Abstract
Cancer is a major health concern worldwide and is still in a continuous surge of seeking for effective treatments. Since the discovery of RNAi and their mechanism of action, it has shown promises in targeted therapy for various diseases including cancer. The ability of RNAi to selectively silence the carcinogenic gene makes them ideal as cancer therapeutics. Oral delivery is the ideal route of administration of drug administration because of its patients’ compliance and convenience. However, orally administered RNAi, for instance, siRNA, must cross various extracellular and intracellular biological barriers before it reaches the site of action. It is very challenging and important to keep the siRNA stable until they reach to the targeted site. Harsh pH, thick mucus layer, and nuclease enzyme prevent siRNA to diffuse through the intestinal wall and thereby induce a therapeutic effect. After entering the cell, siRNA is subjected to lysosomal degradation. Over the years, various approaches have been taken into consideration to overcome these challenges for oral RNAi delivery. Therefore, understanding the challenges and recent development is crucial to offer a novel and advanced approach for oral RNAi delivery. Herein, we have summarized the delivery strategies for oral delivery RNAi and recent advancement towards the preclinical stages.
Similar content being viewed by others
Avoid common mistakes on your manuscript.
1 Introduction
RNA interference (RNAi) is a rapidly developing filed in targeted delivery. RNAi is a mechanism where there is a selective knockdown of messenger RNA (mRNA). RNAi was first discovered in the nematode Caenorhabditis elegans by Andrew Fire and Craig Mello [1, 2]. It has been observed that exogenous double-stranded RNA (dsRNA) can cause gene suppression [1, 3]. Based on their biological roles and structures, small non-coding RNAs are classified into three main categories: miRNA (micro-RNA), siRNA (small interfering RNA), and shRNA (small hairpin RNA) [4]. siRNA is a double-stranded RNA which prevents gene expression. siRNA has been used as a targeted therapy to treat various viral diseases and cancer [5]. siRNA suppresses the expression of oncogenic genes by targeting the mRNA expression. siRNA is a small non-coding dsRNA of about 22–25 base pair with dinucleotide overhang at 3’ which interfere with the protein synthesis by blocking the translation [6,7,8]. Studies suggest that activated “Dicer,” a mammalian cytoplasmic enzyme, breaks down the long dsRNA to generate small interfering RNA (siRNA). Then, each double-stranded siRNA is fragmented into the passenger strand (sense strand) and the guide strand (antisense strand) (Fig. 1). Along the same line, the guide strand is incorporated into the RNA-induced silencing complex (RISC), while the passenger strand is degraded. The RISC contains ssRNA, a guide strand to look for and to bind with complementary mRNA molecules and Argonaute 2 (AGO2) protein, which is a member of the Argonaute family protein [9, 10]. The guide strand of siRNA then pairs with a complementary sequence in a mRNA molecule. Once mRNA is bound to siRNA, mRNA will be cleaved and destroyed by Argonaute, which causes post-transcriptional gene silencing [9, 11, 12].
siRNA-mediated gene silencing mechanism. Naked siRNA or nanoparticle-loaded siRNA enters the cell through endocytosis. After endosomal escaping, two strands of siRNA get separated into the passenger and guide strand. The guide strand along with RISC binds with the targeted mRNA and with the help of Ago2 breaks down the mRNA for selective gene silencing
As conventional chemotherapeutics cause severe toxicity due to nonspecific distribution, researchers are now looking for alternative approaches for cancer therapy and delivery [13,14,15]. Selective gene silencing therapy by siRNA has been revolutionary in cancer therapy. Compared to the conventional chemotherapeutics, siRNA has a lot of advantages in cancer treatment [16]. Several studies suggest that siRNA can significantly reduce the cancer cell by silencing responsible gene [16]. In addition, siRNA was found to be sensitive in drug-resistant tumors like chemotherapy-resistant prostate cancer, breast cancer, and lung cancer [17,18,19,20]. Ongoing research is focused on identifying the genes that can be silenced to reduce cancer cell population or increase the sensitivity of chemotherapy. This selective targeting is very beneficial for the clinical management of patients by treating cancer-specific cells that do not harm the neighboring health cells [21]. With significant progress, several siRNA-based cancer therapeutics have moved to the clinical trial for solid tumor, mesenchymal cancer, and pancreatic cancer (Table1) (NCT01591356, NCT03608631, NCT03087591, NCT00672542, NCT01437007). However, the siRNA considered for the pre-clinical and clinical are mostly delivered as injectables without carriers or with liposomal nanoparticle-based carriers. Usually, biological molecule-based therapeutics including siRNA offer higher therapeutic potential than small molecules because of their biocompatibility, feasibility, and less toxicity [22,23,24]. However, the larger molecular weight prevents their diffusion via biological barriers due to the interaction with biological barriers [24]. The siRNA-based targeted therapy started in the early 2000s. RNAi is required to be administered via injection though oral delivery is always preferable for the patient and the manufacturing perspective due to being painless, patient compliance, and non-sterilize production [25].
Oral delivery of therapeutic RNAs is still a challenge because of the poor cellular uptake, instability under physiological conditions (harsh pH of stomach), degradation under nucleases, off-target effects, clearance by phagocytes such as macrophages, and possible immunogenicity [5, 26, 27]. To achieve the expected therapeutic effect of RNAi (siRNA), an appropriate vehicle is required that can transport the RNA to the site of action in the cells of target tissues [26]. The successful application of siRNA for cancer therapy requires the development of clinically suitable, safe, and effective drug delivery systems [28]. In this review, we will discuss the progress in the oral delivery of RNAi, different carrier systems, challenges of oral delivery, and different ways to overcome current challenges.
2 Evolution of oral RNAi-mediated cancer research
The discovery of siRNA was not too long ago. At the earliest onset of the twenty-first century, it was discovered by Andrew Fire and Craig Mello in 1998 [29]. Afterwards, as researchers kept pursuing the role of siRNA, Hamilton and Baulcombe discovered how it can contribute in post-transcriptional gene silencing (PTGS) in 1999 [30]. Eventually, it leads to being reported that a target gene can be silenced by introducing siRNA into mammalian cells in 2001 [31]. Subsequently, various research was conducted to utilize the properties of RNAi in the fields of biomedical research and drug development. Statistical data shows that, between 2001 and 2005, there has been around 6122 (Fig. 2) publications made focusing on siRNA. Due to the importance of their pioneering discovery, Fire and Mello were awarded the Nobel prize in Medicine in 2006 [32]. The following 4 years saw a rise of siRNA-related research by about 4.6 times more where 28,443 papers were published. Following this trend, the next decade saw 4 times more publications than its predecessor. Nearly 81,985 research articles were published in a span of 10 years as multibillion dollar pharmaceutical industries started investing in RNAi startups.
After nearly two decades of continuous research, siRNA-based therapeutics like ONPATTRO® (Patisiran) and GIVLAARI™ (Givosiran) were introduced by Alnylam Pharmaceuticals to treat hereditary transthyretin (hATTR) amyloidosis as well as acute hepatic porphyria (AHP) respectively [33,34,35]. These US-FDA (US Food and Drug Administration) and EC (European Commission) approved drugs have implications on how siRNA technology can be used to treat mutagenic disorders in the human body. Properly strategizing delivery methods of siRNA can help enable fight off cancer. The development of inorganic nanoparticles serving as drug carriers has made this procedure much easier. This new direction for cancer treatment has already been successful in reducing lung cancer, ovarian cancer, breast cancer, liver cancer, prostate cancer, etc. as referenced in Table 1. Already since 2020, more than 8280 articles have been published further increasing the scope of siRNA research, and the number keeps increasing. And it is only a matter of time till the numerous other RNAi-based drugs and therapeutic approaches from the waiting list get approved by US-FDA. Figure 3 represents a timeline for the evolution of oral RNAi since its discovery.
In this review, we are focusing on the oral delivery of RNAi. The above information gave us an idea about the RNAi that could be used for cancer treatment. Now, we will discuss how RNAi could be delivered orally. Oral delivery is the most sought out means of administration for treatments mainly because it can be self-administered, is easy to transport, and has usability. However, a form of cure for cancer orally was not prevalent until much later. The journey of release drug delivery system was pioneered with Spansule® back in 1952 [36], which utilized the control of dissolution of the drug using a coating barrier that restricts interaction with gastrointestinal fluids. From there onwards, various other drugs were in development utilizing various forms of release mechanisms like diffusion, osmosis, and ion exchange. But up until the 1980s, all the drugs that were formulated would work up to 24 h. Only after 1989 was Lupron Depot® brought to the market as a poly lactide-co-glycolide (PLGA)-based injectable that retains its therapeutic effects for up to 6 months subsequently began the new era of PEGylation which brought in drugs like Doxil®, Movantik®, Onpattro®, and many others, where the idea is to attach the PEG (polyethylene glycol) to protein molecules so that they can be prevalent in the bloodstream for a much longer period [37, 38]. However, the downside to this form of therapeutic treatments is these cause a reduction in efficacy on successive uses.
Soon afterwards, the inclusion of nucleic acid-based therapeutics entered the procedure because of its increased possibilities and the ability to treat and repair numerous genetic disorders and reduced complicacies with drug discovery. Even though the world saw opportunities with non-oral-based measures, there has not been much success with oral-based nucleic acid drug delivery. The challenges mainly reside in the biological barriers of the GI tract, resulting in a compromised therapeutic outcome. Taming nanoparticle-based coatings is the key to overcoming these hurdles. Since the 1990s, polymeric nanomaterials like PEI-based nanoparticles have garnered much attention as it is known to interact with negatively charged nucleic acids, improving cellular internalization [39]. Jones et al. (1997) first delivered the oral plasmid DNA with PLGA nanoparticle [40]. The first successful oral siRNA was delivered by a group of researchers in 2009 for the suppression of systemic inflammation. They entrapped the TNF-α siRNA within beta-1,3-D-glucan particle [41]. Then began the development of PEI/siRNA complexes to silence tumor necrosis factor a (TNFa) via oral administration to treat inflammatory bowel disease or IBD [42]. Ballarín-González et al. (2013) first proved that siRNA loaded in chitosan nanoparticle can distribute in different organs even 1 h after gavage whereas naked siRNA cannot [43]. In search for nontoxicity and effective absorption in the GI tract, researchers stumbled upon Chitosan-based NPs, like oligonucleotide (ODN)-loaded chitosan-modified poly (D,L-lactide-co-glycolide) nanospheres (CS-PLGA NSs) for the treatment of ulcerative colitis (UC) [44]. Other notable researches on chitosan-based components included the oral delivery of Map4k4 siRNA to treat dextran sulfate sodium (DSS)-induced UC by galactosylated trimethyl chitosan- cysteine (GTC/TPP) NPs [45].
Lipid-based nanoparticles also entered into the research table due to its easy binding structure. This served as the baseline for developing Lipofectamine™, which is mostly used for gene transfection in laboratories [46], besides also proving to be highly stable in gastrointestinal environments making it suitable for oral delivery [47]. To date, this has been the most used method of RNA-based drug delivery coupled with other materials for oral administration.
3 Barriers in oral delivery
Successful delivery of siRNA is challenged by their own physicochemical properties and various biological barriers in the gastrointestinal (GI) tract [48, 49]. The focus is to protect the siRNA and maintain their stability from the route of administration to the site of action and to transport through the intracellular layer by avoiding the enzymatic degradation. siRNA is hydrophilic and negatively charged which minimizes the membrane permeability [50]. The charge and large size also affect the diffusion through intestinal layer. To overcome this obstacle, the conjugation of siRNA with bioactive and biocompatible molecule and the synthesis of hydrophobic siRNA had been successfully reported [51].
3.1 Physiological properties of different parts of the GI tract
The gastrointestinal (GI) tract comprises of mouth, esophagus, stomach, small intestine, and large intestine. Each of these segments has its own properties and poses as a barrier in a different way. Oral cavity has been a popular site of the local delivery of drugs. The esophagus does not consider as ideal drug delivery place due to first transition time. The stomach on the other hand is a place of drug degradation. Low pH, thick mucus layer (50–140 µm), and gastric enzyme make the stomach unfavorable for oral delivery [52]. The retention time however depends on the gastric emptying. For delivering any drug in the stomach, it needs to be stable in low pH to prevent enzymatic degradation and pass through the thickest mucus layer of the GI tract [53]. The mucous layer is very viscous, and it has a net negative charge due to the presence of sulfate and sialic acid which prevents the diffusion across the layer.
The small intestine is considered the most favorable site for drug absorption due to its long retention time, extensive surface area, high epithelial permeability, and systemic absorption. Especially in Peyer’s patches (a lymphoid system in the small intestine), there is less mucous layer which favors the absorption of hydrophobic molecule [54, 55]. However, the intestinal enzyme and mucus layer hinder the absorption. Large intestine residence time is up to 20 h; however, the fecal matter and bacteria create problem in successful drug delivery.
3.2 Mucus layer as a barrier for RNAi-based oral therapeutics
The mucus layer is a protective layer for the underlying mucus membrane of the eye, respiratory tract, stomach, and genital tract. The mucus layer protects the mucosa from hydrochloric acid of the stomach, pathogens, or other foreign particles and also presents as a barrier for the diffusion of drug or drug carrier. It also acts as a lubricant and maintains the moisture of the GI tract. Mucus is mainly composed of water (90–95%) and mucin (2–5%) [54]. Mucin is a high molecular weight glycoproteins responsible for forming an entangled network and gives the gel-like properties to the mucus [56]. There are two layers of mucus over the epithelium, adjacent adherent mucus and upper loose mucus layer [57]. Mucus is secreted continuously from the goblet cell and mucous cell in the intestine and the stomach, respectively [58]. The continuous degradation and shedding of mucus along with peristalsis movement of the GI tract depict a dynamic barrier for the drug. To overcome this barrier, the drug has to be diffused upstream to reach and cross the epithelium. In addition, the shear-thinning properties of mucous enable the upper layer of mucus to coat and lubricate the intestinal content and form a slippage plane [54, 59]. The mucin network forms a mesh-like filter for the larger molecules (mesh size 100 to 2000 nm, depending on the body part). For the particle larger than the mesh size, it presents as a barrier and hinders their passage through the mucus (Fig. 4). The unstirred water layer and viscosity also contribute to the steric properties of the mucus barrier. Though the steric barrier does not affect the particle smaller than the mesh size, it can get constrained by the interactive filter where the particles bind with the different components of mucus and get trapped [60]. The polyanionic mucin acts as an interactive filter for the negatively charged DNA and bacterial polysaccharide [61, 62]. Furthermore, the hydrogen bonds from the carbohydrates produce ionic interaction and polyvalent bond with the particle and prevent diffusion [56, 59, 63].
Illustration of mucus layer as a barrier for drug delivery. Positively charged, hydrophilic small molecule can diffuse through mucus layer to get absorbed through the epithelium. Large molecule cannot pass the mucus barrier due to steric barrier. Furthermore, a molecule of any size can interact with different components of mucus and get trapped there. Both naked siRNA and siRNA loaded in carrier must pass the mucus barrier to enter the epithelium. The image was adapted from “Drug Diffusion Through Mucus Barriers” BioRender.com (2022). Retrieved from https://app.biorender.com/biorender-templates
3.3 Enzymatic degradation as a barrier for RNAi-based oral therapeutics
Biological compounds undergo enzymatic degradation in the GI tract by proteases. Nucleic acid compounds like siRNA get degraded by nuclease (Fig. 5). Nuclease is an essential enzyme for DNA repair, DNA replication, base excision repair, and mismatch repair mechanism. Nuclease enzyme is also capable of breaking the phosphodiester bond of nucleic acid. Nuclease and nucleosidases are the nucleic acid-degrading enzyme, secreted from the pancreas. It was found in a study that plasmid DNA is completely degraded in a diluted GI fluid [64]. To avoid the breakdown, the physicochemical characteristic of siRNA needs to be changed, or it needs to be delivered with a carrier that can prevent the degradation by nuclease enzyme [65]. For instance, siRNA has been modified with 2′-flouro (2′-F) pyrimidines to increase the plasma half-life of siRNA in mice plasma [66]. Another study reported that 2′-O-MOE-modified oligonucleotides were stable in rat duodenum for at least 8 h; however, the plasma concentration was only 0.3 to 5.5% compared to intravenous administration [67].
3.4 Barriers for cellular internalization
Another challenge for siRNA molecule faces is the uptake by intestinal epithelium and reaching the circulation. The brush border of the intestine presents a large amount of polar carbohydrates and charged amino acid side chains which provides a high negative charge to the microvilli at the enterocytes [68]. As siRNA is also negatively charged, the enterocyte repulses the siRNA molecule which makes it harder to attach with the cell. Even if siRNA overcomes the repulsion, the hydrophilic nature of it permeates the lipophilic phospholipid bilayer of enterocytes. After crossing all those barriers, nucleic acid reaches the intestinal epithelium. There are four general pathways that are being utilized to facilitate the absorption [69]: (i) transcellular pathway (through epithelial cells), (ii) paracellular pathway (between adjacent cells), (iii) transcytosis and endocytosis, and (iv) lymphatic absorption through M-cells of Peyer’s patches. siRNA-based therapeutics < 5 kDa can be transferred through paracellular pathway, where if the mass is more than that then endocytosis is the only option. In the endocytosis process, cells engulf the molecule and form endosome, and the molecule is delivered via endosome to the lysosome for degradation with lysosomal enzyme (Fig. 6). Thereafter, it goes to the Golgi apparatus for processing, or some of it goes back to the plasma membrane [70,71,72]. One of the major advantages of using siRNA as a therapeutic is that they work within the cytoplasm; therefore, it is not required for them to cross the nuclear barriers. In addition, if it successfully passes all the barriers, it goes under first-pass metabolism.
The mechanism on how siRNA enters the cell by endocytosis and forms endosome. The endosomal content gets degraded by the lysosomal enzyme, and it then goes to the Golgi network for processing. The image was adapted from “Cellular Environment (Background)” BioRender.com (2022). Retrieved from https://app.biorender.com/biorender-templates
4 Carriers for oral delivery of siRNA
Naked siRNAs are comparatively less stable in the bloodstream (degradation by endogenous enzymes) compared to the packaged one. The possible reasons are immunogenic in nature and not permissible to cells through membranes due to the larger size (∼13 kDa) as well as the high negative charge [73]. A suitable carrier enables the delivery of siRNA to the target cells to achieve the optimal silencing effect of the specific gene of interest. Due to their high transduction efficiency, viral vectors such as adenoviruses, herpes simplex-1 viruses, retroviruses, and lentiviruses are widely used as RNA carriers. However, viral vectors have the challenges like immunogenicity—the possibility of an immune response, which could neutralize the viral vector and thus limit the delivery, off targeting due to broad viral tropism, toxicity, mutagenesis, patient’s compliance, bulk production constrains, and high cost. Whereas, non-viral biomaterial-based gene delivery vectors offer the advantages such as specific targeting possibility, ease of production, safer profile, greater loading capacity, low cost, higher production yield, and repeated administration capability [74, 75]. Two decades after the discovery of RNAi, some of the siRNA therapeutics, for instance, Onpattro (patisiran), have gotten FDA approval and are now used in clinics [76, 77]. In this review, we will discuss the emerging application of non-viral vector in RNAi delivery, in vitro and in vivo.
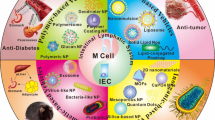
Major non-viral siRNA vectors such as inorganic nanomaterials, polymeric nanomaterials, dendrimers, micelles, liposomes, hydrogels cationic lipids, and peptides are displayed in Fig. 7. To activate the RNAi pathway and knocking down the gene, the siRNA must cross all the barrier and go into the specific site of action. To achieve that expected therapeutic outcomes, the siRNA needs to be delivered either by chemical modification or with any carrier. Systemic delivery of siRNA, especially with cholesterol conjugates, liposomes, and polymer-based nanoparticle approaches, has also been widely explored with moderate success.
4.1 Nanoparticle as a RNAi carrier
The siRNA-based targeted therapy started in the early 2000s and introduced solution to the concerns such as low intracellular uptake, limited stability, and non-targeted immune stimulation. Ligand-targeted nanoparticle delivery systems combining multiple functions improved the drug delivery scenario [78]. Nanocarriers facilitate longer blood retention time, stability, cell penetration property, target-specific delivery, pH-sensitive release, and prevent intracellular endosomal uptake. Organic nanocarriers are biocompatible, biodegradable, stable, and non-immunogenic in nature. They include liposomes, micelles, dendrimers, polymeric nanoparticles, and carbon nanomaterials (graphene, carbon nanotubes, and fullerene). Polymeric nanocarriers include both natural polymers and synthetic polymers [79].
4.1.1 Liposomes as a RNAi carrier
Consideration of lipid as carrier for RNAi has received huge attention recently due to the FDA approval of mRNA-based COVID-19 vaccine along with many other promising outcomes as reported recently. Lipid nanoparticles are used in RNAi delivery due to the protective effect from degradation, biocompatibility, enhanced cellular uptake, and controlled release capability. To address the non-specific delivery, targeting ligands like folate, transferrin, peptides, oligosaccharides, monoclonal antibodies, and aptamers could be incorporated into the lipid nanoparticles [80]. Liposomes are excellent drug carriers (40–500 nm in size) which are made of natural or synthetic lipids and surfactants. The presence of a lipid membrane and aqueous core enables them to carry both lipophilic and hydrophilic agents, and its morphology mimics the cell membrane in nature. Liposomes offer excellent gene transfer possibilities with genetic materials such as DNA, ribozymes, DNAzymes, aptamers, (antisense) oligonucleotides, and siRNAs [81]. Depending on the availability of various phospholipids and intercalating molecules also surface modification with PEG, numerous liposomes could be designed with desired composition, size, surface charge, and morphology to improve the delivery process and imaging purposes. Phagocytic uptake and cellular membrane adhesion and fusion are the predominant uptake mechanisms of liposomes [82, 83]. With dramatic progress in the recent year, numerous liposomal siRNA delivery systems like ALN-VSP02 (targeting KSP and VEGF genes), siRNA-EphA2-DOPC (targeting EphA2 gene), Atu027 (targeting PKN3 gene), ALN–PCS02 (targeting PCSK9) are in clinical trials [84].
Liposome structures for siRNA are mainly of four types—lipoplexes, stable nucleic-acid–lipid particles (SNALPs), lipopolyplexes, and membrane/core nanoparticles (MCNPs). Lipolexes are multilamellar structures made of cationic liposomes, where siRNA is embedded between lipid bilayers. Commercial liposomes like Lipofectin, Lipofectamine, and LipoRNAiMAX form efficient lipoplexes. SNALPs are neutral in surface charge, and the lipids used are sensitive to acidic pH.
Lipopolyplexes are liposomes containing polyplexes (cationic polymer/siRNA complexes). The core–shell structure of MCNP has a solid core made of one or more inorganic porous nanoparticles (calcium phosphate or silica) and lipid bilayer as the shell. For the siRNA transfer, cationic liposomes are used widely; DOTMA and DOTAP poly-l-lysine, PEI, and poly(2-(dimethylamino)ethyl methacrylate) are the most used lipids in siRNA delivery. However, anionic lipids and neutral lipids are also tested in siRNA delivery where neutral liposomes showed excellent tumor accumulation and endosomal escape with improvable siRNA delivery. Which clearly indicate the role of surface charge of the carrier systems in siRNA delivery [84, 85].
Another tumor-targeted siRNA delivery by a nanoscale quaternary polyplex (NQP) is developed with a core–shell structure, which has an ATP-responsive core with a pH-responsive shell. The introduction of siSTAT3-loaded NQP to tumor-bearing mice and the ex vivo fluorescence imaging analysis confirmed the tumor accumulation of the nanosystem. Also, further analysis methods have been established the effective gene silencing and tumor growth inhibition [86]. PEG modification can improve the systemic stability of siRNA lipoplexes. In an in vitro gene silencing investigation on lung cells, regardless of the PEG-derivative type, the PEGylations of cationic liposome/siRNA complexes displayed enhanced systemic stability without losing transfection activity [87]. In another investigation, six nanoliposomes made of different cationic lipids were tested in vitro and in vivo for cellular delivery functions in lung cells/tissues using myeloid cell leukemia sequence 1-specific siRNA (siMcl1). Cationic lipids were used including 1,2-dioleoyl-3-trimethylammonium-propane (DOTAP), 1,2-di-O-octadecenyl-3-trimethylammonium propane (DOTMA), and 1,2-dioleoyl-sn-glycero-3-ethylphosphocholine (EDOPC). The different nanoliposomes showed comparable siRNA delivery efficiency in vitro; however, in vivo pulmonary cellular delivery functions of the fluorescent nanoliposomes exhibited differences. The ECL nanoliposomes made of cationic dioleoyl-sn-glycero-3-ethylphosphocholine and cholesterol exhibited the lowest cytotoxicity in vitro and the highest pulmonary cellular delivery in vivo. Compared to the naked siRNA, the siRNA in ECL nanoliposomes showed a 26-fold increased delivery efficiency and remarkable silencing effect on overexpressed lung tissue proteins [88, 89].
In 2013, the lipid nanoparticle was first used for siRNA-mediated non-cytotoxic gene silencing in intestinal epithelium. They proved that lipid nanoparticles increase the cellular uptake and prevent the pH degradation of siRNA [90]. Later, the same group of researchers delivered the siRNA loaded in lipid nanoparticle in mice. It showed that lipid nanoparticle can retain in the mice intestine for at least 8 h after delivery [91]. Lipidic aminoglycoside derivatives are utilized in the oral delivery of extra cellular miRNA in mice models for introducing epigenetic manipulations under stress [92]. Likewise, lipidic aminoglycoside derivatives were also used for the oral delivery of breast milk miRNA for young rat models [93]. In the case of dietary miRNA, the absorption process is dependent on systemic RNA interference defective protein 1 (SID-1), which helps the transport of exogenous RNA to the cytoplasm [94].
4.1.2 Micelles as a RNAi carrier
Micelles are self-assembled, core–shell structured colloidal nanoparticles with a size range of 5–100 nm, made of block copolymers with hydrophilic and hydrophobic groups [95]. Micelles are intelligent gene delivery systems and support siRNA delivery in anticancer therapies. For the targeted delivery of siRNA to BxPC3 pancreatic cancer cells, an antibody fragment (Fab′)-installed polyion complex (PIC) micelles was designed using block copolymer of azide-functionalized poly(ethylene glycol) and poly(l-lysine). The flow cytometric analysis displayed binding affinity of the micelles to the cells, penetrability, cellular internalization process, and gene silencing effect [96]. Similarly, The in vitro flow cytometry analysis of FITC labeled siRNA–PLGA hybrid and Fab′–PLGA hybrid micelles, displayed high permeability, and targeted accumulation in CEMx174 lymphocyte cells [97]. Another siRNA carrier for colon cancer treatment was prepared by modifying mPEG-PCL micelle with cationic DOTAP lipid, which showed inhibition of the growth of C26 colon cancer cells in vitro and in vivo tumor models [98]. Bile acid derived cholic acid -based block copolymers created mixed micelles with high siRNA loading, which showed improved cell uptake with excellent siRNA transfection in HeLa and HeLa-GFP model cells [99]. A cholesterol-modified chitosan based micelle was utilized for the delivery of curcumin and siRNA towards A549 human lung cancer cells, which showed excellent cellular uptake by the clathrin-mediated endocytosis [100]. Another synergistic delivery system was developed by Shi et al., where a pH sensitive triblock copolymer micelle was created for the co-delivery of siRNA and paclitaxel to tumor cells [101].
Micelles are excellent carriers for oral delivery. Micelles have been widely used for oral drug delivery like different small molecules, insulin, and siRNA [102, 103]. Han et al. reported that zwitterionic micelle mimics a virus like structure and enables it to cross the mucus layer and epithelial tight junction of the GI tract. They reported > 40% oral bioavailability of insulin with zwitterionic micelle [104]. A group of researchers in Japan delivered anti-RelA siRNA orally with a multifunctional peptide carrier (CH2R4H2C)-modified methoxy polyethylene glycol-polycaprolactone polymer micelles (MPEG-PCL-CH2R4H2C). They found for the treatment of IBD. They found improved delivery of MPEG-PCL-CH2R4H2C/siRNA to mice colon compared to naked siRNA. siRNA loaded with micelle had better cell internalization, did not degrade the harsh pH, and was not toxic to the healthy cell [105]. Micelles have a great potential to be used as carriers for oral delivery in other GI cancer or any other cancers.
4.1.3 Dendrimers as a RNAi carrier
Dendrimers are self-assembling nano-sized molecules with a symmetric core, an inner shell, and an outer shell. The exhibit features like low cytotoxicity, polyvalency, electrostatic interactions, ease of surface modification, chemical stability, and water solubility which makes them excellent carriers for siRNA delivery [106, 107]. Ruthenium-based carbosilane-based metallodendrimers are investigated as anticancer siRNA carriers in HL-60 cells [108].
Poly(amidoamine) (PAMAM) dendrimers are extensively used in anticancer applications with its surface and internal modifications enabling the increase in cell specificity and transfection efficiency with the least cytotoxicity towards healthy cells [109]. PAMAM dendrimers with a high density of cationic charges display electrostatic interactions with nucleic acids (DNA, siRNA, miRNA, etc.), creating dendriplexes that can preserve the nucleic acids from degradation. These dendrimers are also efficient for the co-delivery of drugs and genes [110]. Co-delivery of siRNA and curcumin was investigated by polyamidoamine (PAMAM) dendrimers—PAMAM-Cur/Bcl-2 siRNA with ∼82 wt% of curcumin loading. When compared with curcumin or siRNA alone, the dendrimers displayed a more efficient cellular uptake and tumor cell proliferation inhibition towards HeLa cell lines which showed the synergistic effect of these dendrimers [111]. Nuclear factor erythroid 2-related factor 2 (Nrf2) is the transcription factor regulating antioxidant and cytoprotective gene expressions and plays a critical role in cancer progression. Cisplatin is an anticancer drug widely used in different cancers. Nrf2 has the ability to surpass the chemo resistance of bladder cancer cells and thus make them accessible to the treatment, so siRNA targeting the Nrf2 gene is loaded to the nano-micelles and tested in human kidney HK-2 cell to evaluate the drug response in the cancer cells [112].
Another multifunctional anticancer siRNA delivery system was developed by using superparamagnetic iron oxide nanoparticles and Poly(Propyleneimine) generation 5 dendrimers with cisplatin. PEG coating and LHRH peptide enabled the serum stability and specific targeting to cancer cells, respectively [113]. Similarly, for the delivery of Hsp27 siRNA to PC-3 prostate cancer cells, PAMAM dendrimers with a triethanolamine core are developed. The Hsp27 siRNA focus on the specific gene silencing of heat-shock protein 27, for castrate-resistant prostate cancer therapy. The Hsp27 gene silencing leads to the induction of caspase-3/7-dependent apoptosis and PC-3 cell (in vitro) growth inhibition [114].
Another PMAM 4th generation dendrimer for breast cancer therapy was developed with methotrexate (MTX) for the targeted delivery of siRNA to suppress high mobility group protein A2 (HMGA2)—a transcription factor related to progression. HMGA2 siRNA was electrostatically adsorbed on the dendrimers and effectiveness on folate receptor-expressed breast cancer cell lines such as MCF-7, and MDA-MB-231 was assessed. The delivery of siRNA and MTX from the dendrimers by smart release (pH and time-dependent manner) demonstrated cell internalization and gene silencing effects [115]. Dendrimers have been extensively researched for successful gene delivery however oral gene delivery with dendrimers is yet to be explored. PAMAM dendrimers are an ideal component for oral drug delivery as well, due to their ability to translocate through GI epithelium [116]. Dendrimers are one of the best delivery cargo for oral nucleic acid delivery [117]. This area of RNAi delivery needs more research.
4.1.4 Other nanomaterials as RNAi carrier
The other major nanomaterials used in siRNA transfer are polymeric nanomaterials, metal/metal oxide nanoparticles, and carbon nanomaterials.
Polymer nanomaterials-based siRNA delivery systems along with chemical drugs are used in various anticancer therapies successfully. The promising features of mTOR siRNA against lung cancer are limited by its poor stability in biological conditions. Synthesis of a modified-poly (amino-ether) (mPAE) polymer encapsulation of the mTOR siRNA created stable and bio-reducible nanoparticles which is capable of gene knock down and inducing apoptosis in A549 and H460 lung cancer cells [118]. Based on electrostatic interactions, various cationic polymers are used in the efficient delivery of siRNA. For example, nylon 3 copolymers were used for the successful delivery of siRNA to glioblastoma cells. These carriers exhibited high transfection efficiencies, excellent cell internalization, protein knockdown capacities, less cytotoxicity, and significant cellular tolerability [119]. To improve the colloidal stability of the cationic polymer-based nanodelivery system, photocrosslinked bioreducible nanoparticles (XbNPs) are incorporated with them. These carriers have ester bonds, which dissociate by hydrolytic degradation for the intracellular environmentally triggered delivery of RNA for systemic delivery approaches. When tested in both glioma and melanoma cells in high-serum conditions, these XbNPs exhibited enhanced gene knockdown compared to the non-crosslinked delivery systems. The analysis on a metastatic melanoma model with colonized lung tumors displayed the selective accumulation of the nanosystem and safe in vivo delivery of the siRNA [120].
Similarly, to treat gastric cancer stem cells (CSCs), a dual targeting system was developed using CSC-targeting glioma-associated oncogene homolog 1 (Gli1) siRNA nanoparticles and an intrinsic ligand of the CD44 receptor. From the in vitro and in vivo evaluations, the targeting Gli1 siRNA nanoparticles were specifically targeted towards the tumor tissue and selectively eliminated gastric CSCs, and subsequently displayed higher therapeutic efficacy [121].
For glioblastoma (GBM) treatments, multiple siRNA nanopolymeric systems have been found effective. Nanoparticle formulations with different siRNA targeting anti-glioblastoma genes such as Robol, YAP1, NKCC1, EGFR, and survivin were tested with the results in terms of GBM cell death, reduction in GBM migration and suppressing tumor progression [122].
A different siRNA delivery system for inhibiting vascular endothelial growth factor receptor-2 (VEGF R2) expression was designed with self-assembling nanoparticles. This polyethyleneimine (PEI) and PEGylated-based nanosystem had an Arg-Gly-Asp (RGD) peptide ligand for targeting the tumor overexpressed integrins enabling targeted delivery of siRNA. In vivo mouse model studies exhibited tumor-specific uptake, inhibition towards tumor angiogenesis, and tumor growth [21]. In 2022, oral Ephb4 shRNA was delivered with inulin-coated Mn3O4 nanocuboids in Apc knockout colon cancer mice model. The study concluded that inulin-coated Mn3O4 protects the siRNA from degradation in intestinal milieu, does not change the property, and produces a therapeutic effect. It also showed pH-responsive and dual MRI contrast imaging properties [123].
4.1.5 Metal and carbon nanoparticles-based carriers
Metal, metal oxide, and carbon nanomaterials are extensively used for siRNA delivery towards cancer treatment. Gold nanoparticles are one of the mainly used as a carrier system in various siRNA delivery investigations. The biocompatibility, photo thermal potential, and bioimaging capacity makes them excellent diagnostic and delivery system [124,125,126]. Although gold nanoparticle has yet no been used in oral RNAi delivery, it has been used in oral delivery of recombinant insulin [127, 128]. Similarly, carbon nanomaterials such as graphene, graphene oxide, activated carbon nanoparticles, carbon dots, and carbon nanotubes also play a key role in siRNA delivery [129,130,131,132]. Furthermore, metal oxide nanomaterials such as manganese oxide, iron oxide, silica, and metal–organic frameworks such as also productively used for gene therapy using siRNA. Despite the siRNA carrier capacity, metal oxide nanomaterials have phototherapy and imaging potential due to their magnetic properties which enable them to be good bioimaging tools for magnetic resonance imaging and combination therapy for theranostics applications [133,134,135,136]. Researchers have used polyethyleneimine (PEI)-modified magnetic Fe3O4 nanoparticles to deliver the oral Bcl-2 siRNA for oral cancer treatment [137].
4.2 Nanogel based carriers
Nanogels are nano-sized hydrogel-like polymeric materials with characteristic properties of both nanoparticles and hydrogels. The small size facilitates the interaction of nanogels with cells in a specific manner which supports the internalization, and the crosslinked polymer networks enable the functionalization or integration of various therapeutics. By altering the chemical composition, the features of nanogels such as size, charge, porosity, amphiphilicity, and smoothness can be changed. Nanogels can be also modified as stimuli-responsive materials which could trigger the release of therapeutics depending on the change in temp or pH [138].
Considering the cytocompatibility, stability, and transfection efficiency, stimuli-responsive nanogels are excellent candidates for siRNA transfer [139]. Another nanogel was made of self-assembled cholesterol-bearing cycloamylose with spermine group for the delivery of vascular endothelial growth factor (VEGF)-specific short interfering RNA (siVEGF) for treating renal cell carcinoma (RCC). This nanogel was up-taken by the endocytotic pathway, resulting in efficient knockdown of VEGF leading to reduction of neovascularization and interleukin production also inhibited tumor progression [140]. Polyaspartic acid-derived amphiphilic cationic polymers derived nanogel has shown impressive result to deliver oral gene delivery in gut disease [141]. TNF-α targeting siRNA was delivered orally through polycationic 2-(diethylamino)ethyl methacrylate-co-tert-butyl methacrylate (DEAEMA-co-tBMA) nanogels (∼100 nm diameter) for the treatment of inflammatory bowel disease [142], which creates the opportunity to use other different RNAi orally for GI cancers.
4.3 Nanofiber as a RNAi carrier
Nanofibers are polymer fibers with a diameter of less than 1000 nm, created mostly by electrospinning, a technique applying a strong electric field. The polymer solution is prepared and filled in a syringe and allowed to pass through the needle at a specific flow rate. Depending on the electrostatic force created, the polymer forms a jet and fixes on the electrically charged surface created by nanosized fibers. The nanofiber size depends on the polymer composition, solvent, viscosity of the polymer, needle size, electric charge, evaporation rate, etc. The properties of nanofibers depend on the polymer, solvent, and additives; the properties of nanofibers also vary [143]. Nanofibers are made of natural polymers, synthetic polymers, carbon-based materials, semiconducting materials, and composite materials. Nanofibers are used in as medical applications (e.g., drug delivery, wound dressing, tissue engineering, regenerative medicine), energy applications (battery, fuel cell, super capacitors, solar cells, hydrogen storage), environmental remediation, and water treatment [144]. Nanofibers made of natural polymers have excellent biocompatibility and less immunogenicity, and nanofibers made of synthetic polymers have good flexibility and great functionalization possibility, which makes them perfect candidates for medical applications. High surface area, good drug loading efficiency, porous nature, controlled drug release capability, and the possibility to tailor the matrix properties are the major advantages of nanofibers in drug delivery [145].
In cancer research, nanofibers are conjugated with anticancer therapeutics for controlled release. Additionally, nanofibers are also used in combinatorial therapy, cancer diagnosis, construction of in vitro 3D cancer model, and engineering of the bone microenvironment in cancer metastasis [146]. Nanofibers incorporated with proteins and nucleic acids for therapeutic or diagnostic purposes include hormones, growth factors, enzymes, antibodies, and nucleic acids (plasmid DNA, DNA fragments, RNA) [147].siRNA-based gene silencing is successfully implemented using made of collagen, chitosan, and mesoporous silica nanofibers [148,149,150]. A tumor-targeted therapy integrated system for the delivery of siRNA using nanofibers is developed by Yang et al. for cancer treatment. The combination of siRNA with a peptide-conjugated-AIEgen (FC-PyTPA) created FCsiRNA-PyTPA. When introduced to the tumor region, in presence of MMP-2, the system cleaved to 2 units as FCsiRNA and PyTPA and internalized in cells by macropinocytosis and caveolae-mediated endocytosis respectively. The in vitro in vivo analysis proved that self-assembled nanofibers enable lysosomal disruption and protect siRNA for further gene silencing. This multimodal cancer therapy enhances the therapeutic efficiency of the individual unit by gene interference of the siRNA and ROS production to the tumor cells by PyTPA [151]. A localized anticancer system was developed using chromium-doped zinc gallate nanofibers surface modified with gold nanorods in combination with hTERT siRNA. Gold nanorods enabled the photo thermal effect and thus the release of siRNA to the cytoplasm and thus the improved transfection efficiency for which enhances the gene silencing effect up to 65%. In vitro anticancer assays on HEpG2 showed excellent biocompatibility, whereas western blots and qPCR analysis displayed good gene silencing efficiency [152].
Electrospinning nanofibers have great potential for oral small and large molecule delivery. Researchers stated that double-layered electrospun nanofiber composed of Eudragit and chitosan has the properties of sustained release of recombinant human growth hormone delivered to heal oral mucositis [153]. Researchers have used self-adjuvanting peptide nanofiber–CaCO3 composite microparticles for oral vaccine delivery [154].
4.4 Polysaccharide as a RNAi carrier
Biocompatibility, biodegradability, and low immune response are the attracting features of natural polysaccharides as a delivery system. Chitosan, hyaluronic acid, and cyclodextrin are some of the excellent examples of natural polysaccharides used as siRNA delivery systems. The nano state of polysaccharides displayed enhanced tissue absorption, low immunogenic responses, extended siRNA residence time, improved cellular internalization, and also targeted siRNA transport. Depending on the charge of the polysaccharide, the interaction with siRNA differs, e.g., chitosan is positively charged, and the strong electrostatic interactions protects siRNA from degradation, but limits the release time. Other challenges are low stability at physiological pH, weak buffering capacity, and lack of cell specificity. Whereas, hyaluronic acid is anionic polysaccharide, which requires cationic components for the efficient interaction with siRNA yet has the potential for the specific delivery of siRNA to tumors. It shows better stability, low protein adsorption, and targeting capacity. Cyclodextrin is a cationic polymer with lasting biocompatibility, lack of immune stimulation, and the great resistance to degradation by human enzymes [152, 155]. The effective delivery of siRNA with therapeutics using chitosan and hyaluronic acid encourages the use of biopolymers for both in vitro and in vivo applications with promising anticancer gene silencing effects [156, 157]. An siRNA system targeted to Bcl2 oncogene was developed by the combination of chitosan and hyaluronic acid utilizing a cancer stem cell marker CD44 for treating bladder cancer. The fast cellular up taking capacity enabled chitosan as the gene carrier, whereas CD44 the cell surface transmembrane glycoprotein acted as the biomarkers for targeting siRNA into T24 bladder cancer cells by hyaluronic acid dialdehyde ensuring resistance to protein adsorption and prolonged circulation time. The in vivo experiments of the nano-system on a xenograft mice model showed target accumulation, inhibition of the targeted oncogene, and tumor growth suppression with no apparent organ toxicity. The in vitro and in vivo evaluations of the nano-system made of natural macromolecules displayed enhanced stability, high siRNA encapsulation efficiency, and low cytotoxicity, which is recommended for clinical application due to the ease of synthesis and high biological safety [158].
4.5 Potential of mucoadhesive materials for RNAi oral delivery
Mucoadhesive drug delivery is targeted directly to that mucus layer either to adhere or lyse the mucous layer. Mucoadhesive drug delivery is a popular drug delivery tool to deliver the drug to the GI tract. It interacts with the mucus layer of the epithelial cell of the intestine and increases the retention time drug. As a result, it increases the plasma half-life and therapeutic effect. Though mucoadhesive drug delivery system has been developed for oral, buccal, vaginal, nasal, and rectal for both local and systemic effect, it is mostly used in the disease of GI tract disease where the drug needs to be in the site for longer period of time [169, 170]. Several peptide, hormone, hydrophilic molecules have been delivered with mucoadhesive polymer to increase the residence time, increase permeation, owing hydrophilicity, large molecular weight, and enzymatic barrier [169, 171]. There are several theories to explain the mucoadhesive binding [172]. In a nutshell, (1) the wetting theory where it calculates the contact angle and spreading coefficient (Sb) to measure the adhesiveness, (2) the electrostatic theory, (3) the diffusion theory where the polymeric chain of the bio adhesive interpenetrates the glycoprotein mucin chain, (4) adsorption theory, and (5) fraction theory of adhesion [170, 173,174,175,176]. Mucoadhesive polymers have various hydrophilic groups like hydroxyl, carboxyl, amide, and sulfate [177]. With the help of these molecules, the polymers get attached with the mucus layer by the above-mentioned theories. The hydrophilic groups also help to get swelling of the molecules in contact with water and make the molecules exposed to the maximum adhesive site [178]. There are several mucoadhesive polymers that have been studied for oral drug delivery like PEG (polyethene glycol), PVA (polyvinyl alcohol), PAA (polyacrylic acid), PHEMA (poly hydroxyethyl methacrylate), chitosan, hydroxyethyl cellulose, hydroxypropyl cellulose, hydroxypropyl methylcellulose, methyl cellulose, glucan particle, hyaluronic acid, alginate, and poly-l-lysine [170, 179, 180]. Table 2 summarizes the oral siRNA delivery mostly for cancer treatment.
4.5.1 Chitosan as a mucoadhesive carrier for oral RNAi delivery
Chitosan is a widely used biomaterial for mucosal drug delivery due to its muco-permeable and mucoadhesive properties[181, 182]. Several review papers have described the use of chitosan polymer in the oral delivery of RNAi or siRNA [181, 183]. Chitosan is a naturally occurring cationic polysaccharide containing D-glucosamine and its units linked by 1–4-β-glycosidic bonds. It can be prepared by deacetylation of chitin in basic media, and it is nontoxic, biodegradable, and biocompatible, which makes it a good component for drug delivery [184, 185]. Because of its cationic properties, it can easily bind with negatively charged mucin by electrostatic interaction and penetrate the mucosal membrane [186]. Chitosan is ideal for siRNA delivery because of its cationic charge, low toxicity, and biocompatibility [187]. Due to the high positive charge of chitosan, it forms polyplex with negatively charged oligonucleotide or siRNA in the aqueous media that can facilitate drug transport and increase residence time at the epithelial surface, respectively [181, 188]. Katas and Alpar first investigated the use of chitosan to deliver siRNA in vitro [189]. However, the nanoparticle formation is highly dependent on the size of siRNA and the weight of chitosan. Katas et al. showed that chitosan Mw < 110 kDa produce smaller size nanoparticle than compared to the higher Mw (270 kDa) chitosan [189]. Whereas, Liu et al. indicated that the chitosan molecules (Mw 64.8–170 kDa), 5–10 times the length of the siRNA (Mw of 13.36 kDa), could form stable complexes with siRNA through electrostatic forces resulting in high gene silencing efficiency in H1299 human lung carcinoma cells [190]. Chitosan/siRNA nanoparticles have been found to be more stable in the mice body at least up to 5 h after oral delivery than naked siRNA [43]. It has been observed that ternary polymeric nanoparticles formed by thiolated trimethyl chitosan (TTMC) with tripolyphosphate (TPP) provide structural stability and protect siRNA in the intestinal tract. TTMC/siRNA/TPP nanoparticles mediated siRNA delivery was shown higher permeability through rat ileum and high systemic biodistribution after oral administration [191]. Chitosan-based nanoparticles have been used for the successful delivery of siRNA for various diseases like IBD and S.H. Kang at el. (2017) found that oral delivery of Au—siRNA nanoparticle conjugated with glycol chitosan—taurocholic acid was able to treat colorectal liver metastasis in mice. They used Akt2 siRNA for the treatment, and with their engineered vehicle, they found a reduction of the expression of Akt2 and an improvement of cancer by inducing the apoptosis [159]. Another study investigated oral delivery of shRNA and siRNA with galactose-modified trimethyl chitosan-cysteine (GTC) conjugated nanoparticle for hepatoma treatment. They found that with survivin shRNA (iSur-pDNA) and vascular endothelial growth factor (VEGF) siRNA (siVEGF) loaded NPs was stable in GI tract fluid, and they had more intestinal permeability than naked siRNA in the GI tract [160]. Chitosan siRNA has also been delivered orally to knockdown tumor necrosis alpha (TNF-α), which plays an important role in gastric cancer progression [192, 193]. The oral delivery of mannose-modified trimethyl chitosan-cysteine (MTC) NPs loaded siRNA was found stable in rat intestine and was able knockdown TNF-α. Chitosan-coated siRNA-loaded lanthanum phosphate NPs showed higher efficacy in the treatment of colorectal cancer. Chitosan was coated to form a mucoadhesive out layer of NPs. Several studies reported the downregulation of let-7a, miR-34a, Cyclin D1, Bcl-2, and Caspase-3 effects of lanthanum ions [194, 195]. The chitosan siRNA-loaded lanthanum phosphate NPs were able to give a synergistic effect to treat colorectal cancer in C57BL/6 tumor-bearing mice [161]. Another group of researchers used layering of folic acid conjugated chitosan and alginate for attaining the mucoadhesive properties and entrapped oxaliplatin and signal transducer and activator of transcription 3 (STAT3) siRNA on it for treatment of colon cancer in BALB/c mice. They found a better therapeutic effect with oral administration of nanoparticles compared to intravenous one [162]. Codelivery of telomerase reverse transcriptase siRNA and paclitaxel, encapsulated in chitosan coated N-((2-hydroxy-3-trimethylammonium) propyl) (HTCC), showed significant tumor suppression both in vitro and in vivo LLC tumor-bearing mice model. The outer coating of HTCC prevented siRNA from enzymatic degradation and improved siRNA permeability in intestine tract. The Caco2 monolayer transportation shows higher transportation of nanoparticle carrying siRNA than free siRNA which also corresponds with the in vivo transportation study [163]. To treat acute hepatic injury in rat models, an oral delivery of chitosan nanoparticles with TNF-α siRNA targeting macrophages were developed by He et al., to limit the TNF-α expression focussing the anti-inflammatory therapy [196]. Survivin shRNA-expression pDNA (iSur-pDNA) along with vascular endothelial growth factor (VEGF) siRNA was used in the hepatoma treatment. The carrier was made of galactose-modified trimethyl chitosan-cysteine (GTC) conjugates electrostatically conjugates with iSur-pDNA and siVEGF, where the synergistic system showed excellent stability and features supporting cellular uptake, nuclear distribution, and down-regulation of target genes, all directing the inhibition of tumor progression. Oral delivery of the iSur-pDNA and siVEGF nanocomplex exhibited synergistic effects in tumor-induced mice with targeted accumulation in tumors while, silencing survivin and VEGF-supported apoptosis, prevented angiogenesis, and resulted in tumor regression [160]. A similar shRNA-based oral delivery system was developed by Zheng et al., a complex made of chitosan–histidine–cysteine (CHC) for oral delivery of survivin shRNA—expressing plasmid DNA (shSur-pDNA) to support hepatoma regression. The multistep modification with histidine and cysteine improves the biocompatibility of the nanocomplex. In hepatoma-bearing mice, comparing with the control chitosan nanocomplex, the CHC nanocomplex showed enhanced shRNA delivery by better stability, easy internalization, improved endosomal escape, higher nuclear localization, and GSH-responsive release. This resulted in survivin-induced apoptosis, inhibition of tumor progression/proliferation, and thus resulting in the down-regulation of hepatoma tumor cells [167].
4.5.2 Hyaluronic acid as a mucoadhesive carrier for oral RNAi delivery
Hyaluronic acid (HA) is a naturally occurring polymer in the body which helps in tissue hydration, water transport, viscoelasticity, wound healing, and inflammation [197, 198]. Its non-immunogenicity and properties of easy modification make it an ideal component for bioengineered drug delivery [199]. One study shows that the addition of the thiol group with HA improves the muco-adhesiveness, enzyme inhibitory action, enhance permeation, and controlled release of the compound [200]. Researchers have been using HA as a carrier of siRNA for cancer treatment [201, 202]. A study showed that HA coating for mesoporous silica nanoparticle carrying TH287 and MDR1 siRNA provides a better therapeutic effect than naked siRNA. Oral delivery of TH287 and MDR1 siRNA encapsulated MSN with HA coating successfully induced apoptosis and kills cancer cells in both in vitro and in vivo oral cancer mice models. They stated that HA coating provides stability of siRNA in the intestine [164]. Another group of researchers stated that trimethyl chitosan-thiolated chitosan-TAT -hyaluronic acid nanoparticles (NPs) are appropriate carriers for siRNA delivery. They used thiolated chitosan to improve the mucoadhesion which provided stability of STAT3 and PD-L1 siRNA and produced a better effect in breast cancer treatment [203]. Another study suggests HA-coated siRNA causes 90% of siRNA releases in the tumor cells due to the presence of hyaluronidase in a tumor cell. Oral delivery of AKT siRNA coated with hyaluronic acid-taurocholic acid nanocomplex showed more than 1 mm of reduction in tumor size in a colorectal liver metastasis mice model [165].
4.6 Non-viral bacterial carrier
Bacteria are a widely used non-viral vector. They are a useful tool in biotechnology and have been used in the understanding of gene and gene function. Bacteria are used as delivery agents for vaccines, chemicals, therapeutic proteins, or even as gene therapy vectors. Bacteria have been found to be useful for the delivery of RNAi. Unlike some viral vectors, bacteria do not integrate genetic material into the host genome. They are less immunogenic and can be controlled with antibiotics or engineered to increase the safety using nutrients [204]. Nonpathogenic Escherichia coli has been used by researchers to deliver the shRNA orally against catenin beta-1 in human colon cancer xenograft mice model [168]. A different shRNA drug CEQ508 was investigated by Osmond et al. for the treatment of a rare hereditary disorder, familial adenomatous polyposis (FAP), often related to colorectal cancer. CEQ508 contains live-attenuated Escherichia coli engineered to produce plasmid pMBV43-H3 and deliver β-catenin shRNA to facilitate RNA interference at gastrointestinal epithelium. The oral delivery of the CEQ508 in preclinical and clinical models exhibited an acceptable safety profile [205]. The results of the first in human investigations of the oral delivery of CEQ508 in FAP patients lead to the new ideas of combination drug with Celecoxib/Lisinopril (IT-102) against FAP [206].
Saccharomyces cerevisiae (yeast) is used as an efficient encapsulating agent for the in vivo delivery of shRNA. A recombinant yeast system was used for the oral delivery of CD 40- the shRNA of immune-associated gene, related to apoptosis of tumor cells and immunomodulation. The in vivo results showed DC-specific gene silencing corresponding to efficient shRNA delivery [207]. Another oral drug carrier system for the delivery of survivin shRNA-expression pDNA (iSur-pDNA) along with vascular endothelial growth factor (VEGF) siRNA was used in the hepatoma treatment. The carrier was made of galactose-modified trimethyl chitosan-cysteine (GTC) conjugates electrostatically conjugates with iSur-pDNA and siVEGF, where the synergistic system showed excellent stability and features supporting cellular uptake, nuclear distribution, and down-regulation of target genes, all directing the inhibition of tumor progression. Oral delivery of the iSur-pDNA and siVEGF nanocomplex exhibited synergistic effects in tumor-induced mice with targeted accumulation in tumors while, silencing survivin and VEGF-supported apoptosis, prevented angiogenesis and resulted in tumor regression [208].
Yeast-encapsulated non-virus-mediated interleukin-1β shRNA (IL-1β shRNA) was investigated in the treatment of post-traumatic osteoarthritis by oral delivery. The yeast encapsulation helps to improve the biocompatibility of the microcapsule, being resistant to the disintegration of shRNA during digestion in the stomach and intestine. Also, yeast evades unwanted gene interactions and tumor formation. Moreover, the presence of beta-glucans in yeast enables the macrophage targeting due to the glucan receptors on the surface of macrophage, which enables targeted gene delivery and immune regulation. IL-1β shRNA significantly reduced the inflammatory responses by down-regulating the IL-1β expression of macrophages in the intestine, bone marrow, and articular cartilage. Upon the treatment, a reduction in the expression of osteoarthritis markers Col X and MMP13 was observed, indicating the effectiveness of this yeast—shRNA therapeutic microcapsules in protecting the articular cartilage joints of the mice models [209, 210]. In the same way, for the treatment of high-fat diet (HFD) induced obesity, the oral delivery of yeast-encapsulated shRNA (IL-1β shRNA interference vectors) microcapsules were examined by Zhang et al. In the investigation, the microcapsules were orally administered in HFD obese mice models in a dose of 10 mg/kg every 2 days from day 1 to day 29, and the body weight, food intake, and blood glucose were recorded weekly. On the 29th day, the serum samples and tissues and organs of the models were collected for analysis. When compared to the control animals, the treated group showed controlled growth of adipocytes thus regulating body weight and weight of abdominal fat, liver, and lungs. The presence of the microcapsule prevents the degradation of shRNA and thus inhibited the IL-1β expression in the small intestine and intestinal macrophages. The serum analysis displayed regulated blood glucose concentration as well as cytokines expression. Furthermore, from the immunohistochemistry evaluation, the expression of MMP13 and IL-1β (cartilage injury-related proteins) was found to be lesser, which improves the therapeutic potential of the microcapsule by relieving the articular cartilage degeneration triggered by obesity [208].
5 Chemical modification of siRNA for oral delivery
Another interesting siRNA drug delivery system is the siRNA conjugation method. siRNA can be conjugated with various bioactive molecules, lipids, polymers, peptides, antibodies, and inorganic nanostructured materials [211]. The siRNA-conjugated delivery system enhanced the pharmacokinetics, cellular uptake, and target specificity. Various types of siRNA conjugated delivery systems have been reported which provide efficient delivery of siRNA and target the cells and tissue. siRNA has 4 terminal ends which acts as potential conjugation sites. 3′- and 5′ terminus of the sense strand and the 3′-terminus of the antisense strand are promising sites for conjugation with negligible effect on RNAi activity [212]. The conjugations mostly used cleavable linkage such as acid labile and reducible bonds. An example of disulfide linkages is acid labile. siRNA conjugates are further classified as lipophile-siRNA conjugate, peptide-siRNA conjugate, and PEG-siRNA conjugate. For targeted siRNA delivery ligand peptide-siRNA conjugates, antibody-siRNA conjugate, aptamer-siRNA conjugate, and targetable polyelectrolyte complex micelles are the potential options (Fig. 8) [211, 213].
Scheme shows the rationale and designing strategies of the siRNA conjugated delivery system. Adapted with permission from [213].
Springer et al. documented a GaINAc-siRNAIn conjugation in the delivery of RNAi therapeutics. In 1971, clinical possibilities of ASGPR were realized through the delivery of nonglycoproteins to the liver through conjugation to asialofetuin. In 1978, they demonstrated the targeted delivery by conjugation. The first targeted delivery of drug to hepatocytes in vivo was reported in 1979 by injection of asialofetuin-linked trifluoro thymidine which reduced hepatic ectromelia viral DNA replication threefold in rats. Later, low-density lipoprotein and diphtheria toxin delivery were also achieved [214].
Antibody-siRNA conjugates are a promising strategy to enhance siRNA delivery for gene silencing in cancer treatment. Antibody physiochemical properties and route of administration are the critical factors that impact therapeutic potential. The type of antibody and their efficacy in conjugation play a crucial role in tolerability and potential [215]. High affinity and control delivery of antibodies or diverse targets are effective for many diseases. Antibodies and payloads are chemically conjugated with linker. Linker plays critical roles in stability. Lysine or cysteines are used in linkage. Linkers’ physicochemical properties directly affect siRNA and antibody releases specifically in a targeted cell [215]. There should not be an inverse effect of conjugation. The complex formulation of conjugation systems may lead heterogeneous aggregates. THIOMAB is a new technology to covalent conjugation of antibody and siRNA. Amine-tagged siRNA is reactive with the NHS linker which reacts with the thiol group of THIOMABs. This technology significantly enhances the conjugation strategies of siRNA-antibody. It is well known that antibodies are good targeting agent in siRNA-targeted delivery [216]. Antigens are used as a carrier for targeted siRNA such as HER-2 and EGFR. HER-2 siRNA loaded liposome by functionalizing transferrin receptor-specific antibody results silence of HER-2 gene [217]. The antibody-siRNA conjugated delivery system studied for targeting cancer are F5-P/PLK1-siRNA, STAT3 siRNA-hu3S193, F105-p HIV env, KRAS-siRNA-anti-EGFR, Dig-siRNA-Nu647, and antibody-siRNA conjugates [215].
Zhou et al. used the aptamer-siRNA conjugation for transcriptional regulation of HIV-I [218]. This further opens a new window for the investigation of receptor-targeted aptamer-siRNA conjugation system for cancer therapy. The vascular endothelial growth factor receptor 2 (VEGFR2) is a promising target for the treatment of angiogenesis of non-small cell lung cancer. Liao et al. design the bivalent cyclic RGD-siRNA conjugates to enhance the apatinib anti-tumor potential to inhibit VEGFR2 in NSCLC xenografts [219]. Interestingly, biRGD-siVEGFR2 reduced the nephrotoxicity of apatinib [219]. This study proposed the low-dose apatinib as a clinical anti-tumor therapy.
Peptide is also used to conjugate with siRNA for targeted delivery for cancer treatment. Arg-Gly-Asp (RGD) peptide targets tumor vasculature expressing integrin. VEGF siRNA is selectively delivered to the tumor through RGD peptide with PEGylated PEI conjugation. It inhibited murine neuroblastoma tumor growth in mice after i.v. administration [220]. Yao et al. used siRNA against PLK1 coupled with anti-HER2 scFv which could inhibit the growth of HER2 primary breast cancer in vitro and in vivo. The formulation showed a 72-h half-life which is significantly enhanced compared to naked siRNA which has 1.5 h [221]. The complex showed a high level of delivery. Xu et al. demonstrated the GEII peptide conjugated nanoliposomes to enhance the combinational therapeutics efficacy of docetaxel and siRNA in laryngeal cancers [222].
Another interesting molecule to target cancer gene is folate receptor. Folate receptors are overexpressed in many cancer cells. FA is facile to conjugate the surface of liposome and polymeric siRNA nanoparticles. FA-PEI enhanced the receptor-mediated endocytosis. Compared to other strategies, folate-conjugated targeted siRNA delivery is well-studied [223]. Similar strategies are widely used for drug delivery through conjugation.
Cholesterol-siRNA conjugation also showed promising potential in silencing apolipoprotein B in mice when administrated via intravenously; cholesterol-siRNA conjugation enhances the distribution and cellular uptake of siRNA [224]. Single intrastriatal injection silenced a mutant huntingtin gene in mice [225]. RNA aptamer is very selective and used to target tissues and cells such as prostate cancer cells. Aptamer-based siRNA conjugation system is also used to suppress HIV infection. Anti-gp120 RNA aptamer is used to conjugate siRNA. It showed great potential in vitro and in vivo [226].
Biopharmaceutical industries have been investigating the nucleic acid-based biopharmaceuticals. A number of RNAi therapeutics are under clinical trials. Lee et al. documented the preclinical siRNA-based conjugation systems for RNAi therapy [227]. RNAi offers several benefits in cancer therapy such as effective control of tumor growth, specificity, and low cost. RNAi-based therapeutics market keeps growing globally. For example, a billion-dollar business has been developed since the beginning of COVID-19 through the development of mRNA-based vaccines.
Only 4 small interfering RNA (siRNA)-based therapies have been approved (patisiran, givosiran, lumasiran, and inclisiran) and are FDA-approved for managing rare metabolic ailments; there are several other candidates in phase 3 trials. Global RNAi Therapeutics Market Insights and Forecast Report 2022–2026 shows that 7.8 million dollars were spent in 2022 which may reach 11.5 million by 2026 (progressing CAGR of 10.19%) [228]. It concludes that siRNA-based therapeutics are potential options for cancer therapy in the future.
6 Future perspectives
In the past decade, preclinical and clinical studies have demonstrated the potential of RNA therapeutics to treat diseases. However, to bring them to clinic, several advancements are needed. The first one is understanding the interaction of nanocarriers with RNA and their effect on targeting and tolerability, effect of chemical modification of RNA and its impact on the stability, and off-targeting. The last one is, we should understand the efficacy and tolerability of RNA therapeutics in a small animal model and non-human primates and humans. Furthermore, we need to develop small animal models that maximally predict the potential of RNA therapeutics in humans. Hence, through expanding the understanding of RNA formulation, RNA delivery system, nanocarrier, and their interaction with the body and interaction of one another will benefit the development of effective next-generation gene therapeutics.
Although various formulations have been developed, the focus should have remained on the biological stability, specificity, and safety of nanocarriers, which can be translatable from bench to industry. The key challenge of RNA therapeutics commercialization is formulation techniques. Among the various methods developed for RNA therapeutics formulation, many strategies limited their use in industrial application due to various challenges. For example, very complex formulations are difficult to scale up for industrial applications and are expensive. Moreover, it is a huge challenge to get the regulatory approvals due to various limitations. Furthermore, tumor or site of disease targeting approaches needs to be investigated using the as simple as formulation with high therapeutic function by natural mechanism.
The strategies should be robust and consistently produce the formulation at a production scale that range from early-phase development to clinical applications. The great effect needs to be investigated towards the development of strategies for efficient formulation. Recently, the microfluidic method was developed which is continuous and scalable for industrial applications [229]. This technique addresses the clinical need of scalable LNP production of RNA therapeutics and vaccines. However, the same strategy is not suitable for different formulations. The use of a 3D cancer model instead of an animal model is also an emerging field that could be used for siRNA treatment efficacy [230, 231]. The efficacy of RNA therapeutics also depends on the formulation strategies and disease of interest. Hence, extensive investigation needs to be conducted to develop the formulation for various diseases. Positive results from the siRNA therapeutics from clinical trials will boost the confidence of the siRNA therapeutic industries to invest in siRNA cancer therapeutics.
We strongly believe that artificial intelligence (AI) is showing tremendous results in biomedical application ranging from identifying the potential drug molecule to their therapeutic potential in the human body. AI has already been used for treatment strategies, prediction of disease progression, rapid identification of target, and drug delivery system design [232]. AI needs to be explored towards the RNAi delivery, which may provide the therapeutic potential of siRNA. Very recently, artificial intelligence, mathematic modeling, and machine learning approach have been used for targeted non-viral gene delivery [233,234,235,236]. This emerging field has huge potential in delivering oral gene therapy which needs extensive research.
Current progress, interdisciplinary collaboration, and investigation towards the development of next-generation therapeutics using siRNA have a great future.
7 Conclusion
RNA therapeutics are a potent and versatile candidate with the potential to replace small molecule drugs and proteins. RNA therapeutics treats the illnesses through tuning and controlling the expression of the disease-related gene. To knockdown the gene can be achieved using siRNA, shRNA, and miRNA. Cancer is a genetic disease, where there are changes in the gene that controls the cell growth and multiplication. That is why selective gene silencing through the RNAi mechanism has been revolutionary in the cancer treatment lately. However, successful delivery of nucleic acid is still a challenge, in terms of clinical translation, due to both extracellular (enzymatic degradation, poor internalization) and intracellular barriers such as lysosomal degradation. Cancer chemotherapy is a time-consuming process where patients must pay a visit to the clinic for each cycle of intravenous chemotherapy. That is why oral chemotherapy has more patient’s compliance due to its ease of administration and painless application. However, in oral delivery, nucleic acid-based therapeutics come across various hurdles to reach the site of action like thick mucus layer, intestinal peristalsis, harsh pH, and nuclease enzyme. Successful oral delivery of RNAi (siRNA) with good bioavailability would be groundbreaking. To overcome these barriers, different nanocarrier systems and chemical modifications could be beneficial.
In this article, we have comprehensively discussed the oral RNAi delivery strategies for effective therapy of a range of diseases. We briefly insight into the range of barriers in the gastrointestinal tract for oral RNAi delivery. We also summarized the effect of physicochemical properties of the RNAi oral delivery system on the efficiency of oral RNAi delivery. This concluded that the small intestine is the most favorable site for RNAi delivery due to long retention time, extensive surface area, high epithelial permeability, and systemic absorption in payers’ patches.
The impact of oral RNAi delivery mediated by oral drug delivery carriers has high significance to improve the oral local and systemic delivery of RNAi-based therapeutics. The adverse side effects can be controlled or overcome through the development of strategies of modification of existing nanocarriers without altering the RNAi physicochemical properties. More than 10,000 reports have been published based on oral RNAi delivery systems in past decades. Here, in this review, we have summarized a wide range of siRNA delivery systems and have proposed some very emerging systems that have been shown as very promising due to their proven potential in pre-clinical and clinical studies. Despite of great development on oral RNAi delivery using the above-discussed vehicles, the existing gap and unmet need still limit their translation from bench to bedside. There is a great scope to explore the potential of liposomes or lipid-based nanoparticle-based RNAi oral delivery for various chronic systemic and GI-based local diseases.
To date, three siRNA therapeutics have been approved by the FDA for commercial use. In addition, more than 50 active/recruiting clinical trials are underway. Several candidates are waiting to be licensed to conduct clinical studies. Approval of siRNA therapeutics by the FDA may increase the number in the coming years. Recent advances of RNA therapeutics led to the US-FDA approval of Onpattro, a lipid nanoparticles-based siRNA therapeutic, and Givlaari, a siRNA conjugate with N-acetyl galactosamine. Recently, mRNA vaccines developed by Moderna and Pfizer/BioNTech received the emergency use.
References
Fire, A., Xu, S., Montgomery, M. K., Kostas, S. A., Driver, S. E., & Mello, C. C. (1998). Potent and specific genetic interference by double-stranded RNA in Caenorhabditis elegans. Nature, 391(6669), 806–811. https://doi.org/10.1038/35888
Wang, J., & Barr, M. M. (2005). RNA interference in Caenorhabditis elegans. Methods in Enzymology, 392, 36–55. https://doi.org/10.1016/S0076-6879(04)92003-4
Tatiparti, K., Sau, S., Kashaw, S. K., & Iyer, A. K. (2017). siRNA delivery strategies: A comprehensive review of recent developments. Nanomaterials (Basel, Switzerland), 7(4), 77. https://doi.org/10.3390/nano7040077
Resnier, P., Montier, T., Mathieu, V., Benoit, J.-P., & Passirani, C. (2013). A review of the current status of siRNA nanomedicines in the treatment of cancer. Biomaterials, 34(27), 6429–6443. https://doi.org/10.1016/j.biomaterials.2013.04.060
Gavrilov, K., & Saltzman, W. M. (2012). Therapeutic siRNA: Principles, challenges, and strategies. Yale Journal of Biology and Medicine, 85(2), 187–200.
Hammond, S. M., Caudy, A. A., & Hannon, G. J. (2001). Post-transcriptional gene silencing by double-stranded RNA. Nature Reviews Genetics, 2(2), 110–119. https://doi.org/10.1038/35052556
Zamore, P. D., Tuschl, T., Sharp, P. A., & Bartel, D. P. (2000). RNAi: Double-stranded RNA directs the ATP-dependent cleavage of mRNA at 21 to 23 nucleotide intervals. Cell, 101(1), 25–33. https://doi.org/10.1016/S0092-8674(00)80620-0
Strapps, W. R., Pickering, V., Muiru, G. T., Rice, J., Orsborn, S., Polisky, B. A., Sachs, A., & Bartz, S. R. (2010). The siRNA sequence and guide strand overhangs are determinants of in vivo duration of silencing. Nucleic Acids Research, 38(14), 4788–4797. https://doi.org/10.1093/nar/gkq206
Hammond, S. M., Bernstein, E., Beach, D., & Hannon, G. J. (2000). An RNA-directed nuclease mediates post-transcriptional gene silencing in Drosophila cells. Nature, 404(6775), 293–296. https://doi.org/10.1038/35005107
Hammond, S. M., Boettcher, S., Caudy, A. A., Kobayashi, R., & Hannon, G. J. (2001). Argonaute2, a link between genetic and biochemical analyses of RNAi. Science, 293(5532), 1146–1150. https://doi.org/10.1126/science.1064023
Oh, Y.-K., & Park, T. G. (2009). siRNA delivery systems for cancer treatment. Advanced Drug Delivery Reviews, 61(10), 850–862. https://doi.org/10.1016/j.addr.2009.04.018
Doi, N., Zenno, S., Ueda, R., Ohki-Hamazaki, H., Ui-Tei, K., & Saigo, K. (2003). Short-interfering-RNA-mediated gene silencing in mammalian cells requires dicer and eIF2C translation initiation factors. Current Biology, 13(1), 41–46. https://doi.org/10.1016/S0960-9822(02)01394-5
Afrin, H., Salazar, C. J., Kazi, M., Ahamad, S. R., Alharbi, M., & Nurunnabi, M. (2022). Methods of screening, monitoring and management of cardiac toxicity induced by chemotherapeutics. Chinese Chemical Letters. https://doi.org/10.1016/j.cclet.2022.01.011
Huda, M. N., Deaguro, I. G., Borrego, E. A., Kumar, R., Islam, T., Afrin, H., Varela-Ramirez, A., Aguilera, R. J., Tanner, E. E. L., & Nurunnabi, M. (2022). Ionic liquid-mediated delivery of a BCL-2 inhibitor for topical treatment of skin melanoma. Journal of Controlled Release, 349, 783–795.
Afrin, H., Huda, M. N., Islam, T., Oropeza, B. P., Alvidrez, E., Abir, M. I., Boland, T., Turbay, D., & Nurunnabi, M. (2022). Detection of anticancer drug-induced cardiotoxicity using VCAM1-targeted nanoprobes. ACS Applied Materials & Interfaces, 14(33), 37566–37576. https://doi.org/10.1021/acsami.2c13019
de Fougerolles, A., Vornlocher, H.-P., Maraganore, J., & Lieberman, J. (2007). Interfering with disease: A progress report on siRNA-based therapeutics. Nature Reviews Drug Discovery, 6(6), 443–453.
Ye, Q.-F., Zhang, Y.-C., Peng, X.-Q., Long, Z., Ming, Y.-Z., & He, L.-Y. (2012). Silencing Notch-1 induces apoptosis and increases the chemosensitivity of prostate cancer cells to docetaxel through Bcl-2 and Bax. Oncology Letters, 3(4), 879–884.
Bai, Z., Zhang, Z., Qu, X., Han, W., & Ma, X. (2012). Sensitization of breast cancer cells to taxol by inhibition of taxol resistance gene 1. Oncology Letters, 3(1), 135–140.
Naghizadeh, S., Mohammadi, A., Baradaran, B., & Mansoori, B. (2019). Overcoming multiple drug resistance in lung cancer using siRNA targeted therapy. Gene, 714, 143972.
Meng, H., Mai, W. X., Zhang, H., Xue, M., Xia, T., Lin, S., Wang, X., Zhao, Y., Ji, Z., Zink, J. I., & Nel, A. E. (2013). Codelivery of an optimal drug/siRNA combination using mesoporous silica nanoparticles to overcome drug resistance in breast cancer in vitro and in vivo. ACS Nano, 7(2), 994–1005.
Schiffelers, R. M., Ansari, A., Xu, J., Zhou, Q., Tang, Q., Storm, G., Molema, G., Lu, P. Y., Scaria, P. V., & Woodle, M. C. (2004). Cancer siRNA therapy by tumor selective delivery with ligand-targeted sterically stabilized nanoparticle. Nucleic Acids Research, 32(19), e149–e149.
Mitragotri, S., Burke, P. A., & Langer, R. (2014). Overcoming the challenges in administering biopharmaceuticals: Formulation and delivery strategies. Nature Reviews Drug Discovery, 13(9), 655–672. https://doi.org/10.1038/nrd4363
Caffarel-Salvador, E., Abramson, A., Langer, R., & Traverso, G. (2017). Oral delivery of biologics using drug-device combinations. Current Opinion in Pharmacology, 36, 8–13. https://doi.org/10.1016/j.coph.2017.07.003
Zelikin, A. N., Ehrhardt, C., & Healy, A. M. (2016). Materials and methods for delivery of biological drugs. Nature Chemistry, 8(11), 997–1007. https://doi.org/10.1038/nchem.2629
Morishita, M., & Peppas, N. A. (2006). Is the oral route possible for peptide and protein drug delivery? Drug Discovery Today, 11(19–20), 905–910. https://doi.org/10.1016/j.drudis.2006.08.005
Singh, A., Trivedi, P., & Jain, N. K. (2018). Advances in siRNA delivery in cancer therapy. Artificial Cells, Nanomedicine, and Biotechnology, 46(2), 274–283. https://doi.org/10.1080/21691401.2017.1307210
Kirchhoff, F. (2008). Silencing HIV-1 in vivo. Cell, 134(4), 566–568. https://doi.org/10.1016/j.cell.2008.08.004
Xu, C., & Wang, J. (2015). Delivery systems for siRNA drug development in cancer therapy. Asian Journal of Pharmaceutical Sciences, 10(1), 1–12. https://doi.org/10.1016/j.ajps.2014.08.011
Fire, A., Xu, S., Montgomery, M. K., Kostas, S. A., Driver, S. E., & Weng, Y. (1998). Potent and specific genetic interference by double-stranded RNA in Caenorhabditis elegans. Nature, 391(6669), 806–811. https://doi.org/10.1038/35888
Hamilton, A. J., & Baulcombe, D. C. (1999). A species of small antisense RNA in posttranscriptional gene silencing in plants. Science, 286(5441), 950–952. https://doi.org/10.1126/SCIENCE.286.5441.950/SUPPL_FILE/1042575S1_THUMB.GIF
Tuschl, T. (2001). RNA interference and small interfering RNAs. ChemBioChem, 2(4), 239–245. https://doi.org/10.1002/1439-7633(20010401)2:4%3c239::AID-CBIC239%3e3.0.CO;2-R
Eisenstein, M. (2019). Pharma’s roller-coaster relationship with RNA therapies. Nature, 574(7778), S4–S6. https://doi.org/10.1038/D41586-019-03069-3
Hu, B., Zhong, L., Weng, Y., Peng, L., Huang, Y., Zhao, Y., & Liang, X. J. (2020). Therapeutic siRNA: State of the art. Signal Transduction and Targeted Therapy, 5(1), 1–25. https://doi.org/10.1038/s41392-020-0207-x
Huang, Y. Y. (2019). Approval of the first-ever RNAi therapeutics and its technological development history. Progress in Biochemistry and Biophysics, 46, 313–322.
Weng, Y. (2019). RNAi therapeutic and its innovative biotechnological evolution. Biotechnology Advances, 37, 801–825.
Blythe, R. H. (1956). Sympathomimetic preparation. Google Patents.
Barenholz, Y. C. (2012). Doxil®—The first FDA-approved nano-drug: Lessons learned. Journal of Controlled Release, 160(2), 117–134.
Abuchowski, A., McCoy, J. R., Palczuk, N. C., van Es, T., & Davis, F. F. (1977). Effect of covalent attachment of polyethylene glycol on immunogenicity and circulating life of bovine liver catalase. Journal of Biological Chemistry, 252(11), 3582–3586.
Cordes, R. M., Sims, W. B., & Glatz, C. E. (1990). Precipitation of nucleic acids with poly (ethyleneimine). Biotechnology Progress, 6(4), 283–285. https://doi.org/10.1021/bp00004a009
Jones, D. H., Corris, S., McDonald, S., Clegg, J. C. S., & Farrar, G. H. (1997). Poly (DL-lactide-co-glycolide)-encapsulated plasmid DNA elicits systemic and mucosal antibody responses to encoded protein after oral administration. Vaccine, 15(8), 814–817.
Aouadi, M., Tesz, G. J., Nicoloro, S. M., Wang, M., Chouinard, M., Soto, E., et al. (2009). Orally delivered siRNA targeting macrophage Map4k4 suppresses systemic inflammation. Nature, 458(7242), 1180–1184. https://doi.org/10.1038/nature07774
Laroui, H., Theiss, A. L., Yan, Y., Dalmasso, G., Nguyen, H. T. T., Sitaraman, S. V., & Merlin, D. (2011). Functional TNFα gene silencing mediated by polyethyleneimine/TNFα siRNA nanocomplexes in inflamed colon. Biomaterials, 32(4), 1218–1228. https://doi.org/10.1016/j.biomaterials.2010.09.062
Ballarín-González, B., Dagnaes-Hansen, F., Fenton, R. A., Gao, S., Hein, S., Dong, M., & Howard, K. A. (2013). Protection and systemic translocation of siRNA following oral administration of chitosan/siRNA nanoparticles. Molecular Therapy – Nucleic Acids, 2, e76. https://doi.org/10.1038/mtna.2013.2
Tahara, K., Samura, S., Tsuji, K., Yamamoto, H., Tsukada, Y., Bando, Y., Tsujimoto, H., Morishita, R., & Kawashima, Y. (2011). Oral nuclear factor-κB decoy oligonucleotides delivery system with chitosan modified poly (D, L-lactide-co-glycolide) nanospheres for inflammatory bowel disease. Biomaterials, 32(3), 870–878.
Zhang, J., Tang, C., & Yin, C. (2013). Galactosylated trimethyl chitosan–cysteine nanoparticles loaded with Map4k4 siRNA for targeting activated macrophages. Biomaterials, 34(14), 3667–3677.
Khare, P., Dave, K. M., Kamte, Y. S., Manoharan, M. A., O’Donnell, L. A., & Manickam, D. S. (2021). Development of lipidoid nanoparticles for siRNA delivery to neural cells. The AAPS journal, 24(1), 8.
Taira, M. C., Chiaramoni, N. S., Pecuch, K. M., & Alonso-Romanowski, S. (2004). Stability of liposomal formulations in physiological conditions for oral drug delivery. Drug Delivery, 11(2), 123–128.
Miyata, K. (2021). Nucleic acid delivery across biological barriers. Yakugaku Zasshi, 141(5), 635–639. https://doi.org/10.1248/yakushi.20-00219-2
Kriegel, C., Attarwala, H., & Amiji, M. (2013). Multi-compartmental oral delivery systems for nucleic acid therapy in the gastrointestinal tract. Advanced Drug Delivery Reviews, 65(6), 891–901. https://doi.org/10.1016/j.addr.2012.11.003
Rosenmayr-Templeton, L. (2013). The oral delivery of peptides and proteins: Established versus recently patented approaches. Pharmaceutical Patent Analyst, 2(1), 125–145. https://doi.org/10.4155/ppa.12.75
O’Driscoll, C. M., Bernkop-Schnürch, A., Friedl, J. D., Préat, V., & Jannin, V. (2019). Oral delivery of non-viral nucleic acid-based therapeutics - Do we have the guts for this? European Journal of Pharmaceutical Sciences, 133, 190–204. https://doi.org/10.1016/j.ejps.2019.03.027
Guyton, A. C., & Hall, J. E. (1986). Textbook of medical physiology. Elsevier and Saunders.
Bolondi, L., Bortolotti, M., Santi, V., Calletti, T., Gaiani, S., & Labò, G. (1985). Measurement of gastric emptying time by real-time ultrasonography. Gastroenterology, 89(4), 752–759. https://doi.org/10.1016/0016-5085(85)90569-4
Ensign, L. M., Cone, R., & Hanes, J. (2012). Oral drug delivery with polymeric nanoparticles: The gastrointestinal mucus barriers. Advanced drug delivery reviews, 64(6), 557–570. https://doi.org/10.1016/j.addr.2011.12.009
Kogan, A. N., & von Andrian, U. H. (2008). Microcirculation. In R. F. Tuma, W. N. Durán, & K. Ley (Eds.), Chapter 10 - Lymphocyte trafficking (2nd ed., pp. 449–482). Academic Press. https://doi.org/10.1016/B978-0-12-374530-9.00012-7
Boegh, M., & Nielsen, H. M. (2015). Mucus as a barrier to drug delivery – Understanding and mimicking the barrier properties. Basic & Clinical Pharmacology & Toxicology, 116(3), 179–186. https://doi.org/10.1111/bcpt.12342
Atuma, C., Strugala, V., Allen, A., & Holm, L. (2001). The adherent gastrointestinal mucus gel layer thickness and physical state in vivo. American Journal of Physiology-Gastrointestinal and Liver Physiology, 280(5), G922–G929.
Shen, L., & Sasakawa, C. (2009). Molecular mechanisms of bacterial infection via the gut. Springer.
Cone, R. A. (2009). Barrier properties of mucus. Advanced Drug Delivery Reviews, 61(2), 75–85.
Lieleg, O., & Ribbeck, K. (2011). Biological hydrogels as selective diffusion barriers. Trends in Cell Biology, 21(9), 543–551.
Witten, J., & Ribbeck, K. (2017). The particle in the spider’s web: Transport through biological hydrogels. Nanoscale, 9(24), 8080–8095.
Wang, Y.-Y., Schroeder, H. A., Nunn, K. L., Woods, K., Anderson, D. J., Lai, S. K., & Cone, R. A. (2016). Diffusion of immunoglobulin g in shed vaginal epithelial cells and in cell-free regions of human cervicovaginal mucus. PLoS ONE, 11(6), e0158338.
Witten, J., Samad, T., & Ribbeck, K. (2018). Selective permeability of mucus barriers. Current Opinion in Biotechnology, 52, 124–133. https://doi.org/10.1016/j.copbio.2018.03.010
Maturin, L., Sr., & Curtiss, R., III. (1977). Degradation of DNA by nucleases in intestinal tract of rats. Science, 196(4286), 216–218.
Hoerter, J. A. H., & Walter, N. G. (2007). Chemical modification resolves the asymmetry of siRNA strand degradation in human blood serum. RNA, 13(11), 1887–1893. https://doi.org/10.1261/rna.602307
Layzer, J. M., McCaffrey, A. P., Tanner, A. K., Huang, Z., Kay, M. A., & Sullenger, B. A. (2004). In vivo activity of nuclease-resistant siRNAs. RNA, 10(5), 766–771. https://doi.org/10.1261/rna.5239604
Geary, R. S., Khatsenko, O., Bunker, K., Crooke, R., Moore, M., Burckin, T., Truong, L., Sasmor, H., & Levin, A. A. (2001). Absolute bioavailability of 2′-O-(2-methoxyethyl)-modified antisense oligonucleotides following intraduodenal instillation in rats. Journal of Pharmacology and Experimental Therapeutics, 296(3), 898–904.
Bennett, K. M., Walker, S. L., & Lo, D. D. (2014). Epithelial microvilli establish an electrostatic barrier to microbial adhesion. Infection and immunity, 82(7), 2860–2871.
Goldberg, M. (2003). Gomez-Orellana I. Challenges for the oral delivery of macromolecules. Nature Reviews. Drug Discovery, 2, 289–295.
Luzio, J. P., Pryor, P. R., & Bright, N. A. (2007). Lysosomes: Fusion and function. Nature Reviews Molecular Cell Biology, 8(8), 622–632.
Maxfield, F. R., & McGraw, T. E. (2004). Endocytic recycling. Nature reviews Molecular cell biology, 5(2), 121–132.
Gu, F., Crump, C. M., & Thomas, G. (2001). Trans-Golgi network sorting. Cellular and Molecular Life Sciences CMLS, 58(8), 1067–1084.
Whitehead, K. A., Langer, R., & Anderson, D. G. (2009). Knocking down barriers: Advances in siRNA delivery. Nature reviews. Drug discovery, 8(2), 129–138. https://doi.org/10.1038/nrd2742
Patil, S., Gao, Y. G., Lin, X., Li, Y., Dang, K., Tian, Y., Zhang, W.-J., Jiang, S.-F., Qadir, A., & Qian, A.-R. (2019). The development of functional non-viral vectors for gene delivery. International Journal of Molecular Sciences, 20(21), 5491. https://doi.org/10.3390/ijms20215491
Puhl, D. L., D’Amato, A. R., & Gilbert, R. J. (2019). Challenges of gene delivery to the central nervous system and the growing use of biomaterial vectors. Brain Research Bulletin, 150, 216–230. https://doi.org/10.1016/j.brainresbull.2019.05.024
Kaczmarek, J. C., Kowalski, P. S., & Anderson, D. G. (2017). Advances in the delivery of RNA therapeutics: From concept to clinical reality. Genome medicine, 9(1), 60. https://doi.org/10.1186/s13073-017-0450-0
Saw, P. E., & Song, E.-W. (2020). siRNA therapeutics: A clinical reality. Science China Life Sciences, 63(4), 485–500. https://doi.org/10.1007/s11427-018-9438-y
Woodle, M. C., & Lu, P. Y. (2005). Nanoparticles deliver RNAi therapy. Materials Today, 8, 34–41.
Gupta, N., Rai, D. B., Jangid, A. K., Pooja, D., & Kulhari, H. (2019). Nanomaterials-based siRNA delivery: Routes of administration, hurdles and role of nanocarriers. In S. Singh & P. K. Maurya (Eds.), Nanotechnology in modern animal biotechnology: Recent trends and future perspectives (pp. 67–114). Springer. https://doi.org/10.1007/978-981-13-6004-6_3
Eloy, J. O., Petrilli, R., Raspantini, G. L., & Lee, R. J. (2018). Targeted liposomes for siRNA delivery to cancer. Current Pharmaceutical Design, 24(23), 2664–2672.
Etheridge, M. L., Campbell, S. A., Erdman, A. G., Haynes, C. L., Wolf, S. M., & McCullough, J. (2013). The big picture on nanomedicine: The state of investigational and approved nanomedicine products. Nanomedicine: Nanotechnology, Biology and Medicine, 9(1), 1–14.
Allen, T. M. (1997). Liposomes. Drugs, 54(4), 8–14.
Bozzuto, G., & Molinari, A. (2015). Liposomes as nanomedical devices. International Journal of Nanomedicine, 10, 975.
Kanasty, R., Dorkin, J. R., Vegas, A., & Anderson, D. (2013). Delivery materials for siRNA therapeutics. Nature Materials, 12(11), 967–977.
Xia, Y., Tian, J., & Chen, X. (2016). Effect of surface properties on liposomal siRNA delivery. Biomaterials, 79, 56–68.
Wang, C., Liu, Q., Zhang, Z., Wang, Y., Zheng, Y., Hao, J., Zhao, X., Liu, Y., & Shi, L. (2021). Tumor targeted delivery of siRNA by a nano-scale quaternary polyplex for cancer treatment. Chemical Engineering Journal, 425, 130590.
Hattori, Y., Tamaki, K., Sakasai, S., Ozaki, K., & Onishi, H. (2020). Effects of PEG anchors in PEGylated siRNA lipoplexes on in vitro gene-silencing effects and siRNA biodistribution in mice. Molecular Medicine Reports, 22(5), 4183–4196.
Lee, H., Lytton-Jean, A. K. R., Chen, Y., Love, K. T., Park, A. I., Karagiannis, E. D., Sehgal, A., Querbes, W., Zurenko, C. S., Jayaraman, M., Peng, C. G., Charisse, K., Borodovsky, A., Manoharan, M., Donahoe, J. S., Truelove, J., Nahrendorf, M., Langer, R., & Anderson, D. G. (2012). Molecularly self-assembled nucleic acid nanoparticles for targeted in vivo siRNA delivery. Nature Nanotechnology, 7(6), 389–393.
Shim, G., Choi, H., Lee, S., Choi, J., Yu, Y. H., Park, D.-E., Choi, Y., Kim, C.-W., & Oh, Y.-K. (2013). Enhanced intrapulmonary delivery of anticancer siRNA for lung cancer therapy using cationic ethylphosphocholine-based nanolipoplexes. Molecular Therapy, 21(4), 816–824.
Ball, R. L., Knapp, C. M., & Whitehead, K. A. (2015). Lipidoid nanoparticles for siRNA delivery to the intestinal epithelium: In vitro investigations in a Caco-2 model. PLoS ONE, 10(7), e0133154.
Ball, R. L., Bajaj, P., & Whitehead, K. A. (2018). Oral delivery of siRNA lipid nanoparticles: Fate in the GI tract. Scientific Reports, 8(1), 1–12.
Beuzelin, D., Pitard, B., & Kaeffer, B. (2019). Oral delivery of miRNA with lipidic aminoglycoside derivatives in the breastfed rat. Frontiers in physiology, 10, 1037.
Tavares, G. A., Torres, A., Le Drean, G., Queignec, M., Castellano, B., Tesson, L., Remy, S., Anegon, I., Pitard, B., & Kaeffer, B. (2022). Oral delivery of miR-320–3p with lipidic aminoglycoside derivatives at mid-lactation alters miR-320–3p endogenous levels in the gut and brain of adult rats according to early or regular weaning. International Journal of Molecular Sciences, 24(1), 191.
Chen, Q., Zhang, F., Dong, L., Wu, H., Xu, J., Li, H., Wang, J., Zhou, Z., Liu, C., Wang, Y., Liu, Y., Lu, L., Wang, C., Liu, M., Chen, X., Wang, C., Zhang, C., Li, D., Zen, K., Wang, F., Zhang, Q., & Wang, C.-Y. (2021). SIDT1-dependent absorption in the stomach mediates host uptake of dietary and orally administered microRNAs. Cell Research, 31(3), 247–258.
Çetin, M., Aytekin, E., Yavuz, B., & Bozdağ-Pehlivan, S. (2017). Nanoscience in targeted brain drug delivery. In Y. Gürsoy-Özdemir, S. Bozdağ-Pehlivan, & E. Sekerdag (Eds.), Nanotechnology methods for neurological diseases and brain tumors (pp. 117–147). Elsevier.
Min, H. S., Kim, H. J., Ahn, J., Naito, M., Hayashi, K., Toh, K., Kim, B. S., Matsumura, Y., Kwon, I. C., & Miyata, K. (2018). Tuned density of anti-tissue factor antibody fragment onto siRNA-loaded polyion complex micelles for optimizing targetability into pancreatic cancer cells. Biomacromolecules, 19(6), 2320–2329.
Hazekawa, M., Nishinakagawa, T., Kawakubo-Yasukochi, T., & Nakashima, M. (2019). Glypican-3 gene silencing for ovarian cancer using siRNA-PLGA hybrid micelles in a murine peritoneal dissemination model. Journal of Pharmacological Sciences, 139(3), 231–239.
Lu, Y., Zhong, L., Jiang, Z., Pan, H., Zhang, Y., Zhu, G., Bai, L., Tong, R., Shi, J., & Duan, X. (2019). Cationic micelle-based siRNA delivery for efficient colon cancer gene therapy. Nanoscale Research Letters, 14(1), 1–9.
Cunningham, A. J., Gibson, V. P., Banquy, X., Zhu, X. X., & Jeanne, L. C. (2020). Cholic acid-based mixed micelles as siRNA delivery agents for gene therapy. International Journal of Pharmaceutics, 578, 119078.
Muddineti, O. S., Shah, A., Rompicharla, S. V. K., Ghosh, B., & Biswas, S. (2018). Cholesterol-grafted chitosan micelles as a nanocarrier system for drug-siRNA co-delivery to the lung cancer cells. International Journal of Biological Macromolecules, 118, 857–863.
Shi, L., Feng, H., Li, Z., Shi, J., Jin, L., & Li, J. (2021). Co-delivery of paclitaxel and siRNA with pH-responsive polymeric micelles for synergistic cancer therapy. Journal of Biomedical Nanotechnology, 17(2), 322–329.
Potluri, P., & Betageri, G. V. (2006). Mixed-micellar proliposomal systems for enhanced oral delivery of progesterone. Drug Delivery, 13(3), 227–232.
Gaucher, G., Satturwar, P., Jones, M.-C., Furtos, A., & Leroux, J.-C. (2010). Polymeric micelles for oral drug delivery. European Journal of Pharmaceutics and Biopharmaceutics, 76(2), 147–158. https://doi.org/10.1016/j.ejpb.2010.06.007
Han, X., Lu, Y., Xie, J., Zhang, E., Zhu, H., Du, H., Wang, K., Song, B., Yang, C., Shi, Y., & Cao, Z. (2020). Zwitterionic micelles efficiently deliver oral insulin without opening tight junctions. Nature Nanotechnology, 15(7), 605–614. https://doi.org/10.1038/s41565-020-0693-6
Ibaraki, H., Hatakeyama, N., Takeda, A., Arima, N., & Kanazawa, T. (2022). Multifunctional peptide carrier-modified polymer micelle accelerates oral siRNA-delivery to the colon and improves gene silencing-mediated therapeutic effects in ulcerative colitis. Journal of Drug Delivery Science and Technology, 73, 103481. https://doi.org/10.1016/j.jddst.2022.103481
Abbasi, E., Aval, S. F., Akbarzadeh, A., Milani, M., Nasrabadi, H. T., Joo, S. W., Hanifehpour, Y., Nejati-Koshki, K., & Pashaei-Asl, R. (2014). Dendrimers: Synthesis, applications, and properties. Nanoscale Research Letters, 9(1), 1–10.
Tambe, V., Thakkar, S., Raval, N., Sharma, D., Kalia, K., & Tekade, R. K. (2017). Surface engineered dendrimers in siRNA delivery and gene silencing. Current Pharmaceutical Design, 23(20), 2952–2975.
Michlewska, S., Ionov, M., Maroto-Díaz, M., Szwed, A., Ihnatsyeu-Kachan, A., Loznikova, S., Shcharbin, D., Maly, M., Ramirez, R. G., & de la Mata, F. J. (2018). Ruthenium dendrimers as carriers for anticancer siRNA. Journal of Inorganic Biochemistry, 181, 18–27.
Tarach, P., & Janaszewska, A. (2021). Recent advances in preclinical research using PAMAM dendrimers for cancer gene therapy. International Journal of Molecular Sciences, 22(6), 2912.
Abedi-Gaballu, F., Dehghan, G., Ghaffari, M., Yekta, R., Abbaspour-Ravasjani, S., Baradaran, B., Dolatabadi, J. E. N., & Hamblin, M. R. (2018). PAMAM dendrimers as efficient drug and gene delivery nanosystems for cancer therapy. Applied Materials Today, 12, 177–190.
Ghaffari, M., Dehghan, G., Baradaran, B., Zarebkohan, A., Mansoori, B., Soleymani, J., & Hamblin, M. R. (2020). Co-delivery of curcumin and Bcl-2 siRNA by PAMAM dendrimers for enhancement of the therapeutic efficacy in HeLa cancer cells. Colloids and Surfaces B: Biointerfaces, 188, 110762.
Ambrosio, L., Argenziano, M., Cucci, M. A., Grattarola, M., de Graaf, I. A. M., Dianzani, C., Barrera, G., Sánchez Nieves, J., Gomez, R., & Cavalli, R. (2020). Carbosilane dendrimers loaded with siRNA targeting Nrf2 as a tool to overcome cisplatin chemoresistance in bladder cancer cells. Antioxidants, 9(10), 993.
Taratula, O., Garbuzenko, O., Savla, R., Andrew Wang, Y., He, H., & Minko, T. (2011). Multifunctional nanomedicine platform for cancer specific delivery of siRNA by superparamagnetic iron oxide nanoparticles-dendrimer complexes. Current Drug Delivery, 8(1), 59–69.
Liu, X., Rocchi, P., Qu, F., Zheng, S., Liang, Z., Gleave, M., Iovanna, J., & Peng, L. (2009). PAMAM dendrimers mediate siRNA delivery to target Hsp27 and produce potent antiproliferative effects on prostate cancer cells. ChemMedChem, 4(8), 1302–1310.
Abedi Gaballu, F., Cho, W. C.-S., Dehghan, G., Zarebkohan, A., Baradaran, B., Mansoori, B., Abbaspour-Ravasjani, S., Mohammadi, A., Sheibani, N., & Aghanejad, A. (2021). Silencing of HMGA2 by siRNA loaded methotrexate functionalized polyamidoamine dendrimer for human breast cancer cell therapy. Genes, 12(7), 1102.
Yellepeddi, V. K., & Ghandehari, H. (2016). Poly (amido amine) dendrimers in oral delivery. Tissue Barriers, 4(2), e1173773.
Fernandes, G., Pandey, A., Kulkarni, S., Mutalik, S. P., Nikam, A. N., Seetharam, R. N., Kulkarni, S. S., & Mutalik, S. (2021). Supramolecular dendrimers based novel platforms for effective oral delivery of therapeutic moieties. Journal of Drug Delivery Science and Technology, 64, 102647. https://doi.org/10.1016/j.jddst.2021.102647
Gandhi, N. S., Godeshala, S., Koomoa-Lange, D.-L. T., Miryala, B., Rege, K., & Chougule, M. B. (2018). Bioreducible poly (amino ethers) based mTOR siRNA delivery for lung cancer. Pharmaceutical Research, 35(10), 1–20.
Hartl, N., Adams, F., Costabile, G., Isert, L., Döblinger, M., Xiao, X., Liu, R., & Merkel, O. M. (2019). The impact of Nylon-3 copolymer composition on the efficiency of siRNA delivery to glioblastoma Cells. Nanomaterials, 9(7), 986.
Karlsson, J., Tzeng, S. Y., Hemmati, S., Luly, K. M., Choi, O., Rui, Y., Wilson, D. R., Kozielski, K. L., Quiñones-Hinojosa, A., & Green, J. J. (2021). Photocrosslinked bioreducible polymeric nanoparticles for enhanced systemic siRNA delivery as cancer therapy. Advanced Functional Materials, 31(17), 2009768.
Yao, H., Sun, L., Li, J., Zhou, X., Li, R., Shao, R., Zhang, Y., & Li, L. (2020). A novel therapeutic siRNA nanoparticle designed for dual-targeting CD44 and Gli1 of gastric cancer stem cells. International Journal of Nanomedicine, 15, 7013.
Kozielski, K. L., Ruiz-Valls, A., Tzeng, S. Y., Guerrero-Cázares, H., Rui, Y., Li, Y., Vaughan, H. J., Gionet-Gonzales, M., Vantucci, C., & Kim, J. (2019). Cancer-selective nanoparticles for combinatorial siRNA delivery to primary human GBM in vitro and in vivo. Biomaterials, 209, 79–87.
Kourani, K., Jain, P., Kumar, A., Jangid, A. K., Swaminathan, G., Durgempudi, V. R., Jose, J., Reddy, R., Pooja, D., Kulhari, H., & Kumar, L. D. (2022). Inulin coated Mn3O4 nanocuboids coupled with RNA interference reverse intestinal tumorigenesis in Apc knockout murine colon cancer models. Nanomedicine: Nanotechnology, Biology and Medicine, 40, 102504. https://doi.org/10.1016/j.nano.2021.102504
Pędziwiatr-Werbicka, E., Gorzkiewicz, M., Michlewska, S., Ionov, M., Shcharbin, D., Klajnert-Maculewicz, B., Pena-Gonzalez, C. E., Sanchez-Nieves, J., Gomez, R., & de la Mata, F. J. (2021). Evaluation of dendronized gold nanoparticles as siRNAs carriers into cancer cells. Journal of Molecular Liquids, 324, 114726.
Yang, L., Kim, T., Cho, H., Luo, J., Lee, J., Chueng, S. D., Hou, Y., Yin, P. T., Han, J., & Kim, J. H. (2021). Hybrid graphene-gold nanoparticle-based nucleic acid conjugates for cancer-specific multimodal imaging and combined therapeutics. Advanced Functional Materials, 31(5), 2006918.
Yu, A. Y.-H., Fu, R.-H., Hsu, S., Chiu, C.-F., Fang, W.-H., Yeh, C.-A., Tang, C.-M., Hsieh, H.-H., & Hung, H.-S. (2021). Epidermal growth factor receptors siRNA-conjugated collagen modified gold nanoparticles for targeted imaging and therapy of lung cancer. Materials Today Advances, 12, 100191.
Cho, H.-J., Oh, J., Choo, M.-K., Ha, J.-I., Park, Y., & Maeng, H.-J. (2014). Chondroitin sulfate-capped gold nanoparticles for the oral delivery of insulin. International Journal of Biological Macromolecules, 63, 15–20.
Kumari, Y., Singh, S. K., Kumar, R., Kumar, B., Kaur, G., Gulati, M., Tewari, D., Gowthamarajan, K., Karri, V. V. S. N. R., & Ayinkamiye, C. (2020). Modified apple polysaccharide capped gold nanoparticles for oral delivery of insulin. International Journal of Biological Macromolecules, 149, 976–988.
Cheng, F.-F., Chen, W., Hu, L.-H., Chen, G., Miao, H.-T., Li, C., & Zhu, J.-J. (2013). Highly dispersible PEGylated graphene/Au composites as gene delivery vector and potential cancer therapeutic agent. Journal of Materials Chemistry B, 1(38), 4956–4962.
Wang, Q., Zhang, C., Shen, G., Liu, H., Fu, H., & Cui, D. (2014). Fluorescent carbon dots as an efficient siRNA nanocarrier for its interference therapy in gastric cancer cells. Journal of Nanobiotechnology. https://doi.org/10.1186/s12951-014-0058-0
Sengupta, A., Mezencev, R., McDonald, J. F., & Prausnitz, M. R. (2015). Delivery of siRNA to ovarian cancer cells using laser-activated carbon nanoparticles. Nanomedicine, 10(11), 1775–1784.
Yin, F., Hu, K., Chen, Y., Yu, M., Wang, D., Wang, Q., Yong, K.-T., Lu, F., Liang, Y., & Li, Z. (2017). SiRNA delivery with PEGylated graphene oxide nanosheets for combined photothermal and genetherapy for pancreatic cancer. Theranostics, 7(5), 1133.
Bae, K. H., Lee, K., Kim, C., & Park, T. G. (2011). Surface functionalized hollow manganese oxide nanoparticles for cancer targeted siRNA delivery and magnetic resonance imaging. Biomaterials, 32(1), 176–184.
Rea, I., Martucci, N. M., De Stefano, L., Ruggiero, I., Terracciano, M., Dardano, P., Migliaccio, N., Arcari, P., Taté, R., & Rendina, I. (2014). Diatomite biosilica nanocarriers for siRNA transport inside cancer cells. Biochimica et Biophysica Acta (BBA)-General Subjects, 1840(12), 3393–3403.
Cristofolini, T., Dalmina, M., Sierra, J. A., Silva, A. H., Pasa, A. A., Pittella, F., & Creczynski-Pasa, T. B. (2020). Multifunctional hybrid nanoparticles as magnetic delivery systems for siRNA targeting the HER2 gene in breast cancer cells. Materials Science and Engineering: C, 109, 110555.
Mohammed, M. R. S., Ahmad, V., Ahmad, A., Tabrez, S., Choudhry, H., Zamzami, M. A., Bakhrebah, M. A., Ahmad, A., Wasi, S., & Mukhtar, H. (2021). Prospective of nanoscale metal organic frameworks [NMOFs] for cancer therapy. In Seminars in cancer biology (Vol. 69, pp. 129–139). Elsevier.
Jin, L., Wang, Q., Chen, J., Wang, Z., Xin, H., & Zhang, D. (2019). Efficient delivery of therapeutic siRNA by Fe3O4 magnetic nanoparticles into oral cancer cells. Pharmaceutics, 11(11), 615. https://doi.org/10.3390/pharmaceutics11110615
Keskin, D., Zu, G., Forson, A. M., Tromp, L., Sjollema, J., & van Rijn, P. (2021). Nanogels: A novel approach in antimicrobial delivery systems and antimicrobial coatings. Bioactive Materials, 6(10), 3634–3657.
Spencer, D. S., Shodeinde, A. B., Beckman, D. W., Luu, B. C., Hodges, H. R., & Peppas, N. A. (2021). Cytocompatibility, membrane disruption, and siRNA delivery using environmentally responsive cationic nanogels. Journal of Controlled Release, 332, 608–619.
Fujii, H., Shin-Ya, M., Takeda, S., Hashimoto, Y., Mukai, S., Sawada, S., Adachi, T., Akiyoshi, K., Miki, T., & Mazda, O. (2014). Cycloamylose-nanogel drug delivery system-mediated intratumor silencing of the vascular endothelial growth factor regulates neovascularization in tumor microenvironment. Cancer Science, 105(12), 1616–1625.
Yavvari, P. S., Verma, P., Mustfa, S. A., Pal, S., Kumar, S., Awasthi, A. K., Ahuja, V., Srikanth, C. V., Srivastava, A., & Bajaj, A. (2019). A nanogel based oral gene delivery system targeting SUMOylation machinery to combat gut inflammation. Nanoscale, 11(11), 4970–4986. https://doi.org/10.1039/C8NR09599J
Knipe, J. M., Strong, L. E., & Peppas, N. A. (2016). Enzyme- and pH-responsive microencapsulated nanogels for oral delivery of siRNA to induce TNF-α knockdown in the intestine. Biomacromolecules, 17(3), 788–797. https://doi.org/10.1021/acs.biomac.5b01518
Valizadeh, A., & Mussa Farkhani, S. (2014). Electrospinning and electrospun nanofibres. IET Nanobiotechnology, 8(2), 83–92.
Lim, C. T. (2017). Nanofiber technology: Current status and emerging developments. Progress in Polymer Science, 70, 1–17.
Hu, X., Liu, S., Zhou, G., Huang, Y., Xie, Z., & Jing, X. (2014). Electrospinning of polymeric nanofibers for drug delivery applications. Journal of Controlled Release, 185, 12–21.
Chen, S., Boda, S. K., Batra, S. K., Li, X., & Xie, J. (2018). Emerging roles of electrospun nanofibers in cancer research. Advanced Healthcare Materials, 7(6), 1701024.
Stojanov, S., & Berlec, A. (2020). Electrospun nanofibers as carriers of microorganisms, stem cells, proteins, and nucleic acids in therapeutic and other applications. Frontiers in Bioengineering and Biotechnology, 8, 130.
Rujitanaroj, P., Jao, B., Yang, J., Wang, F., Anderson, J. M., Wang, J., & Chew, S. Y. (2013). Controlling fibrous capsule formation through long-term down-regulation of collagen type I (COL1A1) expression by nanofiber-mediated siRNA gene silencing. Acta Biomaterialia, 9(1), 4513–4524.
Pinese, C., Lin, J., Milbreta, U., Li, M., Wang, Y., Leong, K. W., & Chew, S. Y. (2018). Sustained delivery of siRNA/mesoporous silica nanoparticle complexes from nanofiber scaffolds for long-term gene silencing. Acta Biomaterialia, 76, 164–177.
Ashrafizadeh, M., Delfi, M., Hashemi, F., Zabolian, A., Saleki, H., Bagherian, M., Azami, N., Farahani, M. V., Sharifzadeh, S. O., & Hamzehlou, S. (2021). Biomedical application of chitosan-based nanoscale delivery systems: Potential usefulness in siRNA delivery for cancer therapy. Carbohydrate Polymers, 260, 117809.
Yang, J., Dai, J., Wang, Q., Cheng, Y., Guo, J., Zhao, Z., Hong, Y., Lou, X., & Xia, F. (2020). Tumor-triggered disassembly of a multiple-agent-therapy probe for efficient cellular internalization. Angewandte Chemie, 132(46), 20585–20590.
Serrano-Sevilla, I., Artiga, Á., Mitchell, S. G., De Matteis, L., & de la Fuente, J. M. (2019). Natural polysaccharides for siRNA delivery: Nanocarriers based on chitosan, hyaluronic acid, and their derivatives. Molecules, 24(14), 2570.
Choi, J. S., Han, S.-H., Hyun, C., & Yoo, H. S. (2016). Buccal adhesive nanofibers containing human growth hormone for oral mucositis. Journal of Biomedical Materials Research Part B: Applied Biomaterials, 104(7), 1396–1406. https://doi.org/10.1002/jbm.b.33487
Snook, J. D., Chesson, C. B., Peniche, A. G., Dann, S. M., Paulucci, A., Pinchuk, I. V., & Rudra, J. S. (2016). Peptide nanofiber–CaCO 3 composite microparticles as adjuvant-free oral vaccine delivery vehicles. Journal of Materials Chemistry B, 4(9), 1640–1649. https://doi.org/10.1039/C5TB01623A
Mousazadeh, H., Pilehvar-Soltanahmadi, Y., Dadashpour, M., & Zarghami, N. (2021). Cyclodextrin based natural nanostructured carbohydrate polymers as effective non-viral siRNA delivery systems for cancer gene therapy. Journal of Controlled Release, 330, 1046–1070.
Ganesh, S., Iyer, A. K., Weiler, J., Morrissey, D. V., & Amiji, M. M. (2013). Combination of siRNA-directed gene silencing with cisplatin reverses drug resistance in human non-small cell lung cancer. Molecular Therapy-Nucleic Acids, 2, e110.
Eivazy, P., Atyabi, F., Jadidi-Niaragh, F., Aghebati Maleki, L., Miahipour, A., Abdolalizadeh, J., & Yousefi, M. (2017). The impact of the codelivery of drug-siRNA by trimethyl chitosan nanoparticles on the efficacy of chemotherapy for metastatic breast cancer cell line (MDA-MB-231). Artificial Cells, Nanomedicine, and Biotechnology, 45(5), 889–896.
Liang, Y., Wang, Y., Wang, L., Liang, Z., Li, D., Xu, X., Chen, Y., Yang, X., Zhang, H., & Niu, H. (2021). Self-crosslinkable chitosan-hyaluronic acid dialdehyde nanoparticles for CD44-targeted siRNA delivery to treat bladder cancer. Bioactive Materials, 6(2), 433–446.
Kang, S. H., Revuri, V., Lee, S. J., Cho, S., Park, I. K., Cho, K. J., Bae, W. K., & Lee, Y. K. (2017). Oral siRNA delivery to treat colorectal liver metastases. ACS Nano. https://doi.org/10.1021/acsnano.7b05547
Han, L., Tang, C., & Yin, C. (2014). Oral delivery of shRNA and siRNA via multifunctional polymeric nanoparticles for synergistic cancer therapy. Biomaterials, 35(15), 4589–4600. https://doi.org/10.1016/j.biomaterials.2014.02.027
Li, P.-P., Yan, Y., Zhang, H.-T., Cui, S., Wang, C.-H., Wei, W., Qian, H.-G., Wang, J.-C., & Zhang, Q. (2020). Biological activities of siRNA-loaded lanthanum phosphate nanoparticles on colorectal cancer. Journal of Controlled Release, 328, 45–58. https://doi.org/10.1016/j.jconrel.2020.08.027
Janardhanam, L. S. L., Bandi, S. P., & Venuganti, V. V. K. (2022). Functionalized LbL film for localized delivery of STAT3 siRNA and oxaliplatin combination to treat colon cancer. ACS Applied Materials & Interfaces, 14(8), 10030–10046. https://doi.org/10.1021/acsami.1c22166
Wei, W., Lv, P.-P., Chen, X.-M., Yue, Z.-G., Fu, Q., Liu, S.-Y., Yue, H., & Ma, G.-H. (2013). Codelivery of mTERT siRNA and paclitaxel by chitosan-based nanoparticles promoted synergistic tumor suppression. Biomaterials, 34(15), 3912–3923. https://doi.org/10.1016/j.biomaterials.2013.02.030
Shi, X.-L., Li, Y., Zhao, L.-M., Su, L.-W., & Ding, G. (2019). Delivery of MTH1 inhibitor (TH287) and MDR1 siRNA via hyaluronic acid-based mesoporous silica nanoparticles for oral cancers treatment. Colloids and Surfaces B: Biointerfaces, 173, 599–606. https://doi.org/10.1016/j.colsurfb.2018.09.076
Hyun, E.-J., Hasan, M. N., Kang, S. H., Cho, S., & Lee, Y.-K. (2019). Oral siRNA delivery using dual transporting systems to efficiently treat colorectal liver metastasis. International Journal of Pharmaceutics, 555, 250–258. https://doi.org/10.1016/j.ijpharm.2018.11.009
Zhang, L., Peng, H., Zhang, W., Li, Y., Liu, L., & Leng, T. (2020). Yeast cell wall particle mediated nanotube-RNA delivery system loaded with miR365 antagomir for post-traumatic osteoarthritis therapy via oral route. Theranostics, 10(19), 8479–8493. https://doi.org/10.7150/thno.46761
Zheng, H., Tang, C., & Yin, C. (2015). Oral delivery of shRNA based on amino acid modified chitosan for improved antitumor efficacy. Biomaterials, 70, 126–137. https://doi.org/10.1016/j.biomaterials.2015.08.024
Xiang, S., Fruehauf, J., & Li, C. J. (2006). Short hairpin RNA–Expressing bacteria elicit RNA interference in mammals. Nature Biotechnology, 24(6), 697–702. https://doi.org/10.1038/nbt1211
Boddupalli, B. M., Mohammed, Z. N. K., Nath, R. A., & Banji, D. (2010). Mucoadhesive drug delivery system: An overview. Journal of Advanced Pharmaceutical Technology & Research, 1(4), 381–387. https://doi.org/10.4103/0110-5558.76436
Ahuja, A., Khar, R. K., & Ali, J. (1997). Mucoadhesive drug delivery systems. Drug Development and Industrial Pharmacy, 23(5), 489–515.
Veuillez, F., Kalia, Y. N., Jacques, Y., Deshusses, J., & Buri, P. (2001). Factors and strategies for improving buccal absorption of peptides. European journal of Pharmaceutics and Biopharmaceutics, 51(2), 93–109.
Longer, M. A., & Robinson, J. R. (1986). Fundamental-aspects of bioadhesion. Pharmacy International, 7(5), 114–117.
Gu, J. M., Robinson, J. R., & Leung, S. H. (1988). Binding of acrylic polymers to mucin/epithelial surfaces: Structure-property relationships. Critical Reviews in Therapeutic Drug Carrier Systems, 5(1), 21–67.
Kinloch, A. J. (1980). The science of adhesion. Journal of Materials Science, 15(9), 2141–2166.
Huntsberger, J. R. (1967). Mechanisms of adhesion. Journal Paint Technology, 39(507), 199–211.
Wake, W. C. (1976). Adhesion and the formulation of adhesives. Applied Science Publishers.
Kumar, R., Islam, T., & Nurunnabi, M. (2022). Mucoadhesive carriers for oral drug delivery. Journal of Controlled Release, 351, 504–559. https://doi.org/10.1016/j.jconrel.2022.09.024
Yang, X., & Robinson, J. (1998). Bioadhesion in mucosal drug delivery. Academic Press.
Hombach, J., & Bernkop-Schnürch, A. (2010). Mucoadhesive drug delivery systems. In M. Schäfer-Korting (Ed.), Drug delivery (pp. 251–266). Springer. https://doi.org/10.1007/978-3-642-00477-3_9
Nurunnabi, M., Afrin, H., Huda, M. N., & Salazar, C. J. J. (2023). Oral delivery compositions for obesity management. US Patent App. 17/871,953. U.S. Patent and Trademark. https://ppubs.uspto.gov/pubwebapp/static/pages/ppubsbasic.html
Mao, S., Sun, W., & Kissel, T. (2010). Chitosan-based formulations for delivery of DNA and siRNA. Advanced Drug Delivery Reviews, 62(1), 12–27.
Ilium, L. (1998). Chitosan and its use as a pharmaceutical excipient. Pharmaceutical Research, 15(9), 1326–1331.
Martirosyan, A., Olesen, M. J., & Howard, K. A. (2014). Chapter Eleven - Chitosan-based nanoparticles for mucosal delivery of RNAi therapeutics. In L. Huang, D. Liu, & E. Wagner (Eds.), Nonviral vectors for gene therapy (Vol. 88, pp. 325–352). Academic Press. https://doi.org/10.1016/B978-0-12-800148-6.00011-0
Ways, M., Lau, W. M., & Khutoryanskiy, V. (2018). Chitosan and its derivatives for application in mucoadhesive drug delivery systems. Polymers, 10(3), 267. https://doi.org/10.3390/polym10030267
Hejazi, R., & Amiji, M. (2003). Chitosan-based gastrointestinal delivery systems. Journal of Controlled Release, 89(2), 151–165. https://doi.org/10.1016/S0168-3659(03)00126-3
Khutoryanskiy, V. V. (2011). Advances in mucoadhesion and mucoadhesive polymers. Macromolecular bioscience, 11(6), 748–764. https://doi.org/10.1002/mabi.201000388
Shu, X. Z., & Zhu, K. J. (2002). The influence of multivalent phosphate structure on the properties of ionically cross-linked chitosan films for controlled drug release. European Journal of Pharmaceutics and Biopharmaceutics, 54(2), 235–243.
Ballarín-González, B., & Howard, K. A. (2012). Polycation-based nanoparticle delivery of RNAi therapeutics: Adverse effects and solutions. Advanced Drug Delivery Reviews, 64(15), 1717–1729. https://doi.org/10.1016/j.addr.2012.07.004
Katas, H., & Alpar, H. O. (2006). Development and characterisation of chitosan nanoparticles for siRNA delivery. Journal of Controlled Release, 115(2), 216–225.
Liu, X., Howard, K. A., Dong, M., Andersen, M. Ø., Rahbek, U. L., Johnsen, M. G., Hansen, O. C., Besenbacher, F., & Kjems, J. (2007). The influence of polymeric properties on chitosan/siRNA nanoparticle formulation and gene silencing. Biomaterials, 28(6), 1280–1288.
Zhang, J., He, C., Tang, C., & Yin, C. (2013). Ternary polymeric nanoparticles for oral siRNA delivery. Pharmaceutical Research, 30(5), 1228–1239. https://doi.org/10.1007/s11095-012-0961-8
Roșu, M. C., Mihnea, P. D., Ardelean, A., Moldovan, S. D., Popețiu, R. O., & Totolici, B. D. (2022). Clinical significance of tumor necrosis factor-alpha and carcinoembryonic antigen in gastric cancer. Journal of Medicine and Life, 15(1), 4–6.
Suganuma, M., Watanabe, T., Yamaguchi, K., Takahashi, A., & Fujiki, H. (2012). Human gastric cancer development with TNF-α-inducing protein secreted from Helicobacter pylori. Cancer letters, 322(2), 133–138. https://doi.org/10.1016/j.canlet.2012.03.027
Yu, L., Xiong, J., Guo, L., Miao, L., Liu, S., & Guo, F. (2015). The effects of lanthanum chloride on proliferation and apoptosis of cervical cancer cells: Involvement of let-7a and miR-34a microRNAs. BioMetals, 28(5), 879–890.
Su, X., Zheng, X., & Ni, J. (2009). Lanthanum citrate induces anoikis of Hela cells. Cancer Letters, 285(2), 200–209.
He, C., Yin, L., Song, Y., Tang, C., & Yin, C. (2015). Optimization of multifunctional chitosan–siRNA nanoparticles for oral delivery applications, targeting TNF-α silencing in rats. Acta Biomaterialia, 17, 98–106.
Chen, W. Y., & Abatangelo, G. (1999). Functions of hyaluronan in wound repair. Wound Repair and Regeneration: The International Journal of Tissue Repair and Regeneration, 7(2), 79–89. https://doi.org/10.1046/j.1524-475x.1999.00079.x
Fraser, J. R., Laurent, T. C., & Laurent, U. B. (1997). Hyaluronan: Its nature, distribution, functions and turnover. Journal Of Internal Medicine, 242(1), 27–33. https://doi.org/10.1046/j.1365-2796.1997.00170.x
Allison, D. D., & Grande-Allen, K. J. (2006). Review. Hyaluronan: A powerful tissue engineering tool. Tissue Engineering, 12(8), 2131–2140. https://doi.org/10.1089/ten.2006.12.2131
Griesser, J., Hetényi, G., & Bernkop-Schnürch, A. (2018). Thiolated hyaluronic acid as versatile mucoadhesive polymer: From the chemistry behind to product developments—What are the capabilities? Polymers, 10(3), 243. https://doi.org/10.3390/polym10030243
Yang, J., Zhao, R., Feng, Q., Zhuo, X., & Wang, R. (2021). Development of a carrier system containing hyaluronic acid and protamine for siRNA delivery in the treatment of melanoma. Investigational New Drugs, 39(1), 66–76. https://doi.org/10.1007/s10637-020-00986-3
Shahin, S. A., Wang, R., Simargi, S. I., Contreras, A., Parra Echavarria, L., Qu, L., Wen, W., Dellinger, T., Unternaehrer, J., Tamanoi, F., Zink, J. I., & Glackin, C. A. (2018). Hyaluronic acid conjugated nanoparticle delivery of siRNA against TWIST reduces tumor burden and enhances sensitivity to cisplatin in ovarian cancer. Nanomedicine: Nanotechnology, Biology and Medicine, 14(4), 1381–1394. https://doi.org/10.1016/j.nano.2018.04.008
Bastaki, S., Aravindhan, S., Ahmadpour Saheb, N., Afsari Kashani, M., Evgenievich Dorofeev, A., Karoon Kiani, F., Jahandideh, H., Beigi Dargani, F., Aksoun, M., Nikkhoo, A., Masjedi, A., Mahmoodpoor, A., Ahmadi, M., Dolati, S., Namvar Aghdash, S., & Jadidi-Niaragh, F. (2021). Codelivery of STAT3 and PD-L1 siRNA by hyaluronate-TAT trimethyl/thiolated chitosan nanoparticles suppresses cancer progression in tumor-bearing mice. Life Sciences, 266, 118847. https://doi.org/10.1016/j.lfs.2020.118847
Lage, H. (2014). Chapter 5 - Bacterial delivery of RNAi effectors. In E. C. Lattime & S. L. Gerson (Eds.), Gene therapy of cancer (3rd ed., pp. 67–75). Academic Press. https://doi.org/10.1016/B978-0-12-394295-1.00005-6
D’Cruz, O., Hwang, L., Fong, A., Ng, K., Nam, D., Wang, W., & Trieu, V. (2017). Preclinical and clinical studies on safety of CEQ508 bacteria engineered to deliver short-hairpin RNA to mediate RNA interference against β-catenin in the GI tract of patients with familial adenomatous polyposis: 297. Official Journal of the American College of Gastroenterology| ACG, 112, S162–S163.
Trieu, V., Hwang, L., Ng, K., D’Cruz, O., Qazi, S., & Fong, A. (2017). First-in-human Phase I study of bacterial RNA interference therapeutic CEQ508 in patients with familial adenomatous polyposis (FAP). Annals of Oncology, 28, v174.
Zhang, L., Zhang, T., Wang, L., Shao, S., Chen, Z., & Zhang, Z. (2014). In vivo targeted delivery of CD40 shRNA to mouse intestinal dendritic cells by oral administration of recombinant Sacchromyces cerevisiae. Gene Therapy, 21(7), 709–714.
Zhang, L., Zhang, W., Peng, H., Li, Y., Leng, T., Xie, C., & Zhang, L. (2021). Oral gene therapy of HFD-obesity via nonpathogenic yeast microcapsules mediated shRNA delivery. Pharmaceutics, 13(10), 1536.
Zhang, L., Peng, H., Feng, M., Zhang, W., & Li, Y. (2021). Yeast microcapsule-mediated oral delivery of IL-1β shRNA for post-traumatic osteoarthritis therapy. Molecular Therapy-Nucleic Acids, 23, 336–346.
Islam, T., Huda, M. N., Ahsan, M. A., Afrin, H., Salazar, C. J., & Nurunnabi, M. (2021). Theoretical and experimental insights into the possible interfacial interactions between β-glucan and fat molecules in aqueous media. The Journal of Physical Chemistry B, 125(50), 13730–13743. https://doi.org/10.1021/acs.jpcb.1c08065
Jeong, J. H., Mok, H., Oh, Y.-K., & Park, T. G. (2009). siRNA conjugate delivery systems. Bioconjugate Chemistry, 20(1), 5–14. https://doi.org/10.1021/bc800278e
Paredes, E., Evans, M., & Das, S. R. (2011). RNA labeling, conjugation and ligation. Methods, 54(2), 251–259. https://doi.org/10.1016/j.ymeth.2011.02.008
Lee, S. H., Kang, Y. Y., Jang, H.-E., & Mok, H. (2016). Current preclinical small interfering RNA (siRNA)-based conjugate systems for RNA therapeutics. Advanced Drug Delivery Reviews, 104, 78–92. https://doi.org/10.1016/j.addr.2015.10.009
Springer, A. D., & Dowdy, S. F. (2018). GalNAc-siRNA conjugates: Leading the way for delivery of RNAi therapeutics. Nucleic Acid Therapeutics, 28(3), 109–118. https://doi.org/10.1089/nat.2018.0736
Yarian, F., Alibakhshi, A., Eyvazi, S., Arezumand, R., & Ahangarzadeh, S. (2019). Antibody-drug therapeutic conjugates: Potential of antibody-siRNAs in cancer therapy. Journal of Cellular Physiology, 234(10), 16724–16738. https://doi.org/10.1002/jcp.28490
Cuellar, T. L., Barnes, D., Nelson, C., Tanguay, J., Yu, S.-F., Wen, X., Scales, S. J., Gesch, J., Davis, D., van Brabant Smith, A., Leake, D., Vandlen, R., & Siebel, C. W. (2015). Systematic evaluation of antibody-mediated siRNA delivery using an industrial platform of THIOMAB–siRNA conjugates. Nucleic Acids Research, 43(2), 1189–1203. https://doi.org/10.1093/nar/gku1362
Eloy, J. O., Petrilli, R., Trevizan, L. N. F., & Chorilli, M. (2017). Immunoliposomes: A review on functionalization strategies and targets for drug delivery. Colloids and Surfaces B: Biointerfaces, 159, 454–467. https://doi.org/10.1016/j.colsurfb.2017.07.085
Zhou, J., & Rossi, J. J. (2012). Therapeutic potential of aptamer-siRNA conjugates for treatment of HIV-1. BioDrugs, 26(6), 393–400. https://doi.org/10.1007/BF03261896
Liao, L., Cen, B., Li, G., Wei, Y., Wang, Z., Huang, W., He, S., Yuan, Y., & Ji, A. (2021). A bivalent cyclic RGD–siRNA conjugate enhances the antitumor effect of apatinib via co-inhibiting VEGFR2 in non-small cell lung cancer xenografts. Drug Delivery, 28(1), 1432–1442. https://doi.org/10.1080/10717544.2021.1937381
Kim, H. A., Nam, K., & Kim, S. W. (2014). Tumor targeting RGD conjugated bio-reducible polymer for VEGF siRNA expressing plasmid delivery. Biomaterials, 35(26), 7543–7552. https://doi.org/10.1016/j.biomaterials.2014.05.021
Yao, Y., Sun, T., Huang, S., Dou, S., Lin, L., Chen, J., Ruan, J., Mao, C., Yu, F., Zeng, M., Zang, J., Liu, Q., Su, F., Zhang, P., Lieberman, J., Wang, J., & Song, E. (2012). Targeted delivery of PLK1-siRNA by ScFv suppresses Her2 + breast cancer growth and metastasis. Science Translational Medicine, 4(130). https://doi.org/10.1126/scitranslmed.3003601
Xu, W.-W., Liu, D., Cao, Y., & Wang, X. (2017). GE11 peptide-conjugated nanoliposomes to enhance the combinational therapeutic efficacy of docetaxel and siRNA in laryngeal cancers. International Journal of Nanomedicine, 12, 6461–6470. https://doi.org/10.2147/IJN.S129946
Gangopadhyay, S., Nikam, R. R., & Gore, K. R. (2021). Folate receptor-mediated siRNA delivery: Recent developments and future directions for RNAi therapeutics. Nucleic Acid Therapeutics, 31(4), 245–270. https://doi.org/10.1089/nat.2020.0882
Shim, M. S., & Kwon, Y. J. (2010). Efficient and targeted delivery of siRNA in vivo. FEBS Journal, 277(23), 4814–4827. https://doi.org/10.1111/j.1742-4658.2010.07904.x
DiFiglia, M., Sena-Esteves, M., Chase, K., Sapp, E., Pfister, E., Sass, M., Yoder, J., Reeves, P., Pandey, R. K., Rajeev, K. G., Manoharan, M., Sah, D. W. Y., Zamore, P. D., & Aronin, N. (2007). Therapeutic silencing of mutant huntingtin with siRNA attenuates striatal and cortical neuropathology and behavioral deficits. Proceedings of the National Academy of Sciences, 104(43), 17204–17209. https://doi.org/10.1073/pnas.0708285104
Dey, A. K., Griffiths, C., Lea, S. M., & James, W. (2005). Structural characterization of an anti-gp120 RNA aptamer that neutralizes R5 strains of HIV-1. RNA, 11(6), 873–884. https://doi.org/10.1261/rna.7205405
Lee, J. W., Choi, J., Choi, Y., Kim, K., Yang, Y., Kim, S. H., Yoon, H. Y., & Kwon, I. C. (2022). Molecularly engineered siRNA conjugates for tumor-targeted RNAi therapy. Journal of Controlled Release, 351, 713–726. https://doi.org/10.1016/j.jconrel.2022.09.040
Research and Markets. (2022, April 21). Global RNAi therapeutics market insights & forecast report 2022–2026: Rising utilization in oncology pharmaceuticals & progress in collaborations and associated deals in RNAi therapeutics. GlobeNewswire News Room. Retrieved September 28, 2022, from https://www.globenewswire.com/en/news-release/2022/04/21/2426143/28124/en/Global-RNAi-Therapeutics-Market-Insights-Forecast-Report-2022-2026-Rising-Utilization-in-Oncology-Pharmaceuticals-Progress-in-Collaborations-and-Associated-Deals-in-RNAi-Therapeuti.html
Sebastian, V. (2022). Toward continuous production of high-quality nanomaterials using microfluidics: Nanoengineering the shape, structure and chemical composition. Nanoscale, 14(12), 4411–4447. https://doi.org/10.1039/D1NR06342A
Chabattula, S. C., Gupta, P. K., Tripathi, S. K., Gahtori, R., Padhi, P., Mahapatra, S., Biswal, B. K., Singh, S. K., Dua, K., Ruokolainen, J., Mishra, Y. K., Jha, N. K., Bishi, D. K., & Kesari, K. K. (2021). Anticancer therapeutic efficacy of biogenic Am-ZnO nanoparticles on 2D and 3D tumor models. Materials Today Chemistry, 22, 100618. https://doi.org/10.1016/j.mtchem.2021.100618
Panda, S., Hajra, S., Kaushik, A., Rubahn, H. G., Mishra, Y. K., & Kim, H. J. (2022). A focused review on three-dimensional bioprinting technology for artificial organ fabrication. Biomaterials Science, 10(18), 5054–5080. https://doi.org/10.1039/D2BM00797E
Hassanzadeh, P., Atyabi, F., & Dinarvand, R. (2019). The significance of artificial intelligence in drug delivery system design. Advanced Drug Delivery Reviews, 151–152, 169–190. https://doi.org/10.1016/j.addr.2019.05.001
Gong, D., Ben-Akiva, E., Singh, A., Yamagata, H., Est-Witte, S., Shade, J. K., Trayanova, N. A., & Green, J. J. (2022). Machine learning guided structure function predictions enable in silico nanoparticle screening for polymeric gene delivery. Acta Biomaterialia, 154, 349–358.
Kearney, E., Wojcik, A., & Babu, D. (2020). Artificial intelligence in genetic services delivery: Utopia or apocalypse? Journal of Genetic Counseling, 29(1), 8–17.
Moore, J. A., & Chow, J. C. L. (2021). Recent progress and applications of gold nanotechnology in medical biophysics using artificial intelligence and mathematical modeling. Nano Express, 2(2), 22001.
Panda, S., Hajra, S., Kaushik, A., Rubahn, H. G., Mishra, Y. K., & Kim, H. J. (2022). Smart nanomaterials as the foundation of a combination approach for efficient cancer theranostics. Materials Today Chemistry, 26, 101182. https://doi.org/10.1016/j.mtchem.2022.101182
Acknowledgements
The authors are grateful to the BioRender and http://smart.servier.com/ to draw the schemes.
Funding
We acknowledge the funding by the Cancer Prevention Research Institute of Texas (CPRIT) through the Texas Regional Excellence in Cancer Award (TREC) under Award No. PR210153, and National Institutes of Health (NIH) under Award No R03OD032624. The contents of this paper are solely the authors’ responsibility and do not necessarily represent the official views of NIH.
Author information
Authors and Affiliations
Contributions
Humayra Afrin, Renu Geetha Bai, and Md Nurunnabi made the outline. Humayra Afrin, Renu Geetha Bai, Raj Kumar, and Shaikh Shafin Ahmed contributed to writing. Humayra Afrin, Shaikh Shafin Ahmed, and Renu Geetha Bai made the drawing and graphics. Md Nurunnabi and Sandeep Agarwal contributed on editing and revising. All authors contributed to the writing, reviewing, and editing of the manuscript.
Corresponding author
Ethics declarations
Ethical approval
N/A
Informed consent
N/A
Conflict of interest
The authors declare no competing interests.
Additional information
Publisher's note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Rights and permissions
Springer Nature or its licensor (e.g. a society or other partner) holds exclusive rights to this article under a publishing agreement with the author(s) or other rightsholder(s); author self-archiving of the accepted manuscript version of this article is solely governed by the terms of such publishing agreement and applicable law.
About this article
Cite this article
Afrin, H., Geetha Bai, R., Kumar, R. et al. Oral delivery of RNAi for cancer therapy. Cancer Metastasis Rev 42, 699–724 (2023). https://doi.org/10.1007/s10555-023-10099-x
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s10555-023-10099-x