Abstract
Background and Aims
The association between obesity and colorectal cancer (CRC) is well established in older individuals, but evidence is limited in the younger population. The study aims to analyze the relationship of obesity and its related comorbidities in early-onset CRC (E-CRC) and compare it to late-onset CRC (L-CRC).
Methods
A retrospective, cross-sectional study was performed on average-risk individuals ≥ 20 years who were active patients in the commercial database, IBM Watson Health Explorys in the last 5 years. Individuals with CRC were compared to those without CRC across different age groups (20–39, 40–49, and 50–74 years). Individuals with CRC diagnosed < 50 years (E-CRC) were compared to those with CRC between 50 and 74 years (L-CRC). Variables included sex, smoking, obese BMI, diabetes mellitus type 2 (DM2), hypertension (HTN), and hyperlipidemia (HLD). Since Explorys aggregates population-level, de-identified data, approval from institutional review board was not required.
Results
Among 37,483,140 individuals, 162,150 cases of sporadic CRC were identified. Compared to the general population, obesity and HLD were independent risk factors for CRC across all age groups; DM2, HTN, and smoking were independent risk factors for CRC in men of all age groups and women with L-CRC. Compared to L-CRC, individuals with E-CRC had lower percentages of obesity-related comorbidities.
Conclusion
In E-CRC, obesity, DM2, HTN, HLD, and smoking are independent risk factors for CRC among men; obesity and HLD are independent risk factors for CRC in women. These subgroups may benefit from a personalized screening approach to detect early-onset CRC.
Similar content being viewed by others
References
Siegel RL, Miller KD. Cancer statistics, 2019. CA Cancer J Clin. 2019;69:7–34.
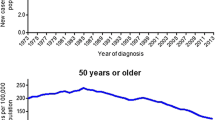
Murphy CC, Sandler RS, Sanoff HK, et al. Decrease in incidence of colorectal cancer among individuals 50 years or older following recommendations for population-based screening Caitlin. Clin Gastroenterol Hepatol. 2017;15:903–909.
Bailey CE, Hu C-Y, You YN, et al. Increasing disparities in age-related incidence of colon and rectal cancer in the United States, 1975–2010. JAMA Surg. 2015;70:773–779.
Pischon T, Lahmann PH, Boeing H, et al. Body size and risk of colon and rectal cancer in the European Prospective Investigation Into Cancer and Nutrition (EPIC). J Natl Cancer Inst. 2006;98:920–931.
Giovannucci E, Ascherio A, Rimm EB, Colditz GA, Stampfer MJ, Willett WC. Physical activity, obesity, and risk for colon cancer and adenoma in men. Ann Intern Med. 1995;122:327–334.
Hong SN, Kim JH, Choe WH, Han HS. Prevalence and risk of colorectal neoplasms in asymptomatic, average-risk screenees 40 to 49 years of age. Gastrointest Endosc. 2010;72:480–489.
Liu P-H, Wu K, Ng K, et al. Association of obesity with risk of early-onset colorectal cancer among women. JAMA Oncol. 2019;63310:37–44.
Martínez ME, Giovannucci E, Spiegelman D, Hunter DJ, Willett WC, Colditz GA. Leisure-time physical activity, body size, and colon cancer in women. J Natl Cancer Inst. 1997;89:948–955.
Kim NH, Jung YS, Park DI, Sohn CI. Prevalence of and risk factors for colorectal neoplasia in asymptomatic young adults (20–39 years old). Clin Gastroenterol Hepatol. 2019;17:115–122.
Hales CM, Fryar CD, Carroll MD, Freedman DS, Ogden CL. Trends in obesity and severe obesity prevalence in US youth and adults by sex and age, 2007-2008 to 2015-2016. JAMA. 2018;319(16):1723–1725.
Ward ZJ, Bleich SN, Cradock AL, et al. Projected U.S. state-level prevalence of adult obesity and severe obesity. N Engl J Med. 2019;381:2440–2450.
Yosuke I, Bo Q, Jennifer P, Rebeccah S, Penny G. Epidemiology of obesity in adults: latest trends. Curr Obes Rep. 2018;7:276–288.
IBM Corporation. The IBM Explorys platform. [Internet]. [cited 2020 Aug 1]
NIH Library of Medicine. Overview of SNOMED CT [Internet]. [cited 2020 Aug 1].
Kaelber DC, Foster W, Gilder J, Love TE, Jain AK. Patient characteristics associated with venous thromboembolic events: a cohort study using pooled electronic health record data. J Am Med Inform Assoc. 2012;19:965–972.
Martinez-Useros J, Garcia-Foncillas J. Obesity and colorectal cancer: molecular features of adipose tissue. J Transl Med. 2016;14:21.
Kim NH, Jung YS, Yang H-J, et al. Prevalence of and risk factors for colorectal neoplasia in asymptomatic young adults (20–39 years old). Clin Gastroenterol Hepatol Off Clin Pract J Am Gastroenterol Assoc. 2019;17:115–122.
Executive summary. Obes Res. 1998;6:51S–179S.
Martınez E, Giovannucci E, Spiegelman D, Hunter DJ, Willett WC, Colditz GA. Leisure-time physical activity, body size, and colon cancer in women. J Natl Cancer Inst. 1997;89:944–955.
United States Census Bureau. Quick facts United States [Internet]. [cited 2020 Aug 23].
González N, Prieto I, Del Puerto-Nevado L, et al. 2017 update on the relationship between diabetes and colorectal cancer: epidemiology, potential molecular mechanisms and therapeutic implications. Oncotarget. 2017;8:18456–18485.
de Kort S, Masclee AAM, Sanduleanu S, et al. Higher risk of colorectal cancer in patients with newly diagnosed diabetes mellitus before the age of colorectal cancer screening initiation. Sci Rep. 2017;7:46527.
Hu FB, Manson JE, Liu S, et al. Prospective study of adult onset diabetes mellitus (type 2) and risk of colorectal cancer in women. J Natl Cancer Inst. 1999;91:542–547.
Seretis A, Cividini S, Markozannes G, Tseretopoulou X, Lopez DS, Ntzani EE, et al. Association between blood pressure and risk of cancer development: a systematic review and meta-analysis of observational studies. Sci Rep. 2019;9(1):8565.
Pakiet A, Kobiela J, Stepnowski P, Sledzinski T, Mika A. Changes in lipids composition and metabolism in colorectal cancer: a review. Lip Health Dis. 2019;18:29.
Yao X, Tian Z. Dyslipidemia and colorectal cancer risk: a meta-analysis of prospective studies. Cancer Causes Control. 2015;26:257–268.
Henry J Kaiser Family Foundation. Overweight and obesity rates for adults by race/ethnicity. Kaiser Family Foundation analysis of the Centers for Disease Control and Prevention (CDC)’s Behavioral Risk Factor Surveillance System (BRFSS) 2013–2017 Survey Results [Internet]. [cited 2020 Feb 8].
Ladabaum U, Mannalithara A, Myer PASG. Obesity, abdominal obesity, physical activity, and caloric intake in U.S. adults: 1988–2010. Am J Med. 2015;127:717–727.
Stokes A, Ni Y, Preston SH. Prevalence and trends in lifetime obesity in the U.S., 1988–2014. Am J Prev Med. 2018;53:567–575.
Siegel RL, Miller KD, Jemal A. Cancer statistics, 2018. CA Cancer J Clin. 2018;68:7–30.
Gausman V, Dornblaser D, Anand S, Hayes RB, O’Connell K, Du M, et al. Risk factors associated with early-onset colorectal cancer. Clin Gastroenterol Hepatol. 2019. https://doi.org/10.1016/j.cgh.2019.10.009.
Low EE, Demb J, Liu L, et al. Risk factors for early-onset colorectal cancer. Gastroenterology. 2020;S0016-5085:30016.
Yeo H, Betel D, Abelson JS, Zheng XE, Yantiss R, Shah MA. Early-onset colorectal cancer is distinct from traditional colorectal cancer. Clin Colorectal Cancer. 2017;16:293–299.
Yantiss RK, Goodarzi M, Zhou XK, et al. Clinical, pathologic, and molecular features of early-onset colorectal carcinoma. Am J Surg Pathol. 2009;33:572–582.
Colorectal Cancer Alliance. Young-onset colorectal cancer survey report [Internet]. 2018. [cited 2020 Feb 8].
Rex DK, Boland CR, Dominitz JA, et al. Colorectal cancer screening: recommendations for physicians and patients from the U.S. Multi-Society Task Force on Colorectal Cancer. Am J Gastroenterol. 2017;153:307–323.
Wolf AMD, Fontham ETH, Church TR, et al. Colorectal cancer screening for average-risk adults: 2018 guideline update from the American Cancer Society. CA Cancer J Clin. 2018;68:250–281.
Glover M, Mansoor E, Panhwar M, Parasa S, Cooper GS. Epidemiology of colorectal cancer in average risk adults 20–39 years of age: a population-based national study. Dig Dis Sci. 2019;64:3602–3609. https://doi.org/10.1007/s10620-019-05690-8.
U.S. Cancer Statistics Working Group. U.S. Cancer Statistics Data Visualizations Tool, based on 2019 submission data (1999–2017): U.S. Department of Health and Human Services, Centers for Disease Control and Prevention and National Cancer Institute [Internet]. [cited 2020 Aug 23].
Funding
None.
Author information
Authors and Affiliations
Contributions
AE, JS and GS contributed to the conception and design of the study. AE collected data. AGE and SMJ analyzed and interpreted the data. AE and JS wrote the initial draft. All authors contributed, revised and approved the final draft.
Corresponding author
Ethics declarations
Conflict of interest
None.
Additional information
Publisher's Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Electronic supplementary material
Below is the link to the electronic supplementary material.
Rights and permissions
About this article
Cite this article
Elangovan, A., Skeans, J., Landsman, M. et al. Colorectal Cancer, Age, and Obesity-Related Comorbidities: A Large Database Study. Dig Dis Sci 66, 3156–3163 (2021). https://doi.org/10.1007/s10620-020-06602-x
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s10620-020-06602-x