Abstract
Kynurenic acid (KYNA) is one of the end products of tryptophan metabolism. The aim of this study was to analyse plasma KYNA concentration in septic shock patients (SSP) with acute kidney injury (AKI) undergoing continuous veno-venous haemofiltration (CVVH). Changes in KYNA content were compared to alterations in the levels of procalcitonin (PCT), C-reactive protein and lactate. Adult SSP with AKI were examined. Measurements were conducted at seven time points: before beginning CVVH and at 6, 12, 24, 48, 72 and 96 h after the beginning of CVVH. Based on clinical outcomes, the data were analysed separately for survivors and non-survivors. Twenty-seven patients were studied. CVVH was associated with reduced plasma KYNA concentration only in survivors. Plasma KYNA concentration correlated with the levels of lactate and PCT only in survivors. (1) CVVH reduced plasma KYNA concentration only in survivors; (2) lack of this reduction may predict fatal outcomes in SSP.
Similar content being viewed by others
Avoid common mistakes on your manuscript.
BACKGROUND
The kynurenine pathway represents a major route for the peripheral metabolism of tryptophan. The process is initiated by tryptophan-2,3-dioxygenase (TDO) and indoleamine-2,3-dioxygenase (IDO). Currently, investigators focus their attention mainly on the role of IDO, which is an inducible enzyme found in cells that are involved in immune reactions [1]. It has been found that IDO is activated during bacterial or viral infection, in autoimmune disease and after severe trauma [2–4]. Circulating cytokines stimulate IDO expression and activity [4, 5]. Interestingly, increased concentrations of tryptophan metabolites, such as quinolinic acid and kynurenic acid (KYNA), depend on the severity of infection [2].
KYNA is a broad-spectrum antagonist of the ionotropic glutamate receptor and of the α7 nicotinic receptor. The role of KYNA in different brain pathologies has been widely described, whereas its peripheral function is not understood as well. The synthesis of KYNA has been documented in the heart, liver and vascular endothelium [6–8]. Importantly, kynurenine metabolites were recently implicated in the pathophysiologies of various acute and chronic diseases, including inflammation (via inhibition of T cell and natural killer function, inhibition of granulocyte activation and tumour necrosis factor alpha (TNFα) production), sepsis and trauma [2, 9–15].
Septic shock is a major cause of death in critically ill patients who are treated in intensive care units (ICUs). The mortality rate of patients in septic shock remains high and ranges between 30 and 50 % [16, 17]. It is associated with increased levels of pro-inflammatory and anti-inflammatory mediators, which cause endothelial injury and multi-organ failure. Diagnosis of the systemic inflammatory response to infection is based mainly on clinical status and biochemical markers including leukocytosis and increases in plasma levels of procalcitonin (PCT), C-reactive protein (CRP) and lactate. However, currently, there is no gold standard for the diagnosis of severe inflammatory responses. The measurement of plasma PCT concentration seems to be the most reliable diagnostic marker [18].
Acute kidney injury (AKI) is frequently associated with septic shock. Despite improvements in the treatment of AKI in septic shock patients, mortality rates remain high. Conventional daily haemodialysis is routinely used to treat AKI, but continuous veno-venous haemofiltration (CVVH) is increasingly popular [19, 20]. Slow and continuous fluid removal, cardiovascular stability and easily controlled biochemical disturbances are the main advantages of CVVH [20]. Several studies have documented significantly decreased plasma concentrations of the proinflammatory cytokines CRP and PCT during CVVH [21, 22]. Nevertheless, a decline in the levels of these mediators was not shown to be a reliable predictor of clinical outcome. Some authors have suggested that metabolites of tryptophan could be useful in the prediction of the outcomes of septic shock [9, 23–25].
It has been shown that the physiological plasma concentration of KYNA ranges between 25 and 35 nmol/L and increases to micromolar concentrations during inflammatory responses and cytokine release [26, 27]. Therefore, the aim of our study was to analyse the effect of CVVH on plasma KYNA concentrations in patients with AKI who were treated for septic shock. Moreover, changes in plasma KYNA concentrations were analysed in parallel to changes in plasma PCT, CRP and lactate levels.
PATIENTS AND METHODS
Ethics
This prospective observational study was conducted in the First Clinic of Intensive Therapy at the Medical University of Lublin, Poland. The study was conducted in accordance with the intensive care unit (ICU) protocol, the Declaration of Helsinki and applicable regulatory requirements as approved by the Institutional Review Board and the local institutional ethics committee. Informed consent was obtained from the legal representatives of patients because all patients were sedated and on mechanical ventilation (MV).
Patient Selection
Adult patients treated with CVVH due to AKI related to septic shock were enrolled. Sepsis was defined as the suspicion of infection plus the systemic response to it (such as tachypnea, tachycardia and hyperthermia or hypothermia). Septic shock was defined as sepsis with evidence of altered organ perfusion associated with hypotension [28]. The diagnosis of AKI was based on RIFLE criteria [29] that included: (1) decrease in diuresis despite fluid and/or diuretic therapy to 0.3 ml/kg/h or less (i.e., oliguria or anuria), (2) decrease in glomerular filtration rate (GFR) > 75 % and (3) increase in serum potassium concentration above 5.5 mmol/L combined with a threefold increase in serum creatinine level. Pregnant women, patients below the age of 18 years, patients with haematological, neoplastic, severe endocrine and metabolic disorders, transplant recipients, HIV-infected patients and those receiving immunosuppressive or steroid drugs or with a do-not-resuscitate order and life expectancy of less than one month were excluded from this study.
Data Collection
For the entire duration of the ICU stay, relevant demographic, clinical and laboratory data were registered in an electronic database along with daily assessments of fluid balance, sepsis-related organ failure assessment (SOFA) scores, MV settings and advanced haemodynamic monitoring variables (obtained with a Swan-Ganz catheter). These data were supplemented by mortality on day 28.
The severity of illness upon ICU admission was described by the acute physiology and chronic health evaluation (APACHE-II) score. For the Glasgow coma score, the best value (before the use of sedation) was used as all the patients were sedated and intubated.
Monitoring and Treatment Techniques
Before starting CVVH, a Swan-Ganz catheter (Arrow Int., Reading, PA, USA) was inserted via the left internal jugular vein. Its position was confirmed by chest X-ray examination. Pulmonary and systemic haemodynamic parameters were measured during the examination period. Fluid administration, vasopressor use and respiratory settings were titrated to obtain adequate oxygen saturation of haemoglobin in mixed-venous blood (SvO2 > 70 %) to keep the rate of oxygen delivery balanced against consumption (keeping haematocrit levels above 30 %). All patients received mineralocorticosteroid therapy (intravenous hydrocortisone infusion at a daily dose of 300 mg). Antibiotic therapy was based on bacteriological results. Systemic arterial blood pressures were measured continuously in the radial artery.
Post-dilution CVVH was performed with a Prismaflex (Gambro, AB, Lund, Sweden) CVVH monitor. A percutaneous double-lumen catheter (Arrow Int., Reading, Pennsylvania, USA) was inserted into the femoral or jugular vein using the standard Seldinger technique. Blood was extracorporeally circulated at a rate of 200 to 250 ml/min through a polysulfone membrane ST 150 (Gambro, AB, Lund, Sweden). High-volume CVVH was performed (70 to 75 ml/kg body weight) during the first 6 h of therapy, followed by low-volume CVVH (35 ml/kg body weight) throughout the remainder of the treatment. Fluid removal at a constant rate of 150 to 200 ml/h was started 6 h after the initiation of CVVH. The ultrafiltration (UF) volume was measured hourly and was balanced according to haemodynamic status. Anticoagulation was achieved using the criteria described by Ostermann and colleagues [30]. The APTT was measured every 4 h. The filter was changed after 48 h or when an excessive increase in transmembrane pressure prevented ultrafiltration.
All patients with gastrointestinal dysfunction grade III or IV [31] received total parenteral nutrition using SMOF Kabiven solution (Fresenius Kabi, Uppsala, Sweden). The mean delivery of calories ranged from 30 to 35 kcal/kg body weight per day. In patients with detectable bowel sounds, the enteral feeding was supplemented with Nutrison Multi Fibre (Nutricia, UK) to reach the target caloric energy supply per day.
Study Protocol and Primary Endpoint
Measurements were taken before CVVH (0 h), and 6, 12, 24, 48, 72 and 96 h after the beginning of CVVH. Based on clinical outcomes, patients were allocated into two groups: patients who survived CVVH treatment (survivors) and patients who died during CVVH, but after 96 h from the beginning of CVVH (non-survivors).
Determination of Studied Parameters
Plasma KYNA concentration was measured fluorometrically. Briefly, blood plasma was deproteinated with 50 % trichloroacetic acid and centrifuged. The supernatant was applied to cation-exchange resin (Dowex 50W+, Sigma). KYNA was eluted, subjected to HPLC (Hewlett Packard 1050 HPLC system: ESA catecholamine HR-30, 3 μm, C18 reverse-phase column) and quantified fluorometrically (Hewlett Packard 1046A fluorescence detector: excitation 344 nm, emission 398 nm). KYNA concentrations were expressed in nM. [32, 33].
Plasma CRP concentration was measured according to the immunoturbidimetric method with latex (ADVIA 1650 analyser, Siemens, USA). Values higher than 5 mg/L were considered clinically important. Plasma PCT concentration was measured using the electrochemiluminescence (ECLIA) method (Cobas e601 analyser, Roche, France). Values greater than 2 ng/mL were considered clinically important. Plasma lactate concentrations were measured with the Cobas b221 analyser (Roche, France). Values greater than 1 mmol/L were considered clinically significant.
STATISTICS
Means and standard deviations (SD) were calculated for parametric data. The value at time point 0 was regarded as the baseline. Categorical variables were compared using the χ 2 and Fisher's exact test and Yates' correction was applied. Student's unpaired t test was used to analyse variables with normal distribution. Non-parametric data were analysed statistically using the Wilcoxon signed-rank test and the Kruskal–Wallis ANOVA test for initial detection of differences. Dunnett's post hoc and Spearman's rank correlation tests were used for inter-point and inter-group comparisons. Additionally, the Spearman's rank correlation test was used for the overall analysis. A P value of P < 0.05 was considered to be significant. A preliminary estimate of sample size was based on expected differences in plasma KYNA concentrations between baseline and 96 h. With a type I error of 0.05 and a type II error of 0.2, the required sample size was 19–23 patients. The dropout rate was estimated at 10 %; thus, a minimum of 26 patients was examined. The sample size was determined using Statistica 9 software. The power of all statistical tests was determined using G*Power software(1 − β).
RESULTS
Forty septic shock patients with AKI were studied; of these, 12 patients were excluded: six patients died during the study period, and their data were thus incomplete; one patient required massive fluid resuscitation due to severe coagulation disorders following bleeding and died at day 5 following ICU admission; three required emergency laparotomies due to intra-abdominal bleeding (two of them died during CVVH); one patient was excluded due to very large haemolysis during sample preparation; and one was excluded because his legal representatives withdrew consent for blood collection. Therefore, this study was completed for 28 patients; 17 male and 11 female aged 60 ± 12 years (Table 1). Fourteen patients were treated for severe pneumonia due to bacterial infection (Pseudomonas aeruginosa, Klebsiella pneumoniae, Acinetobacter baumannii, Streptococcus pneumoniae, Candida glabrata), six for peritonitis (Enterococcus faecalis, Escherichia coli, Candida albicans, Stenotrophomonas maltophilia), three for urinary tract infection (Staphylococcus haemolyticus, Escherichia coli) and one patient was treated after hysterectomy due to pyometra (Enterococcus faecalis, Candida albicans). One patient was treated for sepsis related to an oral abscess (Coagulase-negative staphylococcus, Candida albicans), one patient was treated for a purulent spinal infection (Acinetobacter baumannii, Staphylococcus aureus) and one patient was treated for a purulent crotch infection (Proteus mirabilis, Enterococcus faecalis). The choice of antimicrobial therapy was determined after the culture and sensitivity analysis (Table 2). In all patients, it was administered intravenously.
The mean duration of CVVH was 11.30 ± 1.67 days and was similar in both groups. Nineteen patients survived CVVH treatment (survivors group); however, one patient died at day 24 after ICU admission and two others died at days 26 and 27, respectively. Nine patients died during CVVH (32.1 %), but only after the 96-h study period (non-survivors group). At 28 days, mortality was 52.5 % for the entire group of patients enrolled in the present study.
The critical gastrointestinal dysfunction (III or IV degree) was diagnosed in all participants at the day of admission into ICU. During 96 h of treatment with CVVH, the gastrointestinal function did not improve in non-survivors, whereas the bowel sounds were detected in 74 % of survivors and the enteral feeding was supplemented at the third to fourth day of treatment.
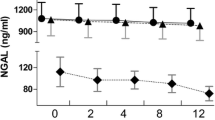
The median value of plasma KYNA concentration was 73.5 nM ([14.28, 131.13]; quartiles 1 and 3, respectively) in survivors and 40.59 nM (15.73, 302.99) in non-survivors, respectively. In survivors, plasma KYNA concentrations decreased starting at 24 h of CVVH, whereas in non-survivors, they increased at 12 and 48 h of CVVH (Table 3). Concentrations did not change compared to baseline values at the remaining time points (Table 3). Plasma KYNA concentrations were significantly higher in non-survivors at 48, 72 and 96 h after the beginning of CVVH compared with those in survivors (Table 3, Fig. 1).
The percentage changes in plasma KYNA, procalcitonin, CRP and lactate concentrations in survivors and non-survivors. The mean of the baseline value was considered to be 100. Time points: Baseline, 6 h after the beginning of CVVH at fluid replacement rates of 70 to 75 ml/kg body weight per min without net UF, 12 h after the beginning of CVVH at fluid replacement rates of 35 ml/kg body weight per min with UF ranging between 150 and 200 ml/h, 24, 48, 72 and 96 h after the beginning of CVVH. In survivors, the percentage values of plasma KYNA concentrations decreased at 6, 12, 24, 48, 72 and 96 h (85, 81, 72, 61, 40 and 35 % of the baseline value, respectively). In non-survivors, the percentage values of plasma KYNA concentrations decreased to 99 % at 6 h of baseline value and increased at 12, 24, 48, 72 and 96 h of baseline value (138, 121, 170, 167 and 148 % of the baseline value, respectively).
The median value of plasma PCT concentration was significantly lower in survivors than in non-survivors at time point 0 (8.89 ng/L [6.72, 23.3] in survivors vs. 51.99 ng/L [29.55, 66.78] in non-survivors). CVVH led to decreased plasma PCT concentration in both groups; however, a higher decline was noted in survivors (Fig. 1, Table 4). Importantly, clinically significant elevation of plasma PCT concentrations was observed throughout the study in non-survivors.
The median value of CRP prior to CVVH was 198.40 mg/L [159.95, 210.81] and 321.90 mg/L [205.03, 386.24] in survivors and non-survivors, respectively. In both groups, CVVH led to decreased plasma concentrations; however, lower values were noted in survivors after 72 h of CVVH (Fig. 1, Table 5).
The baseline value of plasma lactate concentration was significantly lower in survivors than in non-survivors during the entire study period (5.20 mM [4, 8.4] vs. 9.45 mM [8.78, 11.23] in survivors and non-survivors, respectively). Similar to what was observed for PCT and CRP, CVVH led to decreased plasma lactate concentrations in survivors and non-survivors (Fig. 1); however, the decline was greater in survivors than in non-survivors (Table 6).
There were significant correlations between KYNA and lactate concentrations in the studied population (P < 0.001, r = 0.54) as well as in survivors (P < 0.001, r = 0.5). KYNA concentration also showed a slight correlation with PCT concentration in the studied population (P < 0.001, r = 0.36) and in survivors (P < 0.001, r = 0.33). In studied population, plasma KYNA concentrations poorly correlated with plasma alanine aminotransferase (ALT) and aspartate aminotransferase (AST) (P < 0.001, r = 0.33 and P < 0.001, r = 0.3). Plasma KYNA concentration correlated with ALT (P < 0.001, r = 0.45) and AST (P < 0.001, r = 0.44) in non-survivors. There was no correlation between plasma KYNA and CRP concentrations.
Changes in some haemodynamic variables measured by Swan–Ganz catheter were presented in Table 7.
DISCUSSION
We found that the concentration of KYNA in the plasma of septic patients with good clinical outcomes decreased gradually over the course of CVVH. Similarly, the levels of CRP, PCT and lactate decreased gradually during CVVH in this group of patients. In contrast, the concentration of KYNA in the plasma of septic patients with poor clinical results did not decrease over the course of CVVH. In fact, an increase in KYNA concentration was observed. At the same time, the concentrations of CRP, PCT and lactate decreased during CVVH in this group of patients. Plasma KYNA concentration correlated with lactate and PCT only in patients with good outcomes and with ALT and AST in patients with poor clinical outcomes. No correlations were identified between KYNA and CRP, PCT or lactate in septic patients with poor clinical outcomes.
Numerous authors have described an increase in plasma kynurenine concentration and IDO activity in sepsis and in septic shock patients [2, 9, 24, 25]. Moreover, the activity of IDO, which was calculated from the ratio of kynurenine to tryptophan, has been suggested as a marker in the diagnosis of sepsis, septic shock or other diseases. Its activity and the resulting higher levels of kynurenine have been correlated with the severity of sepsis/septic shock, and their persistently elevated values have been noted in non-survivors (i.e., they increased during the initial four days in non-survivor patients) [2, 24, 25]. Tryptophan degradation was also higher after major trauma in non-survivor patients compared to survivors [9]. Some investigators have postulated that the maximum kynurenine/tryptophan ratio was detectable from 1 to 4 days after positive blood culture in septic patients, was stratified by causative bacteria and decreased on recovery. In addition, they observed the highest kynurenine/tryptophan ratios in patients with β-haemolytic streptococcal bacteraemia and the lowest ratios in those with E. coli bacteraemia. The ratio was also significantly higher in septic patients treated for pneumonia compared with those treated for urinary tract infections [23].
Kynurenine is synthesised metabolically from tryptophan. The activation of TDO and IDO following infection decreases the concentration of tryptophan in plasma and increases that of kynurenine [5, 34]. The stimulation of IDO increases tryptophan catabolism and contributes to the synthesis of the several tryptophan metabolites [11]. Kynurenine is an intermediate metabolite on the kynurenine pathway. It is mainly metabolised by two enzymes, kynurenine-3-hydroxylase and kynureninase. The resulting metabolites are 3-hydroxykynurenine, anthranilic acid, 3-hydroxyanthranilic acid, quinolinic acid and nicotinamide adenine dinucleotide (NAD+). It is important to note that this process progresses both in vivo and in vitro. Therefore, the precise measurement of plasma kynurenine concentrations in collected samples requires deactivation of the processes described above. In contrast to kynurenine, KYNA is not metabolised and is stable in solution. A precise and efficient method of separation has been developed using Dowex resin. Moreover, a sensitive chromatographic method has also been developed that enables the determination of KYNA concentrations in femtomolar concentrations. Therefore, measurement of KYNA content may be a good candidate for a laboratory indicator of sepsis.
The plasma KYNA concentration depends on tryptophan and KYNA supplementation, the activity of kynurenine enzymes and the rate of KYNA elimination.
Nutritional habits were strictly controlled during CVVH therapy. During the first few days, all patients received total parenteral nutrition containing 4.5 pmol/mL of KYNA (data not shown) and 1.5 g of tryptophan (Smof Kabiven). It is noteworthy that more than 90 % of plasma tryptophan is metabolised via the kynurenine pathway [35]. When abdominal sounds were detectable, enteral protein nutrition was started. The KYNA content in Nutrison Multi Fibre is 12.5 pmol/L. In all cases, the nutritional preparations were administered continuously, which maintained constant amounts of KYNA and its precursors. Interestingly, treatment with KYNA, which is N-methyl-d-aspartate receptor antagonist decreased obstruction-caused intestinal hypermotility in dogs and 2,4,6-trinitrobenzensulfonic acid-induced colitis in rats [14, 36]. Moreover, some experimental studies documented, that treatment with KYNA significantly reduced the level of inflammatory mediators, such as TNFα and interleukine 6 [36, 37]. On the other hand, circulating cytokines promote kynurenine metabolism and subsequent generation of tryptophan metabolites, including KYNA [2, 3, 5, 38]. Therefore, we can speculate that persistent plasma KYNA concentration results from elevated level of proinflammatory cytokines (despite CVVH) and persisted inflammation in non-survivors; however, this hypothesis requires further studies.
Endogenous KYNA is synthesised from kynurenine by kynurenine aminotransferases [13, 39]. KYNA is not further metabolised in mammals and is eliminated in urine [35]. AKI that follows septic shock may strongly determine the concentration of plasma KYNA because plasma KYNA concentration depends on the rate of its elimination through urine [27, 40, 41]. However, the rate of KYNA elimination during CVVH has not been documented. Indeed, the plasma KYNA/tryptophan ratio has been considered as a sensitive biomarker for the assessment of renal function and an increase in plasma KYNA concentration has predicted incidence of AKI [42, 43]. In patients with chronic renal diseases, increased plasma concentrations of tryptophan metabolites were reduced by renal replacement therapy [27, 42–44]. Intermittent blood purification-haemodialysis reduced plasma kynurenine and quinolinic acid by 30 and 75 %, respectively [41]. Moreover, high concentrations of both metabolites prior to haemodialysis were likely to result from the induction of TDO activity, despite the fact that the IDO activity increased rapidly in response to immune stimulation [13–15, 23, 25, 35, 41, 44]. It can be assumed that in our patients KYNA was eliminated continuously. It can also be assumed that the rate of elimination was constant and did not depend on kidney function. Thus, in the clinical situation studied here, the changes in plasma KYNA concentration depended mainly on the rate of KYNA synthesis. Therefore, a hypothesis may be proposed that the levels of KYNA fell due to its exhaustion in patients that survived septicaemia. This may indicate a beneficial effect of KYNA and should be addressed in appropriate animal models of septicaemia. Although this hypothesis does not address the reasons for the lack of decline of KYNA levels in fatal outcomes of septicaemia, it is still important to elucidate how KYNA and its analogs can benefit septic patients.
During CVVH, plasma KYNA concentrations decreased in survivor patients, whereas they were practically unchanged in non-survivor patients. It is worth stressing that other inflammatory markers, such as CRP, PCT and lactate, decreased in survivors as well as non-survivors following CVVH. Moreover, decreasing plasma KYNA concentration correlated with lactate and PCT in survivors only. It is important to note that KYNA was the only indicator for which plasma concentration was practically unchanged. Although the reason for the high content of KYNA in non-survivor patients is unknown, the prognostic value of this finding is not to be underestimated. The small sample of non-survivors significantly limited the power of statistical analysis. Therefore, our preliminary results should be verified in further studies.
CONCLUSIONS
In conclusion, our study documented that CVVH significantly reduced plasma KYNA concentrations in septic shock patients. Surprisingly, such an effect was noted only in survivors, whereas plasma KYNA concentration was practically unchanged in non-survivors. Furthermore, decreasing plasma KYNA concentration correlated with plasma PCT and lactate concentrations. Based on our findings, we can suggest that plasma KYNA, together with CRP, PCT and lactate concentrations, may be useful as an indicator of inflammatory processes. However, larger clinical studies are necessary to demonstrate more strongly the prognostic value of KYNA in septic shock patients.
References
Tan, P.H., and A.K. Bharath. 2009. Manipulation of indoleamine 2,3 dioxygenase; a novel therapeutic target for treatment of diseases. Expert Opinion on Therapeutic Targets 13: 987–1012.
Zeden, J.P., G. Fusch, B. Holtfreter, J.C. Schefold, P. Reinke, G. Domanska, J.P. Haas, M. Gruendling, A. Westerholt, and C. Schuett. 2010. Excessive tryptophan catabolism along the kynurenine pathway precedes ongoing sepsis in critically ill patients. Anaesthesia and Intensive Care 38: 307–316.
Yeung, A.W., W. Wu, M. Freewan, R. Stocker, N.J. King, and S.R. Thomas. 2012. Flavivirus infection induces indoleamine 2,3-dioxygenase in human monocyte-derived macrophages via tumor necrosis factor and NF-κB. Journal of Leukocyte Biology 91: 657–666.
Schefold, J.C., J.P. Zeden, R. Pschowski, B. Hammoud, C. Fotopoulou, D. Hasper, G. Fusch, S. Von Haehling, H.D. Volk, C. Meisel, C. Schütt, and P. Reinke. 2010. Treatment with granulocyte-macrophage colony-stimulating factor is associated with reduced indoleamine 2,3-dioxygenase activity and kynurenine pathway catabolites in patients with severe sepsis and septic shock. Scandinavian Journal of Infectious Diseases 42: 164–171.
O'Connor, J.C., C. Andre, Y. Wang, M.A. Lawson, S.S. Szegedi, J. Lestage, N. Castanon, K.W. Kelly, and R. Dantzer. 2009. Interferon gamma and tumor necrosis factor alpha mediate the upregulation of indoleamine 2,3-dioxygenase and induction of depressive—like behaviour in mice in response to bacillus Calmette-Guerin. Journal of Neuroscience 29: 4200–4209.
Baran, H., G. Amann, B. Lubec, and G. Lubec. 1997. Kynurenic acid and kynurenine aminotransferase in heart. Pediatric Research 41: 404–410.
Noguchi, T., Y. Minatogawa, E. Okuno, M. Nakatani, M. Morimoto, and R. Kido. 1975. Purification and characterization of kynurenine-2-oxoglutarate aminotransferase from the liver, brain and small intestine of rats. Biochemistry Journal 151: 399–406.
Stazka, J., P. Luchowski, M. Wielosz, Z. Kleinrok, and E.M. Urbanska. 2002. Endothelium-dependent production and liberation of kynurenic acid by rat aortic rings expose to L-kynurenine. European Journal of Pharmacology 448: 133–137.
Ploder, M., A. Spittler, K. Schroecksanadel, G. Neurauter, L.E. Pelinka, E. Roth, and D. Fuchs. 2009. Tryptophan degradation in multiple trauma patients: survivors compared with non-survivors. Clinical Science 116: 593–598.
Lögters, T.T., M.D. Laryea, J. Altrichter, J. Sokolowski, J. Cinati, J. Reipen, W. Linhart, J. Windolf, M. Scholz, and M. Wild. 2009. Increased plasma kynurenine values and kynurenine-tryptophan ratios after major trauma are early indicators for the development of sepsis. Shock 32: 29–34.
Maes, M., I. Mihaylova, M.D. Ruyter, M. Kubera, and E. Bosmans. 2007. The immune effects of TRYCATs (tryptophan catabolites along the IDO pathway): relevance for depression—and other conditions characterized by tryptophan depletion induced by inflammation. Neuro Endocrinology Letters 28: 826–831.
Jung, I.D., M.G. Lee, J.H. Chang, J.S. Lee, Y.I. Jeong, C.M. Lee, W.S. Park, J. Han, S.K. Seo, S.Y. Lee, and Y.M. Park. 2009. Blockade of indoleamine 2,3-dioxygenase protects mice against lipopolysaccharide-induced endotoxin shock. Journal of Immunology 182: 3146–3154.
Mándi, Y., and L. Vécsei. 2012. The kynurenine system and immunoregulation. Journal of Neural Transmission 119: 197–209.
Kaszaki, J., Z. Palásthy, D. Érces, A. Rácz, C. Torday, G. Varga, L. Vécsei, and M. Boros. 2008. Kynurenine acid inhibits intestinal hypermotility and xanthine oxidase activity during experimental colon obstruction in dogs. Neurogastroenterology and Motility 20: 53–62.
Tiszlavicz, Z., B. Németh, F. Fülöp, L. Vécsei, K. Tápai, I. Ocsovszky, and Y. Mándi. 2011. Different inhibitory effects of kynurenic acid and a novel kynurenic acid analogue on tumour necrosis factor-α (TNF-α) production by mononuclear cells, HMGB1 production by monocytes and HNP1-3 secretion by neutrophils. Naunyn-Schmiedeberg's Archives of Pharmacology 383: 447–455.
Laupland, K.B., H.D. Davies, D.L. Church, T.J. Louie, J.S. Dool, D.A. Zygun, and C.J. Doig. 2004. Bloodstream infection-associated sepsis and septic shock in critically ill adults: a population-based study. Infection 32: 59–64.
Angus, D.C., W.T. Linde-Zwirble, J. Lidicker, G. Clermont, J. Carcillo, and M.R. Pinsky. 2001. Epidemiology of severe sepsis in the United States: analysis of incidence, outcome and associated costs of care. Critical Care Medicine 29: 1303–1310.
Uzzan, B., R. Cohen, P. Nicolas, M. Cucherat, and G.Y. Perret. 2006. Procalcitonin as a diagnostic test for sepsis in critically ill adults and after surgery or trauma: a systematic review and meta-analysis. Critical Care Medicine 34: 1996–2003.
Bellomo, R., D. Mansfield, S. Rumble, J. Shapiro, G. Parkin, and N. Bouce. 1993. A comparison of conventional dialytic therapy and acute continuous hemodiafiltration in the management of acute renal failure in the critically ill. Renal Failure 15: 595–602.
Ronco, C., R. Bellomo, P. Homel, A. Brendolan, M. Dan, P. Piccinni, and G. La Greca. 2000. Effects of different doses in continuous veno-venous haemofiltration on outcomes of acute renal failure: a prospective randomized trial. Lancet 355: 26–30.
Peng, Z., P. Pai, L. Hong–Bao, L. Rong, W. Han–Min, and H. Chen. 2010. The impacts of continuous veno-venous hemofiltration on plasma cytokines and monocyte human leukocyte antigen-DR expression in septic patients. Cytokine 50: 186–191.
Heering, P., S. Morgera, F.J. Schmitz, G. Schmitz, R. Willers, H.P. Schultheiss, B.E. Stauer, and B. Grabensee. 1997. Cytokine removal and cardiovascular hemodynamics in septic patients with continuous veno-venous hemofiltration. Intensive Care Medicine 23: 288–296.
Petrovaara, M., A. Raitala, T. Lehtimäki, P.J. Karhunen, S.S. Oja, M. Jalhä, A. Hervonen, and M. Hurme. 2006. Indoleamine 2,3-dioxygenase activity in nonagenarians in markedly increased and predicts mortality. Mechanisms of Ageing and Development 127: 497–499.
Huttenen, R., J. Syrjänen, J. Aittoniemi, S.S. Oja, A. Raitala, J. Laine, M. Pertovaara, R. Vuento, H. Huhtala, and M. Hurme. 2010. High activity of indoleamine 2,3 dioxygenase enzume predicts disease severity and case fatality in bacteriemic patients. Shock 33: 149–154.
Girgin, G., T.T. Sahin, D. Fuchs, O. Yuksel, O. Kurukahvecioglu, M. Sare, and T. Baydar. 2011. Tryptophan degradation and serum neopterin concentrations in intensive care unit patients. Toxicology Mechanisms and Methods 21: 231–235.
Fukushima, T., S. Mitsuhashi, M. Tomiya, M. Iyo, K. Hashimoto, and T. Toyo'oka. 2007. Determination of kynurenic acid in human serum and its correlation with the concentration of certain amino acids. Clinica Chimica Acta 377: 174–178.
Pawlak, D., K. Pawlak, J. Malyszko, M. Mysliwiec, and W. Buczko. 2001. Accumulation of toxic products degradation of kynurenine in hemodialyzed patients. International Urology and Nephrology 33: 399–404.
Bone, R.C. 1991. Let's agree on terminology: definitions of sepsis. Critical Care Medicine 19: 973–976.
Ricci, Z., D. Cruz, and C. Ronco. 2008. The RIFLE criteria and mortality in acute kidney injury: a systematic review. Kidney International 73: 538–546.
Osterman, M., H. Dickie, L. Tovey, and D. Trecher. 2010. Heparin algorithm for anticoagulation during continuous renal replacement therapy. Critical Care 14: 419–420.
Reintam Blaser, A., M.L. Malbrain, J. Starkopf, S. Fruhwald, S.M. Jakob, J. De Waele, J.P. Braun, M. Poeze, and C. Spies. 2012. Gastrointestinal function in intensive care patients: terminology, definitions and management. Recommendations of the ESICM Working Group on Abdominal Problems. Intensive Care Medicine 38: 384–394.
Shibata, K. 1988. Fluorimetric micro-determination of kynurenic acid, an endogenous blocker of neurotoxicity, by high-performance liquid chromatography. Journal of Chromatography 430: 376–380.
Turski, W.A., M. Nakamura, W.P. Todd, B.K. Carper Carpenter, W.O. Whetsell Jr., and R. Schwarcz. 1988. Identification and quantification of kynurenic acid in human brain tissue. Brain Research 454: 164–169.
MacKenzie, C.R., K. Heseler, A. Muller, and W. Däubener. 2007. Role of indoleamine 2,3-dioxygenase in antibacterial defense and immuno-regulation: tryptophan depletion versus production of toxic kynurenines. Current Drug Metabolism 8: 237–244.
Bender, D.A. 1983. Biochemistry of tryptophan in health and disease. Molecular Aspects of Medicine 6: 101–197.
Varga, G., D. Érces, B. Fazekas, M. Fülöp, T. Kovács, J. Kaszaki, F. Fülöp, L. Vécsei, and M. Boros. 2010. N-methyl-d-aspartate receptor antagonism decreases motility and inflammatory activation in the early phase of acute experimental colitis in the rat. Neurogastroenterology and Motility 22: 217–225.
Érces, D., G. Varga, B. Fazekas, T. Kovács, T. Tökés, L. Tiszlavicz, F. Fülöp, L. Vécsei, M. Boros, and J. Kaszaki. 2012. N-methyl-d-aspartate receptor antagonist therapy suppresses colon motility and inflammatory activation six days after onset of experimental colitis in rats. European Journal of Pharmacology 691: 225–234.
Asp, L., A.S. Johansson, A. Mann, B. Owe-Larsson, E.M. Urbanska, T. Kocki, M. Kegel, G. Engberg, G.B. Lundkvist, and H. Karlsson. 2011. Effects of pro-inflammatory cytokines on expression of kynurenine pathway enzymes in human dermal fibroblasts. Journal of Inflammation 8: 25.
Stone, T.W., C.M. Forrest, and L.G. Darlington. 2012. Kynurenine pathway inhibition as a therapeutic strategy for neuroprotection. FEBS Journal 279: 1386–1397.
Pawlak, K., A. Kowalewska, M. Myśliwiec, and D. Pawlak. 2009. Kynurenine and its metabolites—kynurenic acid and anthranilic acid are associated with soluble endothelial adhesion molecules and oxidative status in patients with chronic kidney disease. American Journal of the Medical Sciences 338: 293–300.
Schefold, J.C., J.P. Zeden, C. Fotopoulou, S. von Haeling, R. Pschowski, D. Hasper, H.D. Volk, C. Schuett, and P. Reike. 2009. Increased indoleamine 2,3-dioxygenase (IDO) activity and elevated serum levels of tryptophan catabolites in patients with chronic kidney disease: a possible link between chronic inflammation and uraemic symptoms. Nephrology, Dialysis, Transplantation 24: 1901–1908.
Zhao, J. 2013. Plasma kynurenic acid/tryptophan ratio: a sensitive and reliable biomarker for the assessment of renal function. Renal Failure 35: 648–653.
Rhee, E.P., C.B. Clish, A. Ghorbani, M.G. Larson, S. Elmariah, E. McCabe, Q. Yang, S. Cheng, K. Pierce, A. Deik, A.L. Souza, L. Farrell, C. Domos, R.W. Yeh, I. Palacios, K. Rosenfield, R.S. Vasan, J.C. Florez, T.J. Wang, C.S. Fox, and R.E. Gerszten. 2013. A combined epidemiologic and metabolomic approach improves CKD prediction. Journal of the American Society of Nephrology. doi:10.1681/ASN.2012101006.
Saito, K., S. Fujigaki, M. Heyes, K. Shibata, M. Takamura, H. Fujii, H. Wada, A. Noma, and M. Seishima. 2000. Mechanism of increases in L-kynurenine and quinolinic acid in renal insufficiency. American Journal of Physiology. Renal Physiology 279: F565–F572.
Acknowledgements
The authors would like to thank Professor Waldemar Turski (Department of Clinical and Experimental Pharmacology, Medical University of Lublin, Poland), for his valuable suggestions and for sharing his expertise during the preparation of this manuscript. This study was partially supported by the Polish Science Foundation (FNP).
Author information
Authors and Affiliations
Corresponding author
Rights and permissions
Open Access . This article is distributed under the terms of the Creative Commons Attribution License which permits any use, distribution, and reproduction in any medium, provided the original author(s) and the source are credited.
To view a copy of this licence, visit http://creativecommons.org/licenses/by/2.0/.
About this article
Cite this article
Dabrowski, W., Kocki, T., Pilat, J. et al. Changes in Plasma Kynurenic Acid Concentration in Septic Shock Patients Undergoing Continuous Veno-Venous Haemofiltration. Inflammation 37, 223–234 (2014). https://doi.org/10.1007/s10753-013-9733-9
Published:
Issue Date:
DOI: https://doi.org/10.1007/s10753-013-9733-9