Abstract
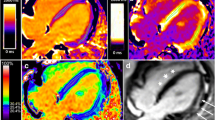
Duchenne muscular dystrophy (DMD) is an X-linked genetic disorder leading to progressive skeletal and cardiac myopathy. Elevated myocardial T1 values correlate with fibrosis in most disease processes, but DMD skeletal and cardiac histopathology is defined by fibrofatty replacement that may result in a decrease in T1 values, due to the low T1 of fat. The study goal was to assess myocardial T1 values in DMD patients with and without late gadolinium enhancement (LGE). A retrospective analysis was performed on all patients with DMD referred for CMR at our institution from 7/5/2017 to 10/24/2018. T1 measurements were performed using breath-held modified Look Locker inversion recovery (MOLLI) sequences at the basal and mid-ventricular levels. The cohort was separated into patients without the presence of LGE (LGE−) and patients with current or previous LGE (LGE+). A total of 207 CMR studies were analyzed. The LGE− group comprised 88 patients while 119 patients were in the LGE+ group. The LGE+ group was older, had larger indexed LV end-diastolic volume and lower LV ejection fraction (LVEF) compared to the LGE− group. T1 values in the LGE+ group were lower compared to the LGE− group (mid T1 1012 ms vs. 1035 ms; p = 0.002), with 5 CMR studies demonstrating mid T1 values < 900 ms. There was no correlation between mid T1 and LVEF in the LGE− group. In the LGE+ cohort, lower T1 values correlated with worse LVEF (r = 0.34, p = 0.0002). The association between mid T1 values and LVEF remained statistically significant on multivariable analysis when accounting for number of LGE segments, LVEDVi, and age (p = 0.009). This is the largest study assessing native T1 values in patients with DMD. The results demonstrate that patients with LGE had lower T1 values than patients without LGE. In the LGE+ group, lower T1 values correlated with worse LV systolic function. These results are consistent with the evolving recognition of fibrofatty replacement in advanced stages of DMD myopathy. Furthermore, our study supports that there is not a simple linear relationship between increasing T1 values and advancing disease progression reported in most other cardiomyopathies.



Similar content being viewed by others

Data availability
The data that support the findings of this study are available on request from the corresponding author [SML]. The data are not publicly available due to records which may contain information that could compromise patient confidentiality.
References
Muntoni F, Torelli S, Ferlini A (2003) Dystrophin and mutations: one gene, several proteins, multiple phenotypes. Lancet Neurol 2:731–740
Centers for Disease Control and Prevention (2009) Prevalence of Duchenne/Becker muscular dystrophy among males aged 5–24 years—four states, 2007. MMWR Morb Mortal Wkly Rep 58:1119–1122
Eagle M, Baudouin SV, Chandler C, Giddings DR, Bullock R, Bushby K (2002) Survival in Duchenne muscular dystrophy: improvements in life expectancy since 1967 and the impact of home nocturnal ventilation. Neuromuscul Disord 12:926–929
Connuck DM, Sleeper LA, Colan SD, Cox GF, Towbin JA, Lowe AM et al (2008) Characteristics and outcomes of cardiomyopathy in children with Duchenne or Becker muscular dystrophy: a comparative study from the Pediatric Cardiomyopathy Registry. Am Heart J 155:998–1005
Power A, Poonja S, Disler D, Myers K, Patton DJ, Mah JK et al (2017) Echocardiographic image quality deteriorates with age in children and young adults with Duchenne muscular dystrophy. Front Cardiovasc Med 4:82
Soslow JH, Xu M, Slaughter JC, Stanley M, Crum K, Markham LW et al (2016) Evaluation of echocardiographic measures of left ventricular function in patients with Duchenne muscular dystrophy: assessment of reproducibility and comparison to cardiac magnetic resonance imaging. J Am Soc Echocardiogr 29:983–991
American Academy of Pediatrics Section on Cardiology and Cardiac Surgery (2005) Cardiovascular health supervision for individuals affected by Duchenne or Becker muscular dystrophy. Pediatrics 116:1569–1573
Bushby K, Muntoni F, Bourke JP (2003) 107th ENMC international workshop: the management of cardiac involvement in muscular dystrophy and myotonic dystrophy. 7th–9th June 2002, Naarden, the Netherlands. Neuromuscul Disord 13:166–72
Birnkrant DJ, Bushby K, Bann CM, Apkon SD, Blackwell A, Case LE et al (2018) Diagnosis and management of Duchenne muscular dystrophy, part 2: respiratory, cardiac, bone health, and orthopaedic management. Lancet Neurol 17:347–361
Ong KS, Kinnett K, Soelaeman R, Webb L, Bain JS, Martin AS et al (2018) Evaluating implementation of the updated care considerations for Duchenne muscular dystrophy. Pediatrics 142:S118–S128
Feingold B, Mahle WT, Auerbach S, Clemens P, Domenighetti AA, Jefferies JL et al (2017) Management of cardiac involvement associated with neuromuscular diseases: a scientific statement from the American Heart Association. Circulation 136:e200–e231
Tandon A, Villa CR, Hor KN, Jefferies JL, Gao Z, Towbin JA, Wong BL et al (2015) Myocardial fibrosis burden predicts left ventricular ejection fraction and is associated with age and steroid treatment duration in Duchenne muscular dystrophy. J Am Heart Assoc 4:e001338
Soslow JH, Damon SM, Crum K, Lawson MA, Slaughter JC, Xu M et al (2016) Increased myocardial native T1 and extracellular volume in patients with Duchenne muscular dystrophy. J Cardiovasc Magn Reson 18:5
Schelbert EB, Messroghli DR (2016) State of the art: clinical applications of cardiac T1 mapping. Radiology 278:658–676
Haaf P, Garg P, Messroghli DR, Broadbent DA, Greenwood JP, Plein S (2016) Cardiac T1 mapping and extracellular volume (ECV) in clinical practice: a comprehensive review. J Cardiovasc Magn Reson 18:89
Messroghli DR, Moon JC, Ferreira VM, Grosse-Wortmann L, He T, Kellman P et al (2017) Clinical recommendations for cardiovascular magnetic resonance mapping of T1, T2, T2* and extracellular volume: a consensus statement by the Society for Cardiovascular Magnetic Resonance (SCMR) endorsed by the European Association for Cardiovascular Imaging (EACVI). J Cardiovasc Magn Reson 19:75
Flett AS, Hayward MP, Ashworth MT, Hansen MS, Taylor AM, Elliott PM et al (2010) Equilibrium contrast cardiovascular magnetic resonance for the measurement of diffuse myocardial fibrosis: preliminary validation in humans. Circulation 122:138–144
Starc JJ, Moore RA, Rattan MS, Villa CR, Gao Z, Mazur W et al (2017) Elevated myocardial extracellular volume fraction in Duchenne muscular dystrophy. Pediatr Cardiol 38:1485–1492
Olivieri LJ, Kellman P, McCarter RJ, Cross RR, Hansen MS, Spurney CF (2016) Native T1 values identify myocardial changes and stratify disease severity in patients with Duchenne muscular dystrophy. J Cardiovasc Magn Reson 18:72
Bish LT, Yarchoan M, Sleeper MM, Gazzara JA, Morine KJ, Acosta P et al (2011) Chronic losartan administration reduces mortality and preserves cardiac but not skeletal muscle function in dystrophic mice. PLoS ONE 6:e20856
Chun JL, O’Brien R, Berry SE (2012) Cardiac dysfunction and pathology in the dystrophin and utrophin-deficient mouse during development of dilated cardiomyopathy. Neuromuscul Disord 22:368–379
Quinlan JG, Hahn HS, Wong BL, Lorenz JN, Wenisch AS, Levin LS (2004) Evolution of the mdx mouse cardiomyopathy: physiological and morphological findings. Neuromuscul Disord 14:491–496
Klingler W, Jurkat-Rott K, Lehmann-Horn F, Schleip R (2012) The role of fibrosis in Duchenne muscular dystrophy. Acta Myol 31:184–195
Burakiewicz J, Sinclair CDJ, Fischer D, Walter GA, Kan HE, Hollingsworth KG (2017) Quantifying fat replacement of muscle by quantitative MRI in muscular dystrophy. J Neurol 264:2053–2067
Tsai WC, Kao KJ, Chang KM, Hung CF, Yang Q, Lin CE et al (2017) B1 field correction of T1 estimation should be considered for breast dynamic contrast-enhanced MR imaging even at 1.5 T. Radiology 282:55–62
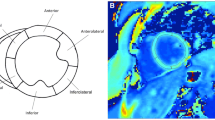
Cerqueira MD, Weissman NJ, Dilsizian V, Jacobs AK, Kaul S, Laskey WK, Pennell DJ et al (2002) Standardized myocardial segmentation and nomenclature for tomographic imaging of the heart. A statement for healthcare professionals from the Cardiac Imaging Committee of the Council on Clinical Cardiology of the American Heart Association. Int J Cardiovasc Imaging 18:539–542
Lang SM, Alsaied T, Moore RA, Rattan M, Ryan TD, Taylor MD (2019) Conservative gadolinium administration to patients with Duchenne muscular dystrophy: decreasing exposure, cost, and time, without change in medical management. Int J Cardiovasc Imaging 35(12):2213–2219
Niss O, Fleck R, Makue F, Alsaied T, Desai P, Towbin JA et al (2017) Association between diffuse myocardial fibrosis and diastolic dysfunction in sickle cell anemia. Blood 130:205–213
Puntmann VO, Voigt T, Chen Z, Mayr M, Karim R, Rhode K et al (2013) Native T1 mapping in differentiation of normal myocardium from diffuse disease in hypertrophic and dilated cardiomyopathy. JACC Cardiovasc Imaging 6:475–484
Puntmann VO, Peker E, Chandrashekhar Y, Nagel E (2016) T1 mapping in characterizing myocardial disease: a comprehensive review. Circ Res 119:277–299
Panovsky R, Pesl M, Holecek T, Machal J, Feitova V, Mrazova L et al (2019) Cardiac profile of the Czech population of Duchenne muscular dystrophy patients: a cardiovascular magnetic resonance study with T1 mapping. Orphanet J Rare Dis 14(1):10
Kellman P, Bandettini WP, Mancini C, Hammer-Hansen S, Hansen MS, Arai AE (2015) Characterization of myocardial T1-mapping bias caused by intramyocardial fat in inversion recovery and saturation recovery techniques. J Cardiovasc Magn Reson 17:33
Mordi I, Radjenovic A, Stanton T, Gardner RS, McPhaden A, Carrick D et al (2015) Prevalence and prognostic significance of lipomatous metaplasia in patients with prior myocardial infarction. JACC Cardiovasc Imaging 8:1111–1112
Reiter U, Reiter C, Krauter C, Fuchsjager M, Reiter G (2018) Cardiac magnetic resonance T1 mapping. Part 2: diagnostic potential and applications. Eur J Radiol 109:235–247
Baroldi G, Silver MD, De Maria R, Parodi O, Pellegrini A (1997) Lipomatous metaplasia in left ventricular scar. Can J Cardiol 13:65–71
Pouliopoulos J, Chik WW, Kanthan A, Sivagangabalan G, Barry MA, Fahmy PN et al (2013) Intramyocardial adiposity after myocardial infarction: new implications of a substrate for ventricular tachycardia. Circulation 128:2296–2308
Kim HK, Serai S, Lindquist D, Merrow AC, Horn PS, Kim DH et al (2015) Quantitative skeletal muscle MRI: part 2, MR spectroscopy and T2 relaxation time mapping-comparison between boys with Duchenne muscular dystrophy and healthy boys. AJR Am J Roentgenol 205:W216–W223
Hasuwa T, Kawano H, Fukae S, Arakawa S, Maemura K (2020) Fat infiltration in myocardium in Duchenne muscular dystrophy with atrial tachycardia. Eur Heart J Cardiovasc Imaging 21(8):922
Dabir D, Child N, Kalra A, Rogers T, Gebker R, Jabbour A et al (2014) Reference values for healthy human myocardium using a T1 mapping methodology: results from the International T1 Multicenter cardiovascular magnetic resonance study. J Cardiovasc Magn Reson 16:69
Piechnik SK, Ferreira VM, Lewandowski AJ, Ntusi NA, Banerjee R, Holloway C et al (2013) Normal variation of magnetic resonance T1 relaxation times in the human population at 1.5 T using ShMOLLI. J Cardiovasc Magn Reson 15:13
Rauhalammi SM, Mangion K, Barrientos PH, Carrick DJ, Clerfond G, McClure J et al (2016) Native myocardial longitudinal (T1) relaxation time: regional, age, and sex associations in the healthy adult heart. J Magn Reson Imaging 44:541–548
Kanda T, Fukusato T, Matsuda M, Toyoda K, Oba H, Kotoku J et al (2015) Gadolinium-based contrast agent accumulates in the brain even in subjects without severe renal dysfunction: evaluation of autopsy brain specimens with inductively coupled plasma mass spectroscopy. Radiology 276:228–232
Kanda T, Ishii K, Kawaguchi H, Kitajima K, Takenaka D (2014) High signal intensity in the dentate nucleus and globus pallidus on unenhanced T1-weighted MR images: relationship with increasing cumulative dose of a gadolinium-based contrast material. Radiology 270:834–841
Kanda T, Matsuda M, Oba H, Toyoda K, Furui S (2015) Gadolinium deposition after contrast-enhanced MR imaging. Radiology 277:924–925
Kanda T, Oba H, Toyoda K, Kitajima K, Furui S (2016) Brain gadolinium deposition after administration of gadolinium-based contrast agents. Jpn J Radiol 34:3–9
Hor KN, Taylor MD, Al-Khalidi HR, Cripe LH, Raman SV, Jefferies JL et al (2013) Prevalence and distribution of late gadolinium enhancement in a large population of patients with Duchenne muscular dystrophy: effect of age and left ventricular systolic function. J Cardiovasc Magn Reson 15:107
Acknowledgements
The authors would like to acknowledge the Heart Institute and the Heart Institute Research Core at Cincinnati Children’s Hospital Medical Center for their support of the project.
Funding
N/A.
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
Conflict of interest
The authors declare that they have no competing interests or funds to disclose.
Ethical approval
This study was approved by the Institutional Review Board at Cincinnati Children’s Hospital Medical Center.
Informed consent
The requirement for informed consent was waived due to the retrospective nature of the study.
Additional information
Publisher’s Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Rights and permissions
About this article
Cite this article
Lang, S.M., Alsaied, T., Khoury, P.R. et al. Variations in native T1 values in patients with Duchenne muscular dystrophy with and without late gadolinium enhancement. Int J Cardiovasc Imaging 37, 635–642 (2021). https://doi.org/10.1007/s10554-020-02031-z
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s10554-020-02031-z