Abstract
Background
Peroral endoscopic myotomy (POEM) is a novel operation for the treatment of achalasia and other esophageal motility disorders. While POEM has shown excellent short-term safety and efficacy, the long-term symptomatic outcomes after the procedure are unknown.
Methods
Patients from a single center that underwent POEM for treatment of esophageal motility orders and were greater than 5 years removed from their operation were studied. Patients were contacted to assess current symptoms and encouraged to undergo repeat endoscopy for objective follow-up.
Results
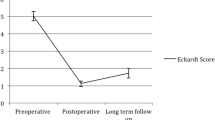
Thirty-six patients underwent POEM from October, 2010 to February, 2012 and current symptom scores were obtained from 29 patients at median 65-month follow-up. In the 23 patients with achalasia, Eckardt scores were significantly improved from preoperative baseline (mean current 1.7 vs. preoperative 6.4, p < 0.001). Nineteen patients (83%) with achalasia had a symptomatic success (Eckardt ≤3) and none required retreatment for symptoms. Eckardt scores were dramatically improved at 6 months and maintained at 2 years; however, there was a small but significant worsening of symptoms between 2 and 5-years. Of the five patients with EGJ outflow obstruction, all had current Eckardt scores ≤3 but two needed reintervention for persistent or recurrent symptoms, one with a laparoscopic Heller myotomy and another with an endoscopic cricomyotomy and proximal esophageal myotomy extension. At 6-month follow-up, repeat manometry showed decreased EGJ relaxation pressures and esophagram demonstrated improved emptying. 24-h pH monitoring showed abnormal distal esophageal acid exposure in 38% of patients. Fifteen patients underwent endoscopy at 5-years, revealing erosive esophagitis in two (13%), new hiatal hernia in two, and new non-dysplastic Barrett’s esophagus in one. The patient with Barrett’s underwent a subsequent laparoscopic hiatal hernia repair and Toupet fundoplication.
Conclusions
POEM resulted in a successful palliation of symptoms in the majority of patients after 5 years, though these results emphasize the importance of long-term follow-up in all patients.

Similar content being viewed by others
References
Boeckxstaens GE, Zaninotto G, Richter JE (2014) Achalasia. Lancet 383:83–93
Yaghoobi M, Mayrand S, Martel M, Roshan-Afshar I, Bijarchi R, Barkun A (2013) Laparoscopic Heller’s myotomy versus pneumatic dilation in the treatment of idiopathic achalasia: a meta-analysis of randomized, controlled trials. Gastrointest Endosc 78:468–475
Moonen A, Annese V, Belmans A, Bredenoord AJ, Bruley des Varannes S, Costantini M, Dousset B, Elizalde JI, Fumagalli U, Gaudric M, Merla A, Smout AJ, Tack J, Zaninotto G, Busch OR, Boeckxstaens GE (2016) Long-term results of the European achalasia trial: a multicentre randomised controlled trial comparing pneumatic dilation versus laparoscopic Heller myotomy. Gut 65:732–739
Schoenberg MB, Marx S, Kersten JF, Rosch T, Belle S, Kahler G, Vassiliou MC, Luth S, von Renteln D (2013) Laparoscopic Heller myotomy versus endoscopic balloon dilatation for the treatment of achalasia: a network meta-analysis. Ann Surg 258:943–952
Sawas T, Ravi K, Geno DM, Enders F, Pierce K, Wigle D, Katzka DA (2017) The course of achalasia one to four decades after initial treatment. Aliment Pharmacol Ther 45:553–560
Vela MF, Richter JE, Khandwala F, Blackstone EH, Wachsberger D, Baker ME, Rice TW (2006) The long-term efficacy of pneumatic dilatation and Heller myotomy for the treatment of achalasia. Clin Gastroenterol Hepatol 4:580–587
Inoue H, Minami H, Kobayashi Y, Sato Y, Kaga M, Suzuki M, Satodate H, Odaka N, Itoh H, Kudo S (2010) Peroral endoscopic myotomy (POEM) for esophageal achalasia. Endoscopy 42:265–271
Bhayani NH, Kurian AA, Dunst CM, Sharata AM, Rieder E, Swanstrom LL (2014) A comparative study on comprehensive, objective outcomes of laparoscopic Heller myotomy with per-oral endoscopic myotomy (POEM) for achalasia. Ann Surg 259:1098–1103
von Renteln D, Inoue H, Minami H, Werner YB, Pace A, Kersten JF, Much CC, Schachschal G, Mann O, Keller J, Fuchs KH, Rosch T (2012) Peroral endoscopic myotomy for the treatment of achalasia: a prospective single center study. Am J Gastroenterol 107:411–417
Hungness ES, Sternbach JM, Teitelbaum EN, Kahrilas PJ, Pandolfino JE, Soper NJ (2016) Per-oral endoscopic myotomy (POEM) after the learning curve: durable long-term results with a low complication rate. Ann Surg 264:508–517
Werner YB, Costamagna G, Swanstrom LL, von Renteln D, Familiari P, Sharata AM, Noder T, Schachschal G, Kersten JF, Rosch T (2016) Clinical response to peroral endoscopic myotomy in patients with idiopathic achalasia at a minimum follow-up of 2 years. Gut 65:899–906
Inoue H, Sato H, Ikeda H, Onimaru M, Sato C, Minami H, Yokomichi H, Kobayashi Y, Grimes KL, Kudo SE (2015) Per-oral endoscopic myotomy: a series of 500 patients. J Am Coll Surg 221:256–264
Eckardt VF (2001) Clinical presentations and complications of achalasia. Gastrointest Endosc Clin N Am 11:281–292
Kahrilas PJ, Bredenoord AJ, Fox M, Gyawali CP, Roman S, Smout AJ, Pandolfino JE, International High Resolution Manometry Working G (2015) The Chicago classification of esophageal motility disorders, v3.0. Neurogastroenterol Motil 27:160–174
Swanstrom LL, Rieder E, Dunst CM (2011) A stepwise approach and early clinical experience in peroral endoscopic myotomy for the treatment of achalasia and esophageal motility disorders. J Am Coll Surg 213:751–756
Boeckxstaens GE, Annese V, des Varannes SB, Chaussade S, Costantini M, Cuttitta A, Elizalde JI, Fumagalli U, Gaudric M, Rohof WO, Smout AJ, Tack J, Zwinderman J, Zaninotto G, Busch OR, European Achalasia Trial I (2011) Pneumatic dilation versus laparoscopic Heller’s myotomy for idiopathic achalasia. N Engl J Med 364:1807–1816
Jones R, Junghard O, Dent J, Vakil N, Halling K, Wernersson B, Lind T (2009) Development of the GerdQ, a tool for the diagnosis and management of gastro-oesophageal reflux disease in primary care. Aliment Pharmacol Ther 30:1030–1038
Zaninotto G, Costantini M, Rizzetto C, Zanatta L, Guirroli E, Portale G, Nicoletti L, Cavallin F, Battaglia G, Ruol A, Ancona E (2008) Four hundred laparoscopic myotomies for esophageal achalasia: a single centre experience. Ann Surg 248:986–993
Rawlings A, Soper NJ, Oelschlager B, Swanstrom L, Matthews BD, Pellegrini C, Pierce RA, Pryor A, Martin V, Frisella MM, Cassera M, Brunt LM (2012) Laparoscopic Dor versus Toupet fundoplication following Heller myotomy for achalasia: results of a multicenter, prospective, randomized-controlled trial. Surg Endosc 26:18–26
Familiari P, Gigante G, Marchese M, Boskoski I, Tringali A, Perri V, Costamagna G (2016) Peroral endoscopic myotomy for esophageal achalasia: outcomes of the first 100 patients with short-term follow-up. Ann Surg 263:82–87
Gholoum S, Feldman LS, Andrew CG, Bergman S, Demyttenaere S, Mayrand S, Stanbridge DD, Fried GM (2006) Relationship between subjective and objective outcome measures after Heller myotomy and Dor fundoplication for achalasia. Surg Endosc 20:214–219
Okeke FC, Raja S, Lynch KL, Dhalla S, Nandwani M, Stein EM, Chander Roland B, Khashab MA, Saxena P, Kumbhari V, Ahuja NK, Clarke JO (2017) What is the clinical significance of esophagogastric junction outflow obstruction? evaluation of 60 patients at a tertiary referral center. Neurogastroenterol Motil. doi:10.1111/nmo.13061
Perez-Fernandez MT, Santander C, Marinero A, Burgos-Santamaria D, Chavarria-Herbozo C (2016) Characterization and follow-up of esophagogastric junction outflow obstruction detected by high resolution manometry. Neurogastroenterol Motil 28:116–126
Teitelbaum EN, Soper NJ, Arafat FO, Santos BF, Kahrilas PJ, Pandolfino JE, Hungness ES (2014) Analysis of a learning curve and predictors of intraoperative difficulty for peroral esophageal myotomy (POEM). J Gastrointest Surg 18:92–98 discussion 8–9
Kurian AA, Dunst CM, Sharata A, Bhayani NH, Reavis KM, Swanstrom LL (2013) Peroral endoscopic esophageal myotomy: defining the learning curve. Gastrointest Endosc 77:719–725
Acknowledgements
The authors would like to acknowledge Angie Gill, RN, and Lisa Leeth for their help coordinating the clinical aspects of this study.
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
Disclosures
Dr. Reavis is a consultant for Boston Scientific, Endogastric Solutions, and Stryker, and receives teaching or advisory honoraria from Ethicon, Mederi, Gore, and Apollo. Dr. DeMeester is a consultant for Bard. Dr. Swanstrom is on the scientific advisory boards of Olympus and Boston Scientific. These disclosures are not related to the current study. Drs. Teitelbaum, Dunst, Sharata, and Ward have no disclosures or conflicts of interest to report.
Rights and permissions
About this article
Cite this article
Teitelbaum, E.N., Dunst, C.M., Reavis, K.M. et al. Clinical outcomes five years after POEM for treatment of primary esophageal motility disorders. Surg Endosc 32, 421–427 (2018). https://doi.org/10.1007/s00464-017-5699-2
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s00464-017-5699-2