesthesia. BALB/c mice were treated by oral gavage with 1, 8-cineol (30, 60, and 120 mg/kg) or oseltamivir (10 mg/kg) for 2 days before viral challenge and received concomitant treatment for 5 days after infection. On day 6 post-infection, 10 mice per group were sacrificed to collect related samples, measure body weight and lung wet weight, and detect the viral load, cytokine, pathological changes, ICAM-1, VCAM-1, and NF-kB expression in the lungs.
Survival Experiments
Mice were anesthetized in a chamber containing absorbent cotton saturated with 30-ml diethyl ether for about 30 s and infected intranasally with 5 MLD50 of influenza virus in sterile PBS (pre-cooled). BALB/c mice were treated with 1,8-cineol or oseltamivir (oral administration) for 2 days before infection. Mice received concomitant these treatment after infection for 5 days and were monitored daily for 15 days post-infection. For the IFV-C group, the mice were only given saline (0.5 % Tween 80) at the same intervals. Mice were observed continuously daily for weight loss, survival, and clinical symptoms of illness (e.g., ruffled fur, inactivity, poor appetite, hunched posture, and rapid shallow breathing) for 15 days after infection to assess the survival rate.
Lung Index
The severity of pulmonary edema was assessed by lung index. Mouse body weight was measured, and the lungs were removed and washed. The lung index was calculated following lung weight/body weight ratio’s multiplication by 100 %.
Lung Pathology
The lungs of mice were fixed in 10 % PBS-buffered formaldehyde, dehydrated in graded ethanol, and embedded in low-melting point paraffin. Five-micrometer pieces were sectioned and stained with HE and then examined under microscopy in a double-blinded manner. Lung injury score were assigned between 0 (normal) and 4 (severe) based on the following criteria: necrotic bronchiolar and bronchial epithelium’s presence; serocellular exudates in the bronchiolar and bronchial lumina; inflammatory cells (predominantly lymphocytes and neutrophils) in the bronchiolar, peribronchiolar and alveolar interstitium; alveolar or peribronchiolar collapse (atelectasis); and diffuse or multifocal interstitial edema. A score of 0 represented no damage, 1 mild damage, 2 moderate damage, 3 severe damage, and 4 very severe histological changes [28].
Viral Load Analysis
The viral load in the lungs was determined as previously described [27]. The lungs were homogenized and centrifuged at 4000×g for 15 min at 4 °C. Total RNA was extracted using the RNeasy kit (Invitrogen, Carlsbad, CA, USA). Total RNA was reverse transcribed into cDNA using the RevertAid First Strand cDNA Synthesis Kit (MBI Fermentas, Vilnius, Lithuania) according to the protocol of the manufacturer. The primer sequences for influenza A virus (A/Font Monmouth/1/47), which were designed by Primer-BLAST from NCBI, for quantitative polymerase chain reaction (qPCR) of the IFV M gene were the following: forward 5′-AATGGTGCAGGCGATGAGAG-3′ and reverse 5′-TACTTGCGGCAACAACGAGAG-3′. GAPDH primers were used as internal controls of cellular RNAs: forward 5′-CCTCGTCCCGTAGACAAAATG-3′ and reverse 5′-TGAGGTCAATGAAGGGGTCG-3′. Quantitative reverse transcriptase PCR (qRT-PCR) was conducted using a Platinum SYBR Green qPCR SuperMix-UDG kit (Invitrogen) in an ABI StepOne qPCR machine (Applied Biosystems, Foster city, CA, USA) with the following parameters: 95 °C for 2 min, followed by 40 cycles of 95 °C for 15 s, 62.5 °C for 30 s, and 72 °C for 30 s. Each sample was analyzed three times. The IFV quantity of PCR products was analyzed according to the mode for normalized expression (2−ΔΔct). ΔΔct was calculated as follows: ΔΔct=Δct (target gene) − Δct (reference gene) [29]. Relative quantities of IFV load in the lungs in the experimental groups compared to the NC group were calculated after the NC group was normalized to 1.
Cytokine in Lung Homogenate in Mice Infected with IFV
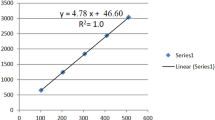
The mice were euthanized by exsanguination, and the lungs were removed, homogenized, and centrifuged at 4000×g for 15 min at 4 °C. The supernatants of the lung homogenates were stored at −80 °C for subsequent analysis of cytokine levels. IL-6, TNF-α, IL-1β, and IFN-γ concentrations from lung homogenates were measured using commercially available mouse IL-6, TNF-α, IL-1β, and IFN-γ ELISA Kit (Multisciences Biotech, Hangzhou, China) according to the manufacturer’s instructions. Briefly, samples were tested at 1:2 dilutions and biotinylated IL-6, TNF-α, IL-1β, and IFN-γ antibodies were respectively applied into 96-well plates pre-coated with monoclonal anti-mouse IL-6, TNF-α, IL-1β, and anti-mouse IFN-γ antibodies. The samples were incubated for 90 min at room temperature, 90 min at 37 °C, and 2 h at room temperature. After washing four times, streptavidin–HRP working solution was added and incubated for 30 min at room temperature. TMB was added and incubated for 30 min at room temperature and in the dark after washing. The reaction was stopped with a stop solution, and OD450 was read immediately by an ELISA plate reader (Bio-Tek ELx800, Vermont, USA). Purified mouse IL-6, TNF-α, IL-1β, and IFN-γ (standard) were used to create a standard curve for the determination of IL-6, TNF-α, IL-1β, and IFN-γ.
Cytokine in Nasal Lavage Fluids in Mice Infected with IFV
For collection of nasal lavage fluids, mice were killed, the skin was removed from the head, and the lower jaw was cut away. Lavage was performed by introducing a 12-gauge, blunt-ended, intragastric syringe needle into the nasal cavity and washing the mucosa with 1-ml sterile PBS. The nasal lavage fluids were centrifuged for 15 min at 4000×g and stored at −80 °C before cytokine assay. Levels of MCP-1, IL-4, IL-5, and IL-8 in the cell-free nasal lavage fluids were evaluated using ELISA (Multisciences Biotech, Hangzhou, China). Briefly, samples were tested at 1:2 dilutions and biotinylated anti-MCP-1, IL-10, IL-4, and anti-IL-5 antibodies were respectively applied into 96-well plates pre-coated with monoclonal anti-mouse MCP-1, anti-mouse IL-10, anti-mouse IL-4, and anti-mouse IL-5 antibodies. The samples were incubated for 90 min at room temperature, 90 min at 37 °C, and 2 h at room temperature, respectively. After washing four times, streptavidin-HRP working solution was added and incubated for 30 min at room temperature. Tetramethylben-zidine was added and incubated for 30 min at room temperature and in the dark after washing. The reaction was stopped with a stop solution, and absorbance was read immediately at 450 nm by an ELISA plate reader (Bio-Tek ELx800, Vermont, USA).
ICAM-1, VCAM-1, and NF-kB p65 Expression in the Lung
Whole lung tissues were homogenized in radio-immunoprecipitation assay (RIPA) buffer (Exon Biotechnology Inc, Guangzhou, China) and lysed in SDS-PAGE sample buffer, boiled, centrifuged and the supernatant recovered. The homogenate was centrifuged at 12,000×g for 5 min at 4 °C. Protein was quantified with a BCA Protein Assay Kit (Exon Biotechnology Inc, Guangzhou, China). The protein samples (20 mg) were separated by 10 % SDS-PAGE and transferred to polyvinylidene fluoride (PVDF) membranes (Exon Biotechnology Inc, Guangzhou, China). The membranes were soaked in methanol for 1–2 min. Immunoblotting was assayed using anti-NF-kB p65(1:200), anti-ICAM-1 (1:200) and anti-VCAM-1 (1:300) antibodies (Santa Cruz Biotech, Santa Cruz, CA, USA), or anti-GAPDH antibody (1:5000; Santa Cruz Biotech, Santa Cruz, CA, USA) overnight. The secondary antibody (horseradish-peroxidase-conjugated goat anti-rabbit immunoglobulin, 1:5000, Abcam, Cambridge, UK) was added and incubated at room temperature for 1 h. The immunodetection was done using a chemiluminescence detection kit (Guangdong Yuehua Medical Instrument Factory Co., Shantou, China). The relative protein level was normalized to GAPDH. The bands density was quantified using the Gel analysis software (GelPro5.0, Media Cybernetics, Bethesda, MD, USA) via calculating the average optical density in each field.
Statistical Analysis
All data were expressed as means ± SD, and statistical analysis was performed with the PASW for Windows, version 18.0 (SPSS, Chicago, IL, USA). Multiple group comparisons were performed using one-way analysis of variance followed by least significant difference test to detect inter-group differences. Analysis of variance (ANOVA) followed by Tukey’s multiple comparison tests was used. P < 0.05 was considered to be statistically significant. Kruskal-Wallis test was used in the lung injury score. For survival studies, a log-rank (Mantel-Cox) test was used.
RESULTS
1,8-Cineol Treatment Protected Mice from Influenza Challenge
The protective efficacy of 1, 8-cineol in IFV-infected mice was evaluated. The infected mice exhibited clinical symptoms on day 3 post-inoculation with IFV. By day 6, more severe clinical signs of infected mice were present, including inactivity, ruffled fur, poor appetite, rapid shallow breathing, and weight loss.
1,8-Cineol or oseltamivir can relieve the clinical signs in mice. The infected mice began to die from day 4 post-inoculation, reaching a plateau on day 9 (Fig. 2b). The body weight of the infected mice was significantly decreased on days 3–9 post-inoculation compared with the NC group (Fig. 2a). However, survival rates and body weight were higher in the oseltamivir-treated mice and in the 1,8-cineol (60 and 120 mg/kg)-treated mice than those in the IFV-C group. Mice in the IFV-C group did not survive beyond 15 days after infection. The average survival time of mice in the IFV-C group was 5 days. 1,8-cineol treatment (30, 60, and 120 mg/kg) significantly prolonged the survival time of mice after infection (Fig. 2b-c). Therefore, inhibition of the mortality rate and body weight loss, or maximizing survival time, was observed in 1,8-cineol- and oseltamivir-treated mice. None of the mice in the NC group showed any clinical signs or died, and their body mass increased over the course of the experiment. This indicates that 1,8-cineol can protect mice from influenza virus challenge.
1,8-Cineol treatment protected mice from influenza challenge. BALB/c mice (n = 10) were treated for 2 days before viral challenge and 6 days after infection and monitored daily for signs and symptoms, body weight loss, and survival for 15 consecutive days. a Body weight; b survival rate; c survival time. Values are mean ± SD. Asterisks denote the significance levels: one asterisk p < 0.05, two asterisks p < 0.01, and three asterisks p < 0.001, compared with IFV-C group.
1,8-Cineol Attenuated Pulmonary Inflammation in Mice
To assess the pathological changes, HE staining and lung injury score were studied. On day 6 post-inoculation, lung lesions in infected mice were characterized by inflammatory cellular infiltrate, peribronchiolitis with edema and inflammatory cellular infiltrate around the bronchioles, and interstitial edema around the small blood vessels (Fig. 3a-IFV-C). However, after 1,8-cineol treatment, the pathological changes in the lung tissues were relieved. Mice in the NC group showed no histological changes. Lung histopathology score of virus-infected mice treated with 1,8-cineol (30–120 mg/kg) was lower compared with that of the IFV-C group (Fig. 3b). In the IFV-C group, lung index was significantly increased compared with that in the NC group on day 6 post-infection (p < 0.01). Nevertheless, lung index significantly decreased after 1,8-cineol administration (Fig. 3c). Oseltamivir had a similar effect on lung index decrease. Treatment with 1,8-cineol (30–120 mg/kg) significantly suppressed the mRNA expression of influenza virus M gene, as compared to the IFV-C group (Fig. 3d). This indicates that 1,8-cineol alleviates the inflammatory effect of influenza virus.
1,8-Cineol alleviated the severity of HIN1-induced lung injuries at day 6 post-infection (n = 6–10). a Pathological changes of lung tissues (HE, ×100); b pathological scores; c lung index; d relative quantitation of influenza A virus in the lung. Data were presented as mean ± SD. Asterisks denote the significance levels: one asterisk p < 0.05, two asterisks p < 0.01, and three asterisks p < 0.001, compared with IFV-C group.
Influence of 1,8-Cineol on Cytokine and Chemokine Production in Nasal Lavage Fluids
IL-4, IL-5, IL-10, and MCP-1 in nasal lavage fluids were measured by ELISA. Mice in the NC group produced low levels of all basal cytokines/chemokines tested. IL-4, IL-5, IL-10, and MCP-1 in nasal lavage fluids in the mice with H1N1 influenza virus infection were markedly higher on day 5 post-inoculation than in the NC group. Influenza virus-induced cytokine secretion was reduced by 1,8-cineol. Similar to 1,8-cineol, oseltamivir also decreased influenza virus-induced cytokine secretion (Fig. 4).
1,8-Cineol suppressed the production of inflammatory cytokines in nasal lavage fluids (n = 10). On days 6 after infection, mice were euthanized and proinflammatory cytokine and chemokine levels were analyzed in nasal washes by ELISA. Data were presented as mean ± SD. Asterisks denote the significance levels: one asterisk p < 0.05, two asterisks p < 0.01, and three asterisks p < 0.001, compared with IFV-C group.
1,8-Cineol Inhibited Influenza Virus-Induced Changes in Cytokine Levels in Lung Homogenates
Elevation of proinflammatory cytokines is a typical response to influenza virus infection, so we established if 1,8-cineol affected virus-induced release of proinflammatory cytokines.
Lung tissues were harvested from the mice after influenza virus infection, and cytokines (IL-1β, IL-6, TNF-α, and IFN-γ) were analyzed. The levels of IL-1β, IL-6, TNF-α, and IFN-γ in lung homogenate were significantly increased 5 days post-infection, compared with those of the NC group (Fig. 5). However, 1,8-cineol (60–120 mg/kg) significantly attenuated the increases in IL-1β, IL-6, TNF-α, and IFN-γ levels in lung homogenates. The effect of oseltamivir on IL-1β, IL-6, TNF-α, and IFN-γ levels was similar to that of 1,8-cineol. 1,8-Cineol significantly decreased influenza virus-induced cytokine levels in lung homogenates.
Effects of 1,8-cineol on cytokine in lung homogenate in mice infected with IFV (n = 10). Proinflammatory cytokine levels were analyzed in lung homogenates of mice on day 6 after infection by ELISA. Data were presented as mean ± SD. Asterisks denote the significance levels: one asterisk p < 0.05, two asterisks p < 0.01, and three asterisks p < 0.001, compared with IFV-C group. a The level of TNF-alpha in lung homogenate, b the level of INF-gamma in lung homogenate, c the level of IL-1beta in lung homogenate, d the level of IL-6 in lung homogenate.
1,8-Cineol Inhibited Influenza Virus-Induced ICAM-1, VCAM-1, and NF-kB Expression in the Lungs
To study the mechanism of the anti-inflammatory effect of 1,8-cineol, ICAM-1, VCAM-1, and NF-kB expression in lung tissues was analyzed by western blotting. Influenza virus significantly increased ICAM-1, VCAM-1, and NF-kB p65 expression (Fig. 6a). 1,8-Cineol significantly inhibited the increases in ICAM-1, VCAM-1, and NF-kB p65 expression (Fig. 6b–d). Oseltamivir markedly inhibited ICAM-1, VCAM-1, and NF-kB expression.
1,8-Cineol inhibited lung NF-kB, ICAM-1, and VCAM-1 expression in mice infected with IFV by Western blot analysis (n = 6). GAPDH protein was used as a loading control. a Representative page of NF-kB, ICAM-1, and VCAM-1 expression by Western blotting. b Semi-quantitative analysis of NF-kB protein. c Semi-quantitative analysis of ICAM-1 protein. d Semi-quantitative analysis of VCAM-1 protein. Values are mean ± SD. Asterisks denote the significance levels: one asterisk p < 0.05, two asterisks p < 0.01, three asterisks p < 0.001, compared with IFV-C group.
DISCUSSION
Influenza virus frequently causes annual epidemics and sometimes even pandemic outbreaks [30]. The virus normally infects the upper and lower respiratory tract and leads to severe pneumonia, acute respiratory distress syndrome, and often to death in humans [31]. A/Font Monmouth/1/47 is a mouse-adapted influenza virus with high virulence, which can induce strong immune responses and life-threatening pneumonia [32]. In the present study, the effect of 1,8-cineol on the mice infected with influenza A virus was evaluated. The present study clearly demonstrated that 1,8-cineol significantly relieved the signs and symptoms, reduced body weight loss, and improved the survival rate of H1N1-infected mice. Furthermore, lung lesions, a life-threatening complication, can also be alleviated by 1,8-cineol. Altogether, these results suggested that 1,8-cineol had potent protection against H1N1 influenza A virus infection in mice. Therefore, we speculated that the protective effect of 1,8-cineol on mice infected with IFV was accomplished by inhibiting the early recruitment of inflammatory leukocytes to the lungs and suppressing excessive innate inflammatory responses.
Influenza virus pneumonia is characterized by progressively inflammation and diffuse bilateral pulmonary edema, reduced pulmonary compliance, and hypoxemia [33, 34]. After influenza A virus infection, cytokines are released by activated neutrophils and macrophages, leading to increased alveolocapillary membrane permeability. Inflammatory cell infiltration is induced by influenza virus into lung tissues, causing the release of proinflammatory cytokines such as IL-1β, chemotactic factors and TNF-α [3, 4]. These changes cause lung edema, alveolar hemorrhage, and overwhelming inflammation [35]. In the present study, we found that 1,8-cineol attenuated influenza virus-induced lung inflammation. The lower histopathology scores of the lungs in cineol-treated mice revealed that 1,8-cineol might alleviate the development of pulmonary edema.
Previous studies have shown that MCP-1, IP-10, RANTES, T cell activation gene 3, and macrophage inflammatory protein (MIP)-2 mRNA expression in the lungs are elevated at day 3 after influenza virus infection [36, 37]. Protein expression of MIP-1α, MIP-1β, and MCP-1 increases in nasal lavage fluids in response to infection [3, 4, 38]. 1,8-Cineol was reported to suppress inflammatory response in tissues and cells by inhibiting proinflammatory cytokine production previously, such as TNF-α and IL-1β [21, 39]. 1,8-Cineol can significantly reduce the leukocyte number in bronchoalveolar lavage fluid, including neutrophils and macrophages [40]. According to our data, IL-4, IL-5, IL-10, and MCP-1 in nasal lavage fluids and IL-1β, IL-6, TNF-α, and IFN-γ in lung tissue were noticeably raised by influenza virus infection. Meanwhile, 1,8-cineol reduced the upregulated proinflammatory cytokines in nasal lavage fluids and lung tissue. In present study, oral administration of 1,8-cineol (30–120 mg/kg) significantly decreased TNF-α level. TNF-α, a proinflammatory cytokine produced by the innate immune system’s cells following viral infection, has a significant role in priming epithelial cells for higher cytokine and chemokine production in influenza A viral infection [41]. Our findings confirm that the protective effect of 1,8-cineol on mice infected with IFV may be attributed to the inhibition of pulmonary inflammatory responses.
Adhesion molecules, such as VCAM-1 and ICAM-1, are expressed on bronchial microvessels and participate in accumulation and leukocyte recruitment [42]. ICAM-1 and VCAM-1 expression were upregulated on the surface of alveolar endothelial cells upon influenza A virus infection [43]. The decrease in ICAM-1 and VCAM-1 on the cell surface can reduce the susceptibility to and severity of infection [44]. In our current study, analyses of cellular adhesion molecule expression on mouse lungs in response to H1N1 virus infection revealed upregulation of ICAM-1 and VCAM-1, which were subsequently inhibited by 1,8-cineol. This indicates that 1,8-cineol is effective in decreasing the adhesion molecules expressed, to protect the host from continual viral infection.
Influenza virus infection leads to the activation of a variety of intracellular signaling pathways that are in part exploited by the virus to support efficient replication. Activation of NF-kB is one of the hallmarks of host cell response to invasion by influenza virus [45]. NF-kB is the main regulator of cytokine and chemokine production in influenza [45, 46]. Influenza virus infection initiates transcription of a variety of genes for cytokines such as TNF-α, TNF-β, IL-lα, IL-1β, IL-2, IL-4, IL-6, IL-10, ICAM-1, and IFN-γ [47]. Overexpression of cytokines and chemokines induced by influenza virus infection is dependent on the NF-kB signaling pathway [47, 48]. Previous study showed that 1,8-cineol can inhibit nuclear translocation of NF-kappaB p65 and NF-kappaB-dependent transcriptional activity [20, 22, 49]. In present study, compared with the IFV-C group, the expression of NF-kB p65 (the major component of NF-kB) was significantly decreased in the lung after influenza virus challenge in cineol-treated mice.
The exact mechanisms of 1,8-cineol activity in influenza infection require further clarification. One possibility is that the inhibition of signaling via NF-kB. NF-kB activation not only is a hallmark of the host cell response to invasion by influenza virus, but is the main regulator of cytokine and chemokine production in influenza [45]. During replication, the influenza virus activates the Raf/MEK/ERK-cascade and the transcription factor NF-kB. This results in both virus supportive and antiviral effects by promoting viral genome transport for virus assembly and by inducing expression of proinflammatory host factors [50]. 1,8-Cineol treatment might interfere with this chain of events by inhibiting signaling via NF-kB during influenza infection, suppressing virus production and inflammatory responses.
To summarize, our study supports new evidence that 1,8-cineol blocks cytokine production and inhibits viral pneumonia in mice infected with influenza A virus. However, the underlying mechanism of action of 1,8-cineol still needs to be investigated in other subtypes and strains of influenza virus. As combination therapy with anti-inflammatory drugs and antiviral drugs has become an important research topic [51], the combination of an anti-inflammatory agent and NF-kB inhibitor, 1,8-cineol, with an antiviral, e.g., oseltamivir, may have a synergistic effect against influenza virus infection. Further study using mice models will be needed to characterize the effectiveness of the combination therapy on influenza virus-induced pneumonia. In addition, This potential role of 1,8-cineol in patients with pneumonia caused by influenza virus needs to be further investigated in clinical studies.
ALI, acute lung injury; HE, hematoxylin and eosin; ICAM, intercellular adhesion molecule; IFV, influenza virus; IFV-C, influenza virus control; IL, interleukin; MCP, monocyte chemotactic protein; MIP, macrophage inflammatory protein; MLD50, 50 % mouse lethal challenge doses; NC, negative control; NF, nuclear factor; TNF, tumor necrosis factor; VCAM, vascular cell adhesion molecule
References
Mummert, A., H. Weiss, L.P. Long, J.M. Amigo, and X.F. Wan. 2013. A perspective on multiple waves of influenza pandemics. PLoS One 8: e60343.
Droebner, K., S.J. Reiling, and O. Planz. 2008. Role of hypercytokinemia in NF-kappaB p50-deficient mice after H5N1 influenza A virus infection. Journal of Virology 82: 11461–11466.
Julkunen, I., K. Melen, M. Nyqvist, J. Pirhonen, T. Sareneva, and S. Matikainen. 2000. Inflammatory responses in influenza A virus infection. Vaccine 19(Suppl 1): S32–37.
Matikainen, S., J. Siren, J. Tissari, V. Veckman, J. Pirhonen, M. Severa, et al. 2006. Tumor necrosis factor alpha enhances influenza A virus-induced expression of antiviral cytokines by activating RIG-I gene expression. Journal of Virology 80: 3515–3522.
La Gruta, N.L., K. Kedzierska, J. Stambas, and P.C. Doherty. 2007. A question of self-preservation: immunopathology in influenza virus infection. Immunology and Cell Biology 85: 85–92.
Belshe, R.B., M.H. Smith, C.B. Hall, R. Betts, and A.J. Hay. 1988. Genetic basis of resistance to rimantadine emerging during treatment of influenza virus infection. Journal of Virology 62: 1508–1512.
Wang, C., K. Takeuchi, L.H. Pinto, and R.A. Lamb. 1993. Ion channel activity of influenza A virus M2 protein: characterization of the amantadine block. Journal of Virology 67: 5585–5594.
De Clercq, E. 2006. Antiviral agents active against influenza A viruses. Nature Reviews Drug Discovery 5: 1015–1025.
Choi, W.Y., S. Kim, N. Lee, M. Kwon, I. Yang, M.J. Kim, et al. 2009. Amantadine-resistant influenza A viruses isolated in South Korea from 2003 to 2009. Antiviral Research 84: 199–202.
Dunning, J., J.K. Baillie, B. Cao, and F.G. Hayden. 2014. Antiviral combinations for severe influenza. Lancet Infectious Diseases 14: 1259–1270.
Ait-Ouazzou, A., S. Loran, M. Bakkali, A. Laglaoui, C. Rota, A. Herrera, et al. 2011. Chemical composition and antimicrobial activity of essential oils of Thymus algeriensis, Eucalyptus globulus and Rosmarinus officinalis from Morocco. Journal of the Science of Food and Agriculture 91: 2643–2651.
Juergens, U.R., U. Dethlefsen, G. Steinkamp, A. Gillissen, R. Repges, and H. Vetter. 2003. Anti-inflammatory activity of 1.8-cineol (eucalyptol) in bronchial asthma: a double-blind placebo-controlled trial. Respiratory Medicine 97: 250–256.
Zhou, J.Y., X.F. Wang, F.D. Tang, G.H. Lu, Y. Wang, and R.L. Bian. 2007. Inhibitory effect of 1,8-cineol (eucalyptol) on Egr-1 expression in lipopolysaccharide-stimulated THP-1 cells. Acta Pharmacologica Sinica 28: 908–912.
Worth, H., C. Schacher, and U. Dethlefsen. 2009. Concomitant therapy with Cineole (Eucalyptole) reduces exacerbations in COPD: a placebo-controlled double-blind trial. Respiratory Research 10: 69.
Santos, F.A., R.M. Silva, A.R. Campos, R.P. De Araujo, R.C. Lima Junior, and V.S. Rao. 2004. 1,8-cineole (eucalyptol), a monoterpene oxide attenuates the colonic damage in rats on acute TNBS-colitis. Food and Chemical Toxicology 42: 579–584.
Santos, F.A., and V.S. Rao. 2000. Antiinflammatory and antinociceptive effects of 1,8-cineole a terpenoid oxide present in many plant essential oils. Phytotherapy Research 14: 240–244.
Mulyaningsih, S., F. Sporer, J. Reichling, and M. Wink. 2011. Antibacterial activity of essential oils from Eucalyptus and of selected components against multidrug-resistant bacterial pathogens. Pharmaceutical Biology 49: 893–899.
Djenane, D., J. Yanguela, T. Amrouche, S. Boubrit, N. Boussad, and P. Roncales. 2011. Chemical composition and antimicrobial effects of essential oils of Eucalyptus globulus, Myrtus communis and Satureja hortensis against Escherichia coli O157:H7 and Staphylococcus aureus in minced beef. Food Science and Technology International 17: 505–515.
Cho, K.H. 2012. 1,8-cineole protected human lipoproteins from modification by oxidation and glycation and exhibited serum lipid-lowering and anti-inflammatory activity in zebrafish. BMB Reports 45: 565–570.
Lima, P.R., T.S. de Melo, K.M. Carvalho, I.B. de Oliveira, B.R. Arruda, G.A. de Castro Brito, et al. 2013. 1,8-cineole (eucalyptol) ameliorates cerulein-induced acute pancreatitis via modulation of cytokines, oxidative stress and NF-kappaB activity in mice. Life Sciences 92: 1195–1201.
Juergens, U.R., M. Stober, and H. Vetter. 1998. Inhibition of cytokine production and arachidonic acid metabolism by eucalyptol (1.8-cineole) in human blood monocytes in vitro. European Journal of Medical Research 3: 508–510.
Greiner, J.F., J. Muller, M.T. Zeuner, S. Hauser, T. Seidel, C. Klenke, et al. 1833. 1,8-cineol inhibits nuclear translocation of NF-kappaB p65 and NF-kappaB-dependent transcriptional activity. Biochimica et Biophysica Acta 2013: 2866–2878.
Chan, M.C., C.Y. Cheung, W.H. Chui, S.W. Tsao, J.M. Nicholls, Y.O. Chan, et al. 2005. Proinflammatory cytokine responses induced by influenza A (H5N1) viruses in primary human alveolar and bronchial epithelial cells. Respiratory Research 6: 135.
de Jong, M.D., C.P. Simmons, T.T. Thanh, V.M. Hien, G.J. Smith, T.N. Chau, et al. 2006. Fatal outcome of human influenza A (H5N1) is associated with high viral load and hypercytokinemia. Nature Medicine 12: 1203–1207.
Schmolke, M., D. Viemann, J. Roth, and S. Ludwig. 2009. Essential impact of NF-kappaB signaling on the H5N1 influenza A virus-induced transcriptome. Journal of Immunology 183: 5180–5189.
Peiris, J.S., K.P. Hui, and H.L. Yen. 2010. Host response to influenza virus: protection versus immunopathology. Current Opinion in Immunology 22: 475–481.
Li, Y.C., S.Z. Peng, H.M. Chen, F.X. Zhang, P.P. Xu, J.H. Xie, et al. 2012. Oral administration of patchouli alcohol isolated from Pogostemonis Herba augments protection against influenza viral infection in mice. International Immunopharmacology 12: 294–301.
Parsey, M.V., R.M. Tuder, and E. Abraham. 1998. Neutrophils are major contributors to intraparenchymal lung IL-1 beta expression after hemorrhage and endotoxemia. Journal of Immunology 160: 1007–1013.
Livak, K.J., and T.D. Schmittgen. 2001. Analysis of relative gene expression data using real-time quantitative PCR and the 2(-Delta Delta C(T)) Method. Methods 25: 402–408.
Yoon, S.W., R.J. Webby, and R.G. Webster. 2014. Evolution and ecology of influenza A viruses. Current Topics in Microbiology and Immunology 385: 359–375.
Clemans, D.L., R.J. Bauer, J.A. Hanson, M.V. Hobbs, J.W. St Geme 3rd, C.F. Marrs, et al. 2000. Induction of proinflammatory cytokines from human respiratory epithelial cells after stimulation by nontypeable Haemophilus influenzae. Infection and Immunity 68: 4430–4440.
Xu, L., L. Bao, F. Li, Q. Lv, Y. Ma, J. Zhou, et al. 2011. Adaption of seasonal H1N1 influenza virus in mice. PLoS One 6, e28901.
Xu, T., J. Qiao, L. Zhao, G. Wang, G. He, K. Li, et al. 2006. Acute respiratory distress syndrome induced by avian influenza A (H5N1) virus in mice. American Journal of Respiratory and Critical Care Medicine 174: 1011–1017.
Morty, R.E., O. Eickelberg, and W. Seeger. 2007. Alveolar fluid clearance in acute lung injury: what have we learned from animal models and clinical studies? Intensive Care Medicine 33: 1229–1240.
Yuan, X., Y. Wang, D. Du, Z. Hu, M. Xu, and Z. Liu. 2012. The effects of the combination of sodium ferulate and oxymatrine on lipopolysaccharide-induced acute lung injury in mice. Inflammation 35: 1161–1168.
Kaufmann, A., R. Salentin, R.G. Meyer, D. Bussfeld, C. Pauligk, H. Fesq, et al. 2001. Defense against influenza A virus infection: essential role of the chemokine system. Immunobiology 204: 603–613.
Dawson, T.C., M.A. Beck, W.A. Kuziel, F. Henderson, and N. Maeda. 2000. Contrasting effects of CCR5 and CCR2 deficiency in the pulmonary inflammatory response to influenza A virus. American Journal of Pathology 156: 1951–1959.
Fritz, R.S., F.G. Hayden, D.P. Calfee, L.M. Cass, A.W. Peng, W.G. Alvord, et al. 1999. Nasal cytokine and chemokine responses in experimental influenza A virus infection: results of a placebo-controlled trial of intravenous zanamivir treatment. Journal of Infectious Diseases 180: 586–593.
Juergens, U.R., T. Engelen, K. Racke, M. Stober, A. Gillissen, and H. Vetter. 2004. Inhibitory activity of 1,8-cineol (eucalyptol) on cytokine production in cultured human lymphocytes and monocytes. Pulmonary Pharmacology & Therapeutics 17: 281–287.
Zhao, C., J. Sun, C. Fang, and F. Tang. 2014. 1,8-cineol attenuates LPS-induced acute pulmonary inflammation in mice. Inflammation 37: 566–572.
Veckman, V., P. Osterlund, R. Fagerlund, K. Melen, S. Matikainen, and I. Julkunen. 2006. TNF-alpha and IFN-alpha enhance influenza-A-virus-induced chemokine gene expression in human A549 lung epithelial cells. Virology 345: 96–104.
Tosi, M.F., J.M. Stark, C.W. Smith, A. Hamedani, D.C. Gruenert, and M.D. Infeld. 1992. Induction of ICAM-1 expression on human airway epithelial cells by inflammatory cytokines: effects on neutrophil-epithelial cell adhesion. American Journal of Respiratory Cell and Molecular Biology 7: 214–221.
Chiou, W.F., C.C. Chen, and B.L. Wei. 2011. 8-Prenylkaempferol suppresses influenza A virus-induced RANTES production in A549 cells via blocking PI3K-mediated transcriptional activation of NF-kappaB and IRF3. Evidence-based Complementary and Alternative Medicine 2011: 920828.
Yamaya, M., H. Nishimura, Y. Hatachi, M. Yoshida, H. Fujiwara, M. Asada, et al. 2011. Procaterol inhibits rhinovirus infection in primary cultures of human tracheal epithelial cells. European Journal of Pharmacology 650: 431–444.
Haasbach, E., S.J. Reiling, C. Ehrhardt, K. Droebner, A. Ruckle, E.R. Hrincius, et al. 2013. The NF-kappaB inhibitor SC75741 protects mice against highly pathogenic avian influenza A virus. Antiviral Research 99: 336–344.
Barnes, P.J., and M. Karin. 1997. Nuclear factor-kappaB: a pivotal transcription factor in chronic inflammatory diseases. New England Journal of Medicine 336: 1066–1071.
Baeuerle, P.A., and T. Henkel. 1994. Function and activation of NF-kappa B in the immune system. Annual Review of Immunology 12: 141–179.
Mazur, I., W.J. Wurzer, C. Ehrhardt, S. Pleschka, P. Puthavathana, T. Silberzahn, et al. 2007. Acetylsalicylic acid (ASA) blocks influenza virus propagation via its NF-kappaB-inhibiting activity. Cellular Microbiology 9: 1683–1694.
Trinh, H.T., I.A. Lee, Y.J. Hyun, and D.H. Kim. 2011. Artemisia princeps Pamp. Essential oil and its constituents eucalyptol and alpha-terpineol ameliorate bacterial vaginosis and vulvovaginal candidiasis in mice by inhibiting bacterial growth and NF-kappaB activation. Planta Medica 77: 1996–2002.
Haasbach, E., C. Hartmayer, and O. Planz. 2013. Combination of MEK inhibitors and oseltamivir leads to synergistic antiviral effects after influenza A virus infection in vitro. Antiviral Research 98: 319–324.
Zheng, B.J., K.W. Chan, Y.P. Lin, G.Y. Zhao, C. Chan, H.J. Zhang, et al. 2008. Delayed antiviral plus immunomodulator treatment still reduces mortality in mice infected by high inoculum of influenza A/H5N1 virus. Proceedings of the National Academy of Sciences of the United States of America 105: 8091–8096.
Acknowledgments
This work was supported by a Natural Science Foundation of China grant (81470186) and a Guangdong Provincial Natural Science Fund for Research grant (Team Project, S2012030006598). We thank International Science Editing (Co. Clare, Ireland) for the language editorial assistance in the preparation of the manuscript.
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
The study was approved by the Animal Care and Use Committee of the Guangzhou University of Chinese Medicine (Guangzhou, China). Humane endpoints are chosen in the experimental animals (e.g., survival study) via euthanasia and use of anesthesia. Compliance with regulations for the administration of affairs concerning experimental animals of Guangdong Province (2010, No.41).
Conflict of Interest
The authors declare that they have no conflicts of interest.
Rights and permissions
About this article
Cite this article
Li, Y., Lai, Y., Wang, Y. et al. 1, 8-Cineol Protect Against Influenza-Virus-Induced Pneumonia in Mice. Inflammation 39, 1582–1593 (2016). https://doi.org/10.1007/s10753-016-0394-3
Published:
Issue Date:
DOI: https://doi.org/10.1007/s10753-016-0394-3