Abstract
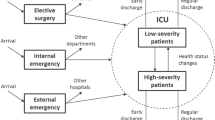
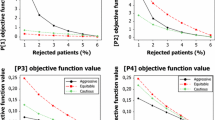
This paper deals with the management of scarce health care resources. We consider a control problem in which the objective is to minimize the rate of patient rejection due to service saturation. The scope of decisions is limited, in terms both of the amount of resources to be used, which are supposed to be fixed, and of the patient arrival pattern, which is assumed to be uncontrollable. This means that the only potential areas of control are speed or completeness of service. By means of queuing theory and optimization techniques, we provide a theoretical solution expressed in terms of service rates. In order to make this theoretical analysis useful for the effective control of the healthcare system, however, further steps in the analysis of the solution are required: physicians need flexible and medically-meaningful operative rules for shortening patient length of service to the degree needed to give the service rates dictated by the theoretical analysis. The main contribution of this paper is to discuss how the theoretical solutions can be transformed into effective management rules to guide doctors’ decisions. The study examines three types of rules based on intuitive interpretations of the theoretical solution. Rules are evaluated through implementation in a simulation model. We compare the service rates provided by the different policies with those dictated by the theoretical solution. Probabilistic analysis is also included to support rule validity. An Intensive Care Unit is used to illustrate this control problem. The study focuses on the Markovian case before moving on to consider more realistic LoS distributions (Weibull, Lognormal and Phase-type distribution).














Similar content being viewed by others
References
Zenios SA (2004) Patient choice in kidney allocation: the role of the queueing discipline. Manuf Serv Oper Manag 6:280–301
Seshaiah CV, Thiagaraj HB (2011) A queueing network congestion model in hospitals. Eur J Oper Res 63:419–427
Solberg B, Asplin B, Weinick R, Magid D (2003) Emergency department crowding: consensus development of potential measures. Ann Emerg Med 42:824–834
de Bruin AM, Bekker R, van Zanten L, Koole GM (2010) Dimensioning hospital wards using the Erlang loss model. Ann Oper Res 178:23–43
Cochran JK, Barthi A (2006) Stochastic bed balancing of an obstetrics hospital. Health Care Manag Sci 9:31–45
Griffiths JD, Price-Lloyd N, Smithies M, Williams JE (2005) Modelling the requirement for supplementary nurses in an intensive care unit. J Oper Res Soc 56:126–133
Bekker R, Koeleman PM (2011) Scheduling admissions and reducing variability in bed demand. Health Care Manag Sci 14:237–249
Harper P, Gamlin H (2003) Reduced outpatient waiting times with improved appointment scheduling: a simulation modelling approach. OR-Spectrum 25:207–222
Vasilakis C, Sobolev BG, Kuramoto L, Levy AR (2007) A simulation study of scheduling clinic appointments in surgical care: individual surgeon versus pooled lists. J Oper Res Soc 58:202–211
Lakshmi C, Sivakumar A (2013) Application of queueing theory in health care: a literature review. Oper Res Health Care 2:25–39
Gross D, Harris CM (2008) Fundamentals of queueing theory. Wiley
Terekhov D, Beck JC (2008) A constraint programming approach for solving a queueing control problem. J Art Int Res 32:123–167
Stidham S (2002) Analysis, design and control of queueing systems. Oper Res 50:197–216
Mallor F, Azcárate C (2014) Combining optimization with simulation to obtain credible models for intensive care units. Ann Oper Res 221:255–271
Anderson D, Price C, Golden B, Jank G, Wasil E (2011) Examining the discharge practices of surgeons at a large medical center. Health Care Manag Sci 14:338–347
Dobson G, Lee H, Pinker E (2010) A model of ICU bumping. Oper Res 58:1564–1576
Shmueli A, Sprug CL, Kaplan E (2003) Optimizing admissions to an intensive care unit. Health Care Manag Sci 6:131–136
Capuzzo M, Moreno RP, Alvisi R (2010) Admission and discharge of critically ill patients. Curr Opin Crit Care 16:499–504
Kramer AA, Higgins TL, Zimmerman JE (2012) Intensive care unit readmissions in U.S. hospitals: patient characteristics, risk factors, and outcomes. Crit Care Med 40:3–10
Marmor YN, Rohleder TR, Cook DJ, Huschka TD, Thompson JE (2013) Recovery bed planning in cardiovascular surgery: a simulation case study. Health Care Manag Sci. doi:10.1007/s10729-013-9231-5
Robert R, Reignier J, Tournoux-Facon C et al (2012) Refusal of intensive care unit admission due to a full unit: impact on mortality. Am J Respir Crit Care Med 185:1081–1087
Sprung CL, Baras M, Iapichino G et al (2012) The Eldicus prospective, observational study of triage decision making in European intensive care units: part I–European intensive care admission triage scores. Crit Care Med 40:125–131
Lin F, Chaboyer W, Wallis M (2009) A literature review of organisational, individual and teamwork factors contributing to the ICU discharge process. Aust Crit Care 22:29–43
Sinuff T, Kahnamoui K, Cook DJ et al (2004) Rationing critical care beds: a systematic review. Crit Care Med 32:1588–1597
Walter KL, Siegler M, Hall JB (2008) How decisions are made to admit patients to medical intensive care units (MICUs): a survey of MICU directors at academic medical centers across the United States. Crit Care Med 36:414–420
Ridge JC, Jones SK, Nielsen MS, Shahani AK (1998) Capacity planning for intensive care units. Eur J Oper Res 105:346–355
Costa AX, Ridley SA, Shahani AK, Harper PR, De Senna V, Nielsen MS (2003) Mathematical modelling and simulation for planning critical care capacity. Anaesthesia 58:320–327
Sprung CL, Danis M, Iapichino G et al (2013) Triage of intensive care patients: identifying agreement and controversy. Int Care Med 39:1916–1924
Task Force of the American College of Critical Care Medicine, Society of Critical Care Medicine (1999) Guidelines for intensive care unit admission, discharge, and triage. Crit Care Med 27:633–638
Azcárate C, Mallor F, Barado J (2012) Calibration of a decision-making process in a simulation model by a bicriteria optimization problem, In Proceedings of the 2012 Winter Simulation Conference, 782–791
Mallor F, Azcárate C, Barado J (2014) Control problems and management policies in health systems. Application to intensive care units. Flex Serv Manuf J. doi:10.1007/s10696-014-9209-8
Wolf RW (1982) Poisson arrivals see time average. Oper Res 30:223–231
Heidegger CP, Treggiari MM, Romand JA (2005) A nationwide survey of intensive care unit discharge practices. Intensive Care Med 31:1676–1682
Barlow RE, Proschan F (1981) Statistical theory of reliability and life testing. To begin with, silver spring, MD
Steyrer J, Schiffinger M, Huber C et al (2013) Attitude is everything? The impact of workload, safety climate, and safety tools on medical errors: a study of intensive care units. Health Care Manage Rev 38:306–316
Metcalfe MA, Sloggett A, McPherson K (1997) Mortality among appropriately referred patients refused admission to intensive-care units. Lancet 350:7–11
Simchen E, Sprung CL, Galai N et al (2007) Survival of critically ill patients hospitalized in and out of intensive care. Crit Care Med 35:449–457
Niven DJ, Bastos JF, Stelfox HT (2014) Critical care transition programs and the risk of readmission or death after discharge from an ICU: a systematic review and meta-analysis. Crit Care Med 42:179–187
Lyons RA, Wareham K, Hutchings HA et al (2000) Population requirement for adult critical-care beds: a prospective quantitative and qualitative study. Lancet 355:595–598
Rauner MS, Zeiles A, Schaffhauser-Linzattti MM, Hornik K (2003) Modelling the effects of the Austrian inpatient reimbursement system on length-of-stay distributions. OR-Spectrum 25:183–206
Vasilakis C, Marshall AH (2005) Modelling nationwide hospital length of stay: opening the black box. J Oper Res Soc 56:862–869
Acknowledgments
This paper has been partially funded by grant MTM2012-36025. The authors would like to extend their gratitude to the reviewers and guest editor for their insightful comments, which have increased the quality of this paper.
Author information
Authors and Affiliations
Corresponding author
Rights and permissions
About this article
Cite this article
Mallor, F., Azcárate, C. & Barado, J. Optimal control of ICU patient discharge: from theory to implementation. Health Care Manag Sci 18, 234–250 (2015). https://doi.org/10.1007/s10729-015-9320-8
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s10729-015-9320-8