Abstract
Background and Objectives
There are several published studies examining the major complications (bleeding and perforation) of colon endoscopic submucosal dissection (ESD). However, little is known about the other complications, such as post-ESD coagulation syndrome (CS). The aims of this study were to evaluate the prevalence and the clinical features of CS after colon ESD.
Methods
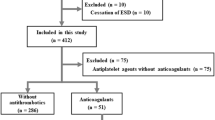
There were 183 cases treated with ESD for either a colorectal laterally spreading tumor or a polypoid mass in Konkuk University Medical Center. There were 151 cases enrolled in this study after excluding patients with perforation, bleeding, nonlifting sign, or nonneoplastic lesions. Patients with a fever above 37.7 °C, abdominal pain, and localized tenderness after ESD without macro- or microperforation, regardless of the symptoms of peritoneal irritation, were deemed as showing post-colon ESD CS.
Results
There were 151 cases enrolled in this study, and 13 patients (8.6 %) showed CS after colorectal ESD. There were no differences in the demographic and endoscopic characteristics between the patients with CS and those without CS. The mean hospitalization stay was 3.0 ± 0.3 days longer in the CS (+) group (6.9 ± 1.9 days) than that in the CS (−) group (3.9 ± 1.6 days) (p = 0.001). All patients with CS were treated with conservative, nonsurgical management, such as fasting and intravenous antibiotics.
Conclusions
The rate of post-ESD CS was less than 9 % in this study. Although CS occurred, all of the patients with CS showed a favorable progression within 1 week.


Similar content being viewed by others
References
Repici A, Hassan C, Carlino A, et al. Endoscopic submucosal dissection in patients with early esophageal squamous cell carcinoma: results from a prospective Western series. Gastrointest Endosc. 2010;71:715–721.
Repici A, Hassan C, De Paula, Pessoa D, et al. Efficacy and safety of endoscopic submucosal dissection for colorectal neoplasia: a systematic review. Endoscopy. 2012;44:137–150.
Tanaka S, Oka S, Kaneko I, et al. Endoscopic submucosal dissection for colorectal neoplasia: possibility of standardization. Gastrointest Endosc. 2007;66:100–107.
Nakamoto S, Sakai Y, Kasanuki J, et al. Indications for the use of endoscopic mucosal resection for early gastric cancer in Japan: a comparative study with endoscopic submucosal dissection. Endoscopy. 2009;41:746–750.
Nakamoto S, Sakai Y, Kasanuki J, et al. Advantage of endoscopic submucosal dissection compared with EMR for early gastric cancer. Gastrointest Endosc. 2006;64:877–883.
Hagel AF, Boxberger F, Dauth W, Kessler HP, Neurath MF, Raithel M. Colonoscopy-associated perforation: a 7-year survey of in-hospital frequency, treatment and outcome in a German university hospital. Colorectal Dis. 2012;14:1121–1125.
Kim ES, Cho KB, Park KS, et al. Factors predictive of perforation during endoscopic submucosal dissection for the treatment of colorectal tumors. Endoscopy. 2011;43:573–578.
Yoon JY, Kim JH, Lee JY, et al. Clinical outcomes for patients with perforations during endoscopic submucosal dissection of laterally spreading tumors of the colorectum. Surg Endosc. 2013;27:487–493.
Onogi F, Araki H, Ibuka T, et al. “Transmural air leak”: a computed tomographic finding following endoscopic submucosal dissection of gastric tumors. Endoscopy. 2010;42:441–447.
Cha JM, Lim KS, Lee SH, et al. Clinical outcomes and risk factors of post-polypectomy coagulation syndrome: a multicenter, retrospective, case-control study. Endoscopy. 2013;45:202–207.
Waye JD, Lewis BS, Yessayan S. Colonoscopy: a prospective report of complications. J Clin Gastroenterol. 1992;15:347–351.
Waye JD, Kahn O, Auerbach ME. Complications of colonoscopy and flexible sigmoidoscopy. Gastrointest Endosc Clin N Am. 1996;6:343–377.
Christie JP, Marrazzo J 3rd. “Mini-perforation” of the colon–not all postpolypectomy perforations require laparotomy. Dis Colon Rectum.. 1991;34:132–135.
Lee H, Cheoi KS, Chung H, et al. Clinical features and predictive factors of coagulation syndrome after endoscopic submucosal dissection for early gastric neoplasm. Gastric Cancer. 2012;15:83–90.
Tanaka S, Oka S, Chayama K. Colorectal endoscopic submucosal dissection: present status and future perspective, including its differentiation from endoscopic mucosal resection. J Gastroenterol. 2008;43:641–651.
Fujishiro M, Yahagi N, Kakushima N, et al. Outcomes of endoscopic submucosal dissection for colorectal epithelial neoplasms in 200 consecutive cases. Clin Gastroenterol Hepatol. 2007;5:678–683.
Saito Y, Uraoka T, Yamaguchi Y, et al. A prospective, multicenter study of 1111 colorectal endoscopic submucosal dissections (with video). Gastrointest Endosc. 2010;72:1217–1225.
Kobayashi N, Saito Y, Uraoka T, Matsuda T, Suzuki H, Fujii T. Treatment strategy for laterally spreading tumors in Japan: before and after the introduction of endoscopic submucosal dissection. J Gastroenterol Hepatol. 2009;24:1387–1392.
Acknowledgments
This work was supported by Konkuk University Medical Center Research Grant 2012.
Conflict of interest
The authors declare that they have no conflict of interest.
Author information
Authors and Affiliations
Corresponding author
Rights and permissions
About this article
Cite this article
Hong, M.J., Kim, J.H., Lee, SY. et al. Prevalence and Clinical Features of Coagulation Syndrome After Endoscopic Submucosal Dissection for Colorectal Neoplasms. Dig Dis Sci 60, 211–216 (2015). https://doi.org/10.1007/s10620-014-3484-9
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s10620-014-3484-9