Abstract
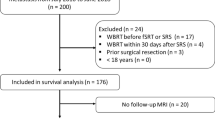
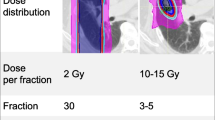
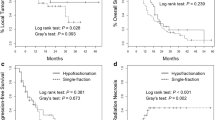
Stereotactic radiosurgery (SRS) is an effective treatment option for multiple brain metastases (BMs). Modern mono-isocentric techniques allow the delivery of multiple stereotactic courses, in the event of intracranial failure. Nevertheless, limited data on effectiveness and toxicity have been reported in comparison to WBRT. Aim of this retrospective matched-pair analysis was to compare patients affected by limited BMs treated with multiple SRS courses using a mono-isocentric, non-coplanar technique (HyperArc™, Varian Medical System) to upfront WBRT. One hundred and two patients accounting for 677 BMs were treated with HyperArc™. In case of further intracranial progression, 44 treatment courses of 201 metastases in 19 patients, were treated by subsequent HyperArc™ courses. This population was matched with 38 patients treated with WBRT. The median BMs number was 4 (range 2–10) for HyperArc™ and 5 (range 2–10) for WBRT. Overall survival (OS) and toxicity were evaluated. The median follow-up was 9 months (range 3–40 months). The median OS was not reached (range 5–22 months) for HyperArc™ patients and 8 months (range 3–40 months) for WBRT patients, while the 1-year OS was 77% and 34.6% for HyperArc™ and WBRT, respectively (p = 0.001; HR 4.77, 95% CI 1.62–14.00). There was one case of radionecrosis. HyperArc™ is an effective and safe technique for the treatment of multiple BMs. In selected cases of intracranial oligorecurrence, further subsequent courses can be safely delivered with the same technical approach. Moreover, in patients with a limited number of BMs, SRS showed an improved survival outcome when compared to WBRT.

Similar content being viewed by others
References
Ebner DK, Gorovets D, Rava P, Cielo D, Kinsella TJ, DiPetrillo TA, Hepel JT (2017) Patients with long-term control of systemic disease are a favorable prognostic group for treatment of brain metastases with stereotactic radiosurgery alone. World Neurosurg 98:266–272. https://doi.org/10.1016/j.wneu.2016.11.010
Dempke WC, Edvardsen K, Lu S, Reinmuth N, Reck M, Inoue A (2015) Brain metastases in NSCLC - are TKIs changing the treatment strategy? Anticancer Res 35(11):5797–5806
Yamamoto M, Kawabe T, Sato Y, Higuchi Y, Nariai T, Watanabe S, Kasuya H (2014) Stereotactic radiosurgery for patients with multiple brain metastases: a case-matched study comparing treatment results for patients with 2-9 versus 10 or more tumors. J Neurosurg 121(Suppl_2):16–25. https://doi.org/10.3171/2014.8.GKS141421
Hughes RT, McTyre ER, LeCompte M, Cramer CK, Munley MT, Laxton AW, Tatter SB, Ruiz J, Pasche B, Watabe K, Chan MD (2018) Clinical outcomes of upfront stereotactic radiosurgery alone for patients with 5 to 15 brain metastases. Neurosurgery. https://doi.org/10.1093/neuros/nyy276
Lehrer EJ, Peterson JL, Zaorsky NG, Brown PD, Sahgal A, Chiang VL, Chao ST, Sheehan JP, Trifiletti DM (2019) Single versus multifraction stereotactic radiosurgery for large brain metastases: an international meta-analysis of 24 trials. Int J Radiat Oncol Biol Phys 103(3):618–630. https://doi.org/10.1016/j.ijrobp.2018.10.038
Habets EJ, Dirven L, Wiggenraad RG, Verbeek-de Kanter A, Lycklama À Nijeholt GJ, Zwinkels H, Klein M, Taphoorn MJ (2016) Neurocognitive functioning and health-related quality of life in patients treated with stereotactic radiotherapy for brain metastases: a prospective study. Neuro Oncol 18(3):435–444. https://doi.org/10.1093/neuonc/nov186
Yamamoto M, Serizawa T, Higuchi Y, Sato Y, Kawagishi J, Yamanaka K, Shuto T, Akabane A, Jokura H, Yomo S, Nagano O, Aoyama H (2017) A multi-institutional prospective observational study of stereotactic radiosurgery for patients with multiple brain metastases (JLGK0901 Study Update): irradiation-related complications and long-term maintenance of mini-mental state examination scores. Int J Radiat Oncol Biol Phys 99(1):31–40. https://doi.org/10.1016/j.ijrobp.2017.04.037
Chang EL, Wefel JS, Hess KR, Allen PK, Lang FF, Kornguth DG, Arbuckle RB, Swint JM, Shiu AS, Maor MH, Meyers CA (2009) Neurocognition in patients with brain metastases treated with radiosurgery or radiosurgery plus whole-brain irradiation: a randomised controlled trial. Lancet Oncol 10(11):1037–1044. https://doi.org/10.1016/S1470-2045(09)70263-3
Gondi V, Paulus R, Bruner DW, Meyers CA, Gore EM, Wolfson A, Werner-Wasik M, Sun AY, Choy H, Movsas B (2013) Decline in tested and self-reported cognitive functioning after prophylactic cranial irradiation for lung cancer: pooled secondary analysis of Radiation Therapy Oncology Group randomized trials 0212 and 0214. Int J Radiat Oncol Biol Phys 86(4):656–664. https://doi.org/10.1016/j.ijrobp.2013.02.033
Mulvenna P, Nankivell M, Barton R, Faivre-Finn C, Wilson P, McColl E, Moore B, Brisbane I, Ardron D, Holt T, Morgan S, Lee C, Waite K, Bayman N, Pugh C, Sydes B, Stephens R, Parmar MK, Langley RE (2016) Dexamethasone and supportive care with or without whole brain radiotherapy in treating patients with non-small cell lung cancer with brain metastases unsuitable for resection or stereotactic radiotherapy (QUARTZ): results from a phase 3, non-inferiority, randomised trial. Lancet 388(10055):2004–2014. https://doi.org/10.1016/S0140-6736(16)30825-X
Aoyama H, Shirato H, Tago M, Nakagawa K, Toyoda T, Hatano K, Kenjyo M, Oya N, Hirota S, Shioura H, Kunieda E, Inomata T, Hayakawa K, Katoh N, Kobashi G (2006) Stereotactic radiosurgery plus whole-brain radiation therapy vs stereotactic radiosurgery alone for treatment of brain metastases: a randomized controlled trial. JAMA 295(21):2483–2491
Brown PD, Jaeckle K, Ballman KV, Farace E, Cerhan JH, Anderson SK et al (2016) Effect of radiosurgery alone vs radiosurgery with whole brain radiation therapy on cognitive function in patients with 1 to 3 brain metastases: a randomized clinical trial. JAMA 316:401–409. https://doi.org/10.1001/jama.2016.9839
Wang C, Lu X, Zhou Z, Wang J, Hui Z, Liang J, Feng Q, Chen D, Xiao Z, Lv J, Wang X, Wang X, Zhang T, Deng L, Wang W, Xiao J, Li J, Bi N, Wang L (2019) The efficacy of upfront intracranial radiation with TKI compared to TKI alone in the NSCLC patients harboring EGFR mutation and brain metastases. J Cancer 10(9):1985–1990. https://doi.org/10.7150/jca.30131
Soffietti R, Abacioglu U, Baumert B, Combs SE, Kinhult S, Kros JM, Marosi C, Metellus P, Radbruch A, Villa Freixa SS, Brada M, Carapella CM, Preusser M, Le Rhun E, Rudà R, Tonn JC, Weber DC, Weller M (2017) Diagnosis and treatment of brain metastases from solid tumors: guidelines from the European Association of Neuro-Oncology (EANO). Neuro Oncol 19(2):162–174. https://doi.org/10.1093/neuonc/now241
Hofmaier J, Bodensohn R, Garny S, Hadi I, Fleischmann DF, Eder M, Dinc Y, Reiner M, Corradini S, Parodi K, Belka C, Niyazi M (2019) Single isocenter stereotactic radiosurgery for patients with multiple brain metastases: dosimetric comparison of VMAT and a dedicated DCAT planning tool. Radiat Oncol 14(1):103. https://doi.org/10.1186/s13014-019-1315-z
Alongi F, Fiorentino A, Gregucci F, Corradini S, Giaj-Levra N, Romano L, Rigo M, Ricchetti F, Beltramello A, Lunardi G, Mazzola R, Ruggieri R (2019) First experience and clinical results using a new non-coplanar mono-isocenter technique (HyperArc™) for Linac-based VMAT radiosurgery in brain metastases. J Cancer Res Clin Oncol 145(1):193–200. https://doi.org/10.1007/s00432-018-2781-7
Ruggieri R, Naccarato S, Mazzola R, Ricchetti F, Corradini S, Fiorentino A, Alongi F (2018) Linac-based VMAT radiosurgery for multiple brain lesions: comparison between a conventional multi-isocenter approach and a new dedicated mono-isocenter technique. Radiat Oncol 13(1):38. https://doi.org/10.1186/s13014-018-0985-2
Ruggieri R, Naccarato S, Mazzola R, Ricchetti F, Corradini S, Fiorentino A, Alongi F (2019) Linac-based radiosurgery for multiple brain metastases: comparison between two mono-isocenter techniques with multiple non-coplanar arcs. Radiother Oncol 132:70–78. https://doi.org/10.1016/j.radonc.2018.11.014
Lau SK, Zakeri K, Zhao X, Carmona R, Knipprath E, Simpson DR, Nath SK, Kim GY, Sanghvi P, Hattangadi-Gluth JA, Chen CC, Murphy KT (2015) Single-isocenter frameless volumetric modulated arc radiosurgery for multiple intracranial metastases. Neurosurgery 77(2):233–240. https://doi.org/10.1227/NEU.0000000000000763(discussion 240)
Kocher M, Wittig A, Piroth MD, Treuer H, Seegenschmiedt H, Ruge M, Grosu AL, Guckenberger M (2014) Stereotactic radiosurgery for treatment of brain metastases. A report of the DEGRO Working Group on Stereotactic Radiotherapy. Strahlenther Onkol 190(6):521–532. https://doi.org/10.1007/s00066-014-0648-7
Minniti G, Scaringi C, Paolini S, Clarke E, Cicone F, Esposito V, Romano A, Osti M, Enrici RM (2016) Repeated stereotactic radiosurgery for patients with progressive brain metastases. J Neurooncol 126(1):91–97. https://doi.org/10.1007/s11060-015-1937-4
Eisenhauer EA, Therasse P, Bogaerts J et al (2009) New response evaluation criteria in solid tumours: revised RECIST guidelines (version1.1). Eur J Cancer 45:228–247
Farris M, McTyre ER, Cramer CK, Hughes R, Randolph DM 2nd, Ayala-Peacock DN, Bourland JD, Ruiz J, Watabe K, Laxton AW, Tatter SB, Zhou X, Chan MD (2017) Brain metastasis velocity: a novel prognostic metric predictive of overall survival and freedom from whole-brain radiation therapy after distant brain failure following upfront radiosurgery alone. Int J Radiat Oncol Biol Phys 98(1):131–141. https://doi.org/10.1016/j.ijrobp.2017.01.201
Mazzola R, Corradini S, Gregucci F, Figlia V, Fiorentino A, Alongi F (2019) Role of radiosurgery/stereotactic radiotherapy in oligometastatic disease: brain oligometastases. Front Oncol 9:206. https://doi.org/10.3389/fonc.2019.00206
Yamamoto M, Serizawa T, Shuto T et al (2014) Results of stereotactic radiosurgery for patients with multiple brain metastases (JLGK0901): a multi-institutional prospective study. Lancet Oncol 15:387–395
Minniti G, Anzellini D, Reverberi C, Cappellini GCA, Marchetti L, Bianciardi F, Bozzao A, Osti M, Gentile PC, Esposito V (2019) Stereotactic radiosurgery combined with nivolumab or Ipilimumab for patients with melanoma brain metastases: evaluation of brain control and toxicity. J Immunother Cancer 7(1):102. https://doi.org/10.1186/s40425-019-0588-y
Trino E, Mantovani C, Badellino S, Ricardi U, Filippi AR (2017) Radiosurgery/stereotactic radiotherapy in combination with immunotherapy and targeted agents for melanoma brain metastases. Expert Rev Anticancer Ther 17(4):347–356. https://doi.org/10.1080/14737140.2017.1296764
Johnson AG, Ruiz J, Hughes R, Page BR, Isom S, Lucas JT, McTyre ER, Houseknecht KW, Ayala-Peacock DN, Bourland DJ, Hinson WH, Laxton AW, Tatter SB, Debinski W, Watabe K, Chan MD (2015) Impact of systemic targeted agents on the clinical outcomes of patients with brain metastases. Oncotarget 6(22):18945–18955
Shen CJ, Rigamonti D, Redmond KJ, Kummerlowe MN, Lim M, Kleinberg LR (2016) The strategy of repeat stereotactic radiosurgery without whole brain radiation treatment for new brain metastases: outcomes and implications for follow-up monitoring. Pract Radiat Oncol 6(6):409–416. https://doi.org/10.1016/j.prro.2016.04.004
Moreau J, Khalil T, Dupic G, Chautard E, Lemaire JJ, Magnier F, Dedieu V, Lapeyre M, Verrelle P, Biau J (2018) Second course of stereotactic radiosurgery for locally recurrent brain metastases: safety and efficacy. PLoS ONE 13(4):e0195608. https://doi.org/10.1371/journal.pone.0195608
Sahgal A, Aoyama H, Kocher M, Neupane B, Collette S, Tago M, Shaw P, Beyene J, Chang EL (2015) Phase 3 trials of stereotactic radiosurgery with or without whole-brain radiation therapy for 1 to 4 brain metastases: individual patient data meta-analysis. Int J Radiat Oncol Biol Phys 91(4):710–717. https://doi.org/10.1016/j.ijrobp.2014.10.024
Shultz DB, Modlin LA, Jayachandran P, Von Eyben R, Gibbs IC, Choi CYH, Chang SD, Harsh GR 4th, Li G, Adler JR, Hancock SL, Soltys SG (2015) Repeat courses of stereotactic radiosurgery (SRS), deferring whole-brain irradiation, for new brain metastases after initial SRS. Int J Radiat Oncol Biol Phys 92(5):993–999. https://doi.org/10.1016/j.ijrobp.2015.04.036
Fritz C, Borsky K, Stark LS, Tanadini-Lang S, Kroeze SGC, Krayenbühl J, Guckenberger M, Andratschke N (2018) Repeated courses of radiosurgery for new brain metastases to defer whole brain radiotherapy: feasibility and outcome with validation of the new prognostic metric brain metastasis velocity. Front Oncol 8:551. https://doi.org/10.3389/fonc.2018.00551
Gasper L, Scott C, Rotman M et al (1997) Recursive partitioning analysis (RPA) of prognostic factors in three Radiation Therapy Oncology Group (RTOG) brain metastases trials. Int J Radiat Oncol Biol Phys 37:745–751
Weltman E, Salvajoli JV, Brandt RA et al (2000) Radiosurgery for brain metastases: a score index for predicting prognosis. Int J Radiat Oncol Biol Phys 46:1155–1161
Lorenzoni J, Devriendt D, Massager N et al (2004) Radiosurgery for treatment of brain metastases: estimation of patient eligibility using three stratification systems. Int J Radiat Oncol Biol Phys 60:218–224
Sperduto PW, Berkey B, Gasper LE et al (2008) A new prognostic index and comparison to three other indices for patients with brain metastases: an analysis of 1,960 patients in the RTOG database. Int J Radiat Oncol Biol Phys 70:510–514
Yamamoto M, Kawabe T, Higuchi Y, Sato Y, Nariai T, Watanabe S, Barfod BE, Kasuya H (2012) Validity of prognostic grading indices for brain metastasis patients undergoing repeat radiosurgery. World Neurosurg 82(6):1242–1249. https://doi.org/10.1016/j.wneu.2014.08.008
Yamamoto M, Sato Y, Serizawa T et al (2012) Subclassification of recursive partitioning analysis Class II patients with brain metastases treated radiosurgically. Int J Radiat Oncol Biol Phys 83:1399–1405
Yamamoto M, Aiyama H, Koiso T, Watanabe S, Kawabe T, Sato Y, Higuchi Y, Kasuya H, Barfod BE (2019) Validity of a recently proposed prognostic grading index, brain metastasis velocity, for patients with brain metastasis undergoing multiple radiosurgical procedures. Int J Radiat Oncol Biol Phys 103(3):631–637. https://doi.org/10.1016/j.ijrobp.2018.10.036
Funding
Not applicable.
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
Conflict of interest
The authors declare that they have no conflict of interest.
Additional information
Publisher's Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Rights and permissions
About this article
Cite this article
Nicosia, L., Figlia, V., Mazzola, R. et al. Repeated stereotactic radiosurgery (SRS) using a non-coplanar mono-isocenter (HyperArc™) technique versus upfront whole-brain radiotherapy (WBRT): a matched-pair analysis. Clin Exp Metastasis 37, 77–83 (2020). https://doi.org/10.1007/s10585-019-10004-3
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s10585-019-10004-3