Abstract
Background and aims
The withdrawal of antithrombotic therapy from patients at high risk of thromboembolism is controversial. Previously, treatment with anticoagulants, such as warfarin and dabigatran, was recommended for heparin bridge therapy (HBT) during endoscopic submucosal dissection (ESD). However, HBT is associated with a high risk of bleeding during and after ESD. This study aimed to investigate the clinical outcomes of colorectal ESD in patients treated with warfarin and direct oral anticoagulants (DOAC).
Methods
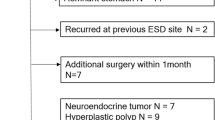
This study included 412 patients with superficial colorectal neoplasms that were resected by ESD between June 2010 and June 2018. The patients were classified into two groups: without antithrombotics (n = 286) and with anticoagulants (n = 51). The anticoagulants group was further divided into two groups: warfarin (n = 26) and DOAC (n = 25).
Results
Among all patients, delayed bleeding occurred in 35 (8.5% [35/412]) patients. The bleeding rate in the anticoagulants group (11.8% [6/51]) was higher than that in the group without antithrombotics (6.6% [19/286]), but the difference was not statistically significant (P = 0.240). The bleeding rate in the DOAC group (16.0% [4/25]) was higher than that in the warfarin group (7.7% [2/26]), but the difference was not statistically significant (P = 0.419). All delayed bleeding was successfully managed with endoscopic hemostasis. Thromboembolic events were not observed in any patients.
Conclusions
The bleeding rate with anticoagulants was relatively high. However, all bleeding events with anticoagulants were minor and clinically controllable. Colorectal ESD with DOAC and warfarin may be feasible and acceptable.

Similar content being viewed by others
Abbreviations
- BMI:
-
Body mass index
- CI:
-
Confidence interval
- CKD:
-
Chronic kidney disease
- DOAC:
-
Direct oral anticoagulants
- ESD:
-
Endoscopic submucosal dissection
- HBT:
-
Heparin bridge therapy
- INR:
-
International normalized ratio
- LST-G:
-
Laterally spreading tumor: granular type
- LST-NG:
-
Laterally spreading tumor: non-granular type
- OR:
-
Odds ratio
References
Saito Y, Uraoka T, Matsuda T, Emura F, Ikehara H, Mashimo Y, Kikuchi T, Fu KI, Sano Y, Saito D (2007) Endoscopic treatment of large superficial colorectal tumors: a case of 200 endoscopic submucosal dissections (with video). Gastrointest Endosc 66:966–973
Fujishiro M, Yahagi N, Kakushima N, Kodashima S, Muraki Y, Ono S, Yamamichi N, Tateishi A, Oka M, Ogura K, Kawabe T, Ichinose M, Omata M (2007) Outcomes of endoscopic submucosal dissection for colorectal epithelial neoplasms in 200 consecutive cases. Clin Gastroenterol Hepatol 5:678–683
Tanaka S, Oka S, Kaneko I, Hirata M, Mouri R, Kanao H, Yoshida S, Chayama K (2007) Endoscopic submucosal dissection for colorectal neoplasia: possibility of standardization. Gastrointest Endosc 66:100–107
Hotta K, Yamaguchi Y, Saito Y, Takao T, Ono H (2012) Current opinions for endoscopic submucosal dissection for colorectal tumors from our experiences: indications, technical aspects and complications. Dig Endosc 24:110–116
Saito Y, Uraoka T, Yamaguchi Y, Hotta K, Sakamoto N, Ikematsu H, Fukuzawa M, Kobayashi N, Nasu J, Michida T, Yoshida S, Ikehara H, Otake Y, Nakajima T, Matsuda T, Saito D (2010) A prospective multicenter study of 1111 colorectal endoscopic submucosal dissection (with video). Gastrointest Endosc 72:1217–1225
Ogasawara N, Yoshimine T, Noda H, Kondo Y, Izawa S, Shinmura T, Ebi M, Funaki Y, Sasaki M, Kasugai K (2016) Clinical risk factors for delayed bleeding after endoscopic submucosal dissection for colorectal tumors in Japanese patients. Eur J Gastroenterol Hepatol 28:1407–1414
Terasaki M, Tanaka S, Shigita K, Asayama N, Nishiyama S, Hayashi N, Nakadoi K, Oka S, Chayama K (2014) Risk factors for delayed bleeding after endoscopic submucosal dissection for colorectal neoplasms. Int J Colorectal Dis 29:877–882
Nakajima T, Saito Y, Tanaka S, Iishi H, Kudo SE, Ikematsu H, Igarashi M, Saitoh Y, Inoue Y, Kobayashi K, Hisasbe T, Matsuda T, Ishikawa H, Sugihara K (2013) Current status of endoscopic resection strategy for large, early colorectal reoplasia in Japan. Surg Endosc 27:3262–3270
Oka S, Tanaka S, Kanao H, Ishikawa H, Watanabe T, Igarashi M, Saito Y, Ikematsu H, Kobayashi K, Inoue Y, Yahagi N, Tsuda S, Simizu S, Iishi H, Yamano H, Kudo SE, Tsuruta O, Saito Y, Cho E, Fujii T, Sano Y, Nakamura H, Sugihara K, Muto T (2010) Current status in the occurrence of postoperative bleeding, perforation and residual/local recurrence during colonoscopic treatment in Japan. Dig Endosc 22:376–380
Probst A, Golger D, Anthuber M, Märkl B, Messmann H (2012) Endoscopic submucosal dissection in large sessile lesions of the rectosigmoid: learning curve in a European center. Endoscopy 44:660–667
Hurlstone DP, Atkinson R, Sanders DS, Thomson M, Cross SS, Brown S (2007) Achieving R0 resection in the colorectum using endoscopic submucosal dissection. Br J Surg 94:1536–1542
Fujimoto K, Fujishiro M, Kato M, Higuchi K, Iwakiri R, Sakamoto C, Uchiyama S, Kashiwagi A, Ogawa H, Murakami K, Mine T, Yoshino J, Kinoshita Y, Ichinose M, Matsui T, Japan Gastroenterological Endoscopy Society (2014) Guidelines for gastroenterological endoscopy in patients undergoing antithrombotic treatment. Dig Endosc 26:1–14
Yoshio T, Nishida T, Kawai N, Yuguchi K, Yamada T, Yabuta T, Komori M, Yamaguchi S, Kitamura S, Iijima H, Tsutsui S, Michida T, Mita E, Tsujii M, Takehara T (2013) Gastric ESD under heparin replacement at high-risk patients of thromboembolism is technically feasible but has a high risk of delayed bleeding: Osaka University ESD Study Group. Gastroenterol Res Pract 2013:365830
Harada H, Suehiro S, Murakami D, Shimizu T, Nakahara R, Katsuyama Y, Miyama Y, Tounou S, Hayasaka K (2017) Continuous use of low-dose warfarin for gastric endoscopic submucosal dissection: a prospective study. Endosc Int Open 5:E348–E353
Yoshio T, Tomida H, Iwasaki R, Horiuchi Y, Omae M, Ishiyama A, Hirasawa T, Yamamoto Y, Tsuchida T, Fujisaki J, Yamada T, Mita E, Ninomiya T, Michitaka K, Igarashi M (2017) Effect of direct oral anticoagulants on the risk of delayed bleeding after endoscopic submucosal dissection. Dig Endosc 29:686–694
Yamashita K, Oka S, Tanaka S, Boda K, Hirano D, Sumimoto K, Mizumoto T, Ninomiya Y, Tamaru Y, Shigita K, Hayashi N, Sanomura Y, Chayama K (2018) Use of anticoagulants increases risk of bleeding after colorectal endoscopic submucosal dissection. Endosc Int Open 6:E857–E864
Kato M, Uedo N, Hokimoto S, Ieko M, Higuchi K, Murakami K, Fujimoto K (2018) Guidelines for gastroenterological endoscopy in patients undergoing antithrombotic treatment: 2017 appendix on anticoagulants including direct oral anticoagulants. Dig Endosc 30:433–440
Connolly SJ, Ezekowitz MD, Yusuf S, Eikelboom J, Oldgren J, Parekh A, Pogue J, Reilly PA, Themeles E, Varrone J, Wang S, Alings M, Xavier D, Zhu J, Diaz R, Lewis BS, Darius H, Diener HC, Joyner CD, Wallentin L, RE-LY Steering Committee and Investigators (2009) Dabigatran versus warfarin in patients with atrial fibrillation. N Engl J Med 361:1139–1151
Patel MR, Mahaffey KW, Garg J, Pan G, Singer DE, Hacke W, Breithardt G, Halperin JL, Hankey GJ, Piccini JP, Becker RC, Nessel CC, Paolini JF, Berkowitz SD, Fox KA, Califf RM, ROCKET AF Investigators (2011) Rivaroxaban versus warfarin in nonvalvular atrial fibrillation. N Engl J Med 365:883–891
Granger CB, Alexander JH, McMurray JJ, Lopes RD, Hylek EM, Hanna M, Al-Khalidi HR, Ansell J, Atar D, Avezum A, Bahit MC, Diaz R, Easton JD, Ezekowitz JA, Flaker G, Garcia D, Geraldes M, Gersh BJ, Golitsyn S, Goto S, Hermosillo AG, Hohnloser SH, Horowitz J, Mohan P, Jansky P, Lewis BS, Lopez-Sendon JL, Pais P, Parkhomenko A, Verheugt FW, Zhu J, Wallentin L, ARISTOTLE Committees and Investigators (2011) Apixaban versus warfarin in patients with atrial fibrillation. N Engl J Med 365:981–992
Giugliano RP, Ruff CT, Braunwald E, Murphy SA, Wiviott SD, Halperin JL, Waldo AL, Ezekowitz MD, Weitz JI, Špinar J, Ruzyllo W, Ruda M, Koretsune Y, Betcher J, Shi M, Grip LT, Patel SP, Patel I, Hanyok JJ, Mercuri M, Antman EM, ENGAGE AF-TIMI 48 Investigators (2013) Edoxaban versus warfarin in patients with atrial fibrillation. N Engl J Med 369:2093–2104
Frost C, Wang J, Nepal S, Schuster A, Barrett YC, Mosqueda-Garcia R, Reeves RA, LaCreta F (2013) Apixaban, an oral direct, factor Xa inhibitor: single-dose safety, pharmacokinetics and pharmacodynamics in healthy subjects. Br J Clin Pharmacol 75:476–487
Anderson MA, Ben-Menachem T, Sl Gan, Appalaneni V, Banerjee S, Cash BD, Fisher L, Harrison ME, Fanelli RD, Fukami N, Ikenberry SO, Jain R, Khan K, Krinsky ML, Lichtenstein DR, Maple JT, Shen B, Strohmeyer L, Baron T, Dominitz JA (2009) Guideline: management of antithrombotic agents for endoscopic procedures. Gastrointest Endosc 70:1060–1070
Gage BF, Waterman AD, Shannon W, Boechler M, Rich MW, Radford MJ (2001) Validation of clinical classification schemes for predicting stroke: results from the National Registry of Atrial Fibrillation. JAMA 285:2864–2870
Go AS, Hylek EM, Chang Y, Phillips KA, Henault LE, Capra AM, Jensvold NG, Selby JV, Singer DE (2003) Anticoagulation therapy for stroke prevention in atrial fibrillation: how well do randomized trials translate into clinical practice? JAMA 290:2685–2692
Goldstein LB, Adams R, Alberts MJ, Appel LJ, Brass LM, Bushnell CD, Culebras A, Degraba TJ, Gorelick PB, Guyton JR, Hart RG, Howard G, Kelly-Hayes M, Nixon JV, Sacco RL (2006) Primary prevention of ischemic stroke: a guideline from the American Heart Association/American Stroke Association Stroke Council: cosponsored by the Atherosclerotic Peripheral Vascular Disease Interdisciplinary Working Group; Cardiovascular Nursing Council; Clinical Cardiology Council; Nutrition, Physical Activity, and Metabolism Council; and the Quality of Care and Outcomes Research Interdisciplinary Working Group: the American Academy of Neurology affirms the value of this guideline. Stroke 37:1583–1633
Austin PC (2009) Some methods of propensity-score matching had superior performance to others: results of an empirical investigation and Monte Carlo simulations. Biom J 51:171–184
Jaruvongvanich V, Prasitlumkum N, Assavapongpaiboon B, Suchartlikitwong S, Sanguankeo A, Upala S (2017) Risk factors for delayed colonic post-polypectomy bleeding: a systematic review and meta-analysis. Int J Colorectal Dis 32:1399–1406
Yanagisawa N, Nagata N, Watanabe K, Iida T, Hamada M, Kobayashi S, Shimbo T, Akiyama J, Uemura N (2018) Post-polypectomy bleeding and thromboembolism risks associated with warfarin vs direct oral anticoagulants. World J Gastroenterol 24:1540–1549
Author information
Authors and Affiliations
Contributions
HH wrote the manuscript and analyzed the data. AY gave final approval of the manuscript. All other authors collected data, reviewed the manuscript, and made revisions.
Corresponding author
Ethics declarations
Disclosures
Hideaki Harada, Ryotaro Nakahara, Daisuke Murakami, Satoshi Suehiro, Takuya Nagasaka, Tetsuro Ujihara, Ryota Sagami, Yasushi Katsuyama, Kenji Hayasaka, Shigetaka Tounou, and Yuji Amano declare that they have no conflicts of interest or financial ties to disclose.
Ethical approval
This study was reviewed and approved by the New Tokyo Hospital Institutional Review Committee.
Informed consent
The patient provided informed written consent.
Additional information
Publisher's Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Rights and permissions
About this article
Cite this article
Harada, H., Nakahara, R., Murakami, D. et al. The effect of anticoagulants on delayed bleeding after colorectal endoscopic submucosal dissection. Surg Endosc 34, 3330–3337 (2020). https://doi.org/10.1007/s00464-019-07101-5
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s00464-019-07101-5