Abstract
Objective
This study aimed to evaluate the long-term efficacy of peroral endoscopic myotomy (POEM) for patients with achalasia.
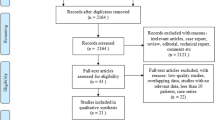
Methods
Prospective data collected from 115 patients (median age 45 years; interquartile range 34–57) with achalasia who underwent POEM at the First Affiliated Hospital of ZheJiang Chinese Medical University with a median follow-up of 36 months were retrospectively analyzed. The Eckardt score and lower esophageal sphincter pressure changes were analyzed, and the gastroesophageal reflux was observed.
Results
During the final follow-up, the mean Eckardt score reduced from 7.5 ± 1.9 preoperatively to 2.3 ± 1.4 after 1 month of surgery (P < 0.001). Treatment success was observed in 91.3% [confidence interval (CI) 86.2–96.4], 90.3% (CI 84.8–95.8), 89.0% (CI 83.1–94.9), 83.7% (CI 75.7–91.7), and 80.1% (CI 69.7–90.5) of patients after 12, 24, 36, 48, and 60 months, respectively. A total of 16 (13.9%) failures occurred. Four patients were nonresponders (failure within 3 months), eight had an early recurrence (between 3 months and 3 years), and four had a late recurrence (after 3 years). Further, 21 (20.6%) patients had symptoms of reflux during the two-year follow-up. Only one patient with symptomatic reflux was newly added during the subsequent three-year follow-up. Moreover, 71 (61.7%) patients underwent gastroscopy after POEM, and 13 (18.3%) patients were diagnosed with reflux esophagitis.
Conclusion
POEM is safe and effective in treating achalasia and has a favorable long-term efficacy.

Similar content being viewed by others
References
Boeckxstaens GE, Giovanni Z, Richter JE. Achalasia. Lancet. 2014;383:83–93.
Bello B, Herbella FA, Patti MG. Evolution of the minimally invasive treatment of esophageal achalasia. World J Surg. 2011;35:1442–1446.
Pasricha PJ, Hawari R, Ahmed I, et al. Submucosal endoscopic esophageal myotomy: a novel experimental approach for the treatment of achalasia. Endoscopy. 2007;39:761–764.
Perretta S, Dallemagne B, Allemann P, et al. Multimedia manuscript. Heller myotomy and intraluminal fundoplication: a NOTES technique. Surg Endosc. 2010;24:2904.
Inoue H, Minami H, Kobayashi Y, et al. Peroral endoscopic myotomy (POEM) for esophageal achalasia. Endoscopy. 2010;42:265–271.
Von Renteln D, Fuchs KH, Fockens P, et al. Peroral endoscopic myotomy for the treatment of achalasia: an international prospective multicenter study. Gastroenterology. 2013;145:309–311.
Ramchandani M, Nageshwar Reddy D, Darisetty S, et al. Peroral endoscopic myotomy for achalasia cardia: Treatment analysis and follow up of over 200 consecutive patients at a single center. Dig Endosc. 2016;28:19–26.
Inoue H, Sato H, Ikeda H, et al. Per-oral endoscopic myotomy: a series of 500 patients. J Am Coll Surg. 2015;221:256–264.
Guo H, Yang H, Zhang X, et al. Long-term outcomes of peroral endoscopic myotomy for patients with achalasia: a retrospective single-center study. Dis Esophagus. 2017;1:1–6.
Teitelbaum EN, Dunst CM, Reavis KM, et al. Clinical outcomes five years after POEM for treatment of primary esophageal motility disorders. Surg Endocr. 2018;32:421–427.
Bin L, Meng L, Yue H, et al. Effect of peroral esophageal myotomy for achalasia treatment: a Chinese study. World J Gastroenterol. 2015;21:5622–5629.
Hu Y, Li M, Lu B, et al. Esophageal motility after peroral endoscopic myotomy for achalasia. J Gastroenterol. 2016;51:458–464.
Crespin OM, Liu LWC, Parmar A, et al. Safety and efficacy of POEM for treatment of achalasia: a systematic review of the literature. Surg Endosc. 2017;31:2187–2201.
Eckardt VF. Clinical presentations and complications of achalasia. Gastrointest Endosc Clin N Am. 2001;11:281.
Eckardt VF, Aignherr C, Bernhard G. Predictors of outcome in patients with achalasia treated by pneumatic dilation. Gastroenterology. 1992;103:1732–1738.
Boeckxstaens GE, Annese V, des Varannes SB, et al. Pneumatic dilation versus laparoscopic Heller’s myotomy for idiopathic achalasia. N Engl J Med. 2011;364:1807–1816.
Li QL, Wu QN, Zhang XC, et al. Outcomes of per-oral endoscopic myotomy for treatment of esophageal achalasia with a median follow-up of 49 months. Gastrointest Endosc. 2018;87:1405–1412.
Herbella FA, Armijo PR, Patti MG. A pictorial presentation of 3.0 Chicago Classification for esophageal motility disorders. Einstein. 2016;14:439–442.
Jan M, Hana S, Zuzana V, et al. Per-oral endoscopic myotomy (POEM): mid-term efficacy and safety. Surg Endosc. 2018;32:1293–1302.
Werner YB, Costamagna G, Swanström LL, et al. Clinical response to peroral endoscopic myotomy in patients with idiopathic achalasia at a minimum follow-up of 2 years. Gut. 2015;65:899.
Ngamruengphong S, Inoue H, Chiu PW, et al. Long-term outcomes of per-oral endoscopic myotomy in patients with achalasia with a minimum follow-up of 2 years: an international multicenter study. Gastrointest Endosc. 2017;85:927.
Moonen A, Annese V, Belmans A, et al. Long-term results of the European achalasia trial: a multicentre randomised controlled trial comparing pneumatic dilation versus laparoscopic Heller myotomy. Gut. 2016;65:732.
Greene CL, Chang EJ, Oh DS, et al. High resolution manometry sub-classification of achalasia: does it really matter? Surg Endosc. 2015;29:1363.
Wu QN, Xu XY, Zhang XC, et al. Submucosal fibrosis in achalasia patients is a rare cause of aborted peroral endoscopic myotomy procedures. Endoscopy. 2017;49:736–744.
Zaninotto G, Costantini M, Rizzetto C, et al. Four hundred laparoscopic myotomies for esophageal achalasia. Ann Surg. 2008;248:986–993.
Patti MG, Molena D, Fisichella PM, et al. Laparoscopic Heller myotomy and Dor fundoplication for achalasia: analysis of successes and failures. Arch Surg. 2001;136:870–877.
Hernández OM, Martinez González MA, Blancas JV, et al. Long-term quality of life after peroral endoscopic myotomy remains compromised in patients with achalasia type III. Endoscopy. 2017;49:1209–1218.
Sharata AM, Dunst CM, Pescarus R, et al. Peroral endoscopic myotomy (POEM) for esophageal primary motility disorders: analysis of 100 consecutive patients. J Gastrointest Surg. 2015;19:161–170.
Shiwaku H, Inoue H, Yamashita K, et al. Peroral endoscopic myotomy for esophageal achalasia: outcomes of the first over 100 patients with short-term follow-up. Surg Endosc. 2016;30:4817–4826.
Ren Y, Tang X, Chen Y, et al. Pre-treatment Eckardt score is a simple factor for predicting one-year peroral endoscopic myotomy failure in patients with achalasia. Surg Endosc. 2017;31:3234–3241.
Repici A, Fuccio L, Maselli R, et al. Gastroesophageal reflux disease after per-oral endoscopic myotomy as compared with Heller’s myotomy with fundoplication: a systematic review with meta-analysis. Gastrointest Endosc. 2018;87:934–943.
Hajar N, Castell DO, Ghomrawi H, et al. Impedance pH confirms the relationship between GERD and BMI. Dig Dis Sci. 2012;57:1875–1879.
Viazis N, Karamanolis GP, Anastasiou J, et al. Refractory GERD: increased body mass index is associated with persisting acid exposure but not hypersensitive esophagus or functional heartburn. Eur J Gastroenterol Hepatol. 2013;25:1450–1455.
Acknowledgments
The authors thank Kejia Zhao and Xianjing Zhao for assisting in the preparation of this manuscript.
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
Conflicts of interest
The authors declare no conflicts of interest.
Rights and permissions
About this article
Cite this article
He, C., Li, M., Lu, B. et al. Long-Term Efficacy of Peroral Endoscopic Myotomy for Patients with Achalasia: Outcomes with a Median Follow-Up of 36 Months. Dig Dis Sci 64, 803–810 (2019). https://doi.org/10.1007/s10620-018-5373-0
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s10620-018-5373-0