Abstract
Purpose
The combination of cyclin-dependent kinase 4/6 inhibitors and endocrine therapy is a standard treatment for hormone receptor (HR)-positive/human epidermal growth factor receptor 2 (HER2)-negative metastatic breast cancer (MBC); however, their toxicities and financial burden are major issues, especially for prolonged treatment. We investigated fulvestrant plus palbociclib in patients with HR-positive MBC resistant to fulvestrant monotherapy.
Methods
Patients who initially received fulvestrant as their first- or second-line endocrine therapy were assigned to group A. Patients with disease progression during fulvestrant monotherapy who subsequently received fulvestrant plus palbociclib were assigned to group B. The primary endpoint was progression-free survival (PFS1) in group B. We set the threshold median PFS of 5 months (null hypothesis).
Results
Between January 2018 and February 2020 we enrolled 167 patients in group A (January 2018–February 2020) from 55 institutions, of whom 72 subsequently received fulvestrant plus palbociclib and were enrolled in group B. The median follow-up was 23.8 and 8.9 months in groups A and B, respectively. The median PFS in group B (combination therapy) was 9.4 (90% confidence interval [CI]: 6.9–11.2) months (p < 0.001). This was 25.7 (90% CI: 21.2–30.3) months in group A (fulvestrant monotherapy). The TTF in group B was 7.2 (90% CI: 5.5–10.4) months. In the post-hoc analysis, the median PFS1 in group B among patients with longer-duration fulvestrant monotherapy (> 1 year) was longer than that of patients with shorter-duration monotherapy (≤ 1 year) (11.3 vs. 7.6 months). No new toxicities were observed.
Conclusion
Our findings suggest that palbociclib plus fulvestrant after disease progression despite fulvestrant monotherapy is potentially safe and effective in patients with HR-positive/HER2-negative advanced MBC.
Similar content being viewed by others
Avoid common mistakes on your manuscript.
Introduction
The aim of advanced breast cancer (ABC) treatment is prolonged overall survival (OS) while maintaining the patient’s quality of life (QOL) [1]. ABC treatment has become increasingly complex owing to multiple newly approved drugs for the treatment of hormone receptor (HR)-positive ABC. Fulvestrant, a selective estrogen receptor degrader and standard endocrine therapy (ET) for HR-positive ABC, is associated with prolonged progression-free survival (PFS) in postmenopausal women in both first- and second-line treatment settings [1,2,3,4]. The Phase III FALCON trial assessed fulvestrant as a first-line treatment and found significant improvement in the median PFS with fulvestrant than with an aromatase inhibitor (AI) such as anastrozole (16.6 vs. 13.8 months) [3].
Cyclin-dependent kinase (CDK) 4/6 inhibitors are used in ABC treatment, inhibiting CDK 4 and CDK 6 in vitro, resulting in decreased RB1 phosphorylation (a tumor suppressor protein) [5]. Positive activity has been observed in breast cancer cell lines with these inhibitors when used in monotherapy, which is synergistic with other endocrine therapies [6]. In patients with metastatic, estrogen receptor-positive breast cancer with AI resistance in the PALOMA-3 trial, the combination of palbociclib–fulvestrant therapy was associated with significantly longer PFS than that of fulvestrant alone [7, 8]. These findings suggest that palbociclib may potentially reverse ET resistance in patients with previous responses to ET, making other drugs, such as AI or fulvestrant, more effective. The TREnd trial investigated the activity of palbociclib combined with the same ET that was received prior to disease progression. The clinical benefit rate was 54%, and the median PFS was 10.8 months in patients who received combination therapy. This benefit may be attributed to the additional therapeutic action of ET following the reversal of prior ET resistance by palbociclib [9].
Patients with ABC often receive multiple drugs throughout treatment, which can negatively impact their QOL; therefore, the adverse-event profile of any treatment is particularly important in this setting. Hence, less toxic treatment strategies that favor HR-positive patients regarding non-difference in OS are important and remain an unmet clinical need. Furthermore, the addition of palbociclib to fulvestrant therapy costs an estimated $918,166 per quality-adjusted life-year (QALY) gained, which is nine times higher than the willingness-to-pay threshold of $100,000 per QALY [10].
We hypothesized that adding palbociclib to fulvestrant therapy would be effective in patients with HR-positive ABC that has progressed despite fulvestrant therapy. Our primary objective was to observe PFS in patients resistant to fulvestrant monotherapy and subsequently treated with fulvestrant plus palbociclib. The secondary objective was to observe PFS in HR-positive ABC patients treated with fulvestrant as first- and second-line therapy.
Methods
Study protocol
The FUTURE trial was a multicenter, prospective cohort study that evaluated the safety and effectiveness of adding palbociclib to fulvestrant therapy for patients with HR-positive ABCs and disease progression despite fulvestrant monotherapy. Patients receiving fulvestrant monotherapy as their first or second endocrine therapy were enrolled (group A). Patients with disease progression during fulvestrant monotherapy were subsequently registered in group B.
Eligible patients were enrolled at 55 investigation sites in academic and community settings in Japan, in accordance with the following key inclusion criteria: (1) women ≥ 20 but < 80 years old with histologically or cytologically confirmed metastatic HR-positive/human epidermal growth factor receptor 2 (HER2)-negative breast cancer; (2) treated with fulvestrant monotherapy as first- or second-line therapy for ABC; and (3) no previous systemic therapy for breast cancer (except for one line of cytotoxic chemotherapy). Patients who did not experience progressive disease during fulvestrant monotherapy and those with severe or uncontrolled medical conditions were excluded. This study was conducted according to the tenets of the Declaration of Helsinki and approved by the institutional review board of Fukushima medical university. All patients provided written informed consent prior to participation.
The study protocol was registered with the University Hospital Medical Information Network, Japan (protocol ID 000,016,109) and at Clinical trials.gov (NCT 02,376,985).
Procedures
Fulvestrant (500 mg) was administered on the following days: 0, 14 (plus 7 days), 28 (plus 7 days), and every 28 (plus 7 days) days thereafter in two 5-mL intramuscular injections at each visit. Fulvestrant dose reductions were not permitted. Treatment continued until objective disease progression was noted or other criteria for discontinuation arose.
Study visits occurred during screenings (within 28 days before registration) and every 4 weeks thereafter until disease progression. Safety and tolerability were assessed at each visit.
Patients were subsequently registered in group B if they experienced disease progression during fulvestrant monotherapy. They continued receiving 500 mg fulvestrant via intramuscular injection in subsequent 28-day cycles and were also orally administered 125 mg palbociclib once daily for 3 weeks, followed by 1 week off in a 28-day cycle. The study treatment continued until disease progression, unacceptable toxic effects, consent withdrawal, or death. Dose interruption, reduction, or delay according to a predefined dose-modification strategy was acceptable for patients who experienced toxic effects related to the investigational drugs.
We assessed tumors at baseline and every 8 weeks (± 14 days) for the first 24 weeks after the first fulvestrant administration and every 12 weeks (± 14 days) thereafter using computed tomography, radiography, or both in all patients.
The assessment of adverse events included incidence and severity (graded according to the National Cancer Institute Common Terminology Criteria, Version 4.0), timing, seriousness, and relatedness to the study treatment.
Estrogen receptor-positive, progesterone receptor-positive tumors, or both, and HER2-negative tumors were locally assessed using an assay consistent with local standards.
Outcome measurement
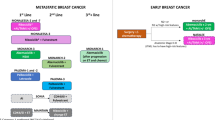
The primary objective was PFS from the start of combination therapy in group B patients (PFS1) (Supplemental Fig. 1). The secondary objective was PFS stratified by patients treated with fulvestrant monotherapy as the first- or second-line therapy in group A (PFS2). Additional endpoints included PFS from the start of monotherapy to failure combination therapy in group B (PFS3), time to treatment failure (TTF) from the start of both fulvestrant monotherapy and combination therapy, OS from the start of both fulvestrant monotherapy and combination therapy, objective response rates (fulvestrant monotherapy, combination of fulvestrant and palbociclib), safety (fulvestrant monotherapy, combination of fulvestrant and palbociclib), and biomarkers.
Statistical analysis
We set the threshold median PFS of 5 months (null hypothesis), which was the reported difference between the fulvestrant monotherapy and combination therapy groups in the PALOMA-3 study. Assuming a median PFS1 of 8 months in group B, the minimum sample size required was 63 patients, with a power of 80% under a one-sided alpha of 0.05. The accrual and follow-up periods were set at 12 and 18 months, respectively. The target number of accrual patients was determined at 70 in the second registration (group B).
The primary analysis was the estimation of two-sided 90% confidence intervals (CIs) for PFS1 and hypothetical testing against the null hypothesis; the median was 5 months. The Kaplan–Meier method was used to summarize the PFS1-3, TTFs, and OS. The standard error of the annual rates and two-sided 90% CIs were calculated using Greenwood's formula. Frequencies and proportions were used to tabulate the overall response rates. The worst grades relating to safety observed during the treatment period were summarized.
Results
Patient characteristics
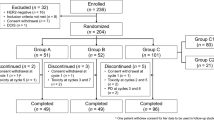
We enrolled 167 patients from 55 institutions between January 2018 and February 2020 in group A and 72 patients in group B. Nine patients from group A did not receive the protocol treatment and were excluded from the analysis. Once the 72 patients were enrolled in group B, enrollment was considered complete, and patients with disease progression in group A thereafter were not included (Fig. 1). Ultimately, the data of 158 patients were included in the analysis. The median follow-up time from enrollment was 23.8 and 8.9 months in groups A and B, respectively. Two patients who received monotherapy in group A were still receiving treatment at the data cutoff point.
In group B, the median age was 67 years; 20 (28%) patients did not receive ET for ABC, 52 (72%) patients received ET before fulvestrant monotherapy, 59 (82%) patients had progesterone receptor-positive tumors, and 82 (51%) patients had visceral disease (Table 1).
Clinical outcomes in group B
Regarding the primary endpoint, the median PFS1 in group B was 9.4 (90% CI = 6.9–11.2; p < 0.001) months (Fig. 2a). The TTF from the start of combination therapy in group B was 7.2 (90% CI = 5.5–10.4) months (Fig. 2b). The median PFS3 in group B was 25.6 (90% CI = 22.1–28.4) months (Fig. 3). PFS1 in group B patients who received fulvestrant as the first-line treatment (median, 8.2 months) was not as long as that of patients who received fulvestrant as the second-line treatment (median, 10.6 months) (Supplemental Fig. 2). PFS among patients with visceral disease (median, 11.3 months) was not significantly different from those without (median, 8.2 months). Other factors, such as de novo metastatic cancer and age > 65, were not significantly different regarding PFS.
In the post-hoc analysis, we explored whether patients who received longer-duration fulvestrant monotherapy would show longer PFS than those receiving shorter-duration monotherapy. The median PFS among patients with longer-duration monotherapy (> 1 year) was 3.7 months longer than that of patients with shorter-duration monotherapy (≤ 1 year) (11.3 vs. 7.6 months).
The overall response rate in group B was 8.3%, and the clinical benefit rate was 37.5% (Table 2).
Clinical outcomes in group A
The median PFS2 for monotherapy patients in group A was 25.7 (90% CI = 21.2–30.3) months (Fig. 4). PFS for patients in group A who received fulvestrant as the first-line treatment (median, 30.3 months) was not significantly different from that of patients who received fulvestrant as the second-line treatment (median, 21.5 months). PFS for patients in group A with visceral disease (median, 25.8 months) was not significantly different from those without (median, 25.4 months). The overall response rate in group A was 22.4%, and the clinical benefit rate was 58.9% (Table 2).
Safety
The adverse events are shown in Tables 3 and 4, with no new safety signals detected. Ultimately, 65 (90%) patients in group B and 78 (49%) in group A reported the occurrence of at least one adverse event in one or more cycles. Hematological toxicities were the most common adverse events in group B. Neutropenia occurred in 62 (86%) patients in group B (43 [59%]) and 17 [23%] were grades 3 and 4, respectively). Infections and febrile neutropenia occurred in two patients. Nine (12.5%) patients reported at least one serious treatment-related adverse event.
Dose reductions occurred in 53 patients (73%) in group B, predominantly due to hematological toxicity (46 [86%]). Similarly, dose delays occurred in 63 (87%) patients. The final palbociclib dose before disease progression was 125 mg in 18 (25%) patients, 100 mg in 24 (33.8%) patients, 75 mg in 14 (19%) patients, and 75 mg in 10 (14%) patients with 2 weeks on and 2 weeks off.
Discussion
This study investigated the strategy of adding palbociclib to fulvestrant after disease progression in patients with HR-positive/HER2-negative ABC. Our data suggest that this treatment strategy is safe, with a median PFS1 of 9.4 months. The primary endpoint was met based on study assumptions. Palbociclib may reverse endocrine therapy resistance in patients receiving fulvestrant treatment. The median PFS3 (fulvestrant monotherapy to treatment failure with fulvestrant plus palbociclib) was 25.6 months. These data are similar to those of combined ET with CDK 4/6 agents in frontline treatment. The strategy of adding palbociclib to ET was also investigated in the TREnd trial [9]. Regarding the activity of palbociclib when given as either a single-agent or in combination with ET after disease progression, the clinical benefit rates for the single-agent and combination groups were 60% and 54%, respectively. The median PFS was 6.5 months and 10.8 months in the single-agent and combination groups, respectively. The strategy of adding palbociclib appears to be beneficial and safe for patients with ET resistance.
Endocrine therapy remains the standard HR-positive/HER2-negative ABC therapy before chemotherapy [4]. Recently, multiple-target therapy with ET was approved, including CDK 4/6, mammalian/mechanistic target of rapamycin, and phosphoinositide 3-kinase inhibitors. However, ET is typically limited to selective estrogen receptor modulators, selective estrogen receptor degraders, and AIs. Most patients receiving targeted therapy have resistance to the same class of ET; therefore, strategies to overcome resistance are of ongoing interest. Preclinical evidence suggests that palbociclib could overcome conditioned resistance to a given ET [11].
Multiple large, phase III studies have confirmed the efficacy of ET combined with CDK 4/6 agents in front- or later-line treatment settings [7, 8, 12, 13]. The strategy of changing to another endocrine agent combined with a CDK4/6 inhibitor has been explored in large phase III clinical trials, with superiority observed in combined therapy over ET alone [7, 8, 12, 13]. The combination of fulvestrant with CDK 4/6 agents in frontline treatment prolonged PFS and OS compared with fulvestrant monotherapy in the MONARCH 2 and MONALEESA-3 trials [13] [14]. The median PFS in patients receiving fulvestrant combined with a CDK4/6 agent in a first-line setting was 33.6 months in the MONALEESA-3 trial, 14.6 months in a second-line setting in the MONALEESA-3 trial, and 16 months in the MONARCH-2 trial. The PFS3 from fulvestrant monotherapy to combined fulvestrant and palbociclib therapy was 25.6 months. However, our strategy included patients who experienced disease progression twice. Despite the limitations in making indirect comparisons across studies, our data and those of the TRrend trial suggest that the strategy of adding a CDK 4/6 inhibitor to the same ET after disease progression may merit further study in a selected population with prolonged benefit during their prior line of ET.
Another noteworthy study is the SONIA-trial [15], an investigator-initiated, multicenter, randomized Phase III study. Its primary objective is to evaluate if treatment with a non-steroidal AI combined with CDK4/6 inhibition as the 1st-line therapy followed by fulvestrant as the 2nd-line therapy (strategy A) could improve PFS, as compared to treatment with a non-steroidal AI as the 1st-line therapy followed by fulvestrant combined with CDK4/6 inhibition as the 2nd-line therapy (strategy B). The SONIA trial will provide evidence in terms of benefit in PFS with an up-front CDK4/6 inhibitor in combination with ET.
In the FALCON trial, fulvestrant had a beneficial treatment effect compared with that of anastrozole in patients with de novo stage 4 cancer, particularly in patients without visceral disease [3]. However, the PARSIFAL study showed that the combination of fulvestrant and palbociclib showed no superiority in PFS over letrozole-palbociclib combination therapy in a patient population among patients with previously untreated ABC [16]. Subgroup analysis showed that patients with de novo stage 4 and non-visceral disease showed no benefit from fulvestrant combined with palbociclib, which is inconsistent with the results of the FALCON trial. Combination therapy with CDK 4/6 inhibitors did not maintain fulvestrant efficacy compared with an AI.
Our data indicated a correlation between fulvestrant monotherapy and treatment duration after combining palbociclib with fulvestrant. In the TREnd trial, subgroup analysis of patients with a history of ET ≥ 6 months showed better PFS than patients with a history of ET < 6 months. Our trial and the TREnd trial demonstrated that patients with a history of long-term ET had better PFS.
Acquired resistance to AI frequently stems from ESR1-mutated subclones, which may be sensitive to fulvestrant and oral selective ER degraders (SERDs). The PADA-1 trial [17] showed that the combination of fulvestrant with palbociclib prolonged PFS in patients with rising ESR1 mutations detected by circulating tumor (ct)DNA. In addition, the SELENA-6 trial will evaluate the hypothesis that switching to a SERD combination with a CDK4/6 inhibitor is effective for patients with detectable ESR1 mutations but without disease progression during 1st-line treatment with AI and a CDK4/6 inhibitor. Oral SERDs such as Elacestrant [18] have demonstrated a significant PFS improvement in patients with ESR1 mutations. Our study collected plasma samples at three time points: before adding palbociclib, on day 15 of the first cycle, and at the end of treatment. Analysis of ctDNA helped us select our treatment strategy, and palbociclib may have the potential to reverse endocrine therapy resistance in patients resistant to fulvestrant.
This study had some limitations. First, the number of patients was too small to confirm whether patients overcame ET resistance. Second, in the single-arm registration study of fulvestrant monotherapy, the study population was more fulvestrant sensitive than the general population. Moreover, patients with early treatment failure on fulvestrant monotherapy were difficult to register. Third, the median follow-up duration was too short to evaluate OS in patients with HR-positive ABC.
In conclusion, our data suggest that palbociclib plus fulvestrant after disease progression with fulvestrant monotherapy may be effective and safe in patients with HR-positive/HER2-negative ABC or MBC. This strategy may be an option for patients with ABC resistant to fulvestrant monotherapy.
Data availability
The datasets generated and/or analyzed during the current study are available from the corresponding author upon reasonable request.
References
Cardoso F, Senkus E, Costa A, Papadopoulos E, Aapro M, Andre F, Harbeck N, Aguilar Lopez B, Barrios CH, Bergh J, Biganzoli L, Boers-Doets CB, Cardoso MJ, Carey LA, Cortes J, Curigliano G, Dieras V, El Saghir NS, Eniu A, Fallowfield L, Francis PA, Gelmon K, Johnston SRD, Kaufman B, Koppikar S, Krop IE, Mayer M, Nakigudde G, Offersen BV, Ohno S, Pagani O, Paluch-Shimon S, Penault-Llorca F, Prat A, Rugo HS, Sledge GW, Spence D, Thomssen C, Vorobiof DA, Xu B, Norton L, Winer EP (2018) 4th ESO-ESMO International Consensus Guidelines for Advanced Breast Cancer (ABC 4)†. Ann Oncol 29:1634–1657. https://doi.org/10.1093/annonc/mdy192
Di Leo A, Jerusalem G, Petruzelka L, Torres R, Bondarenko IN, Khasanov R, Verhoeven D, Pedrini JL, Smirnova I, Lichinitser MR, Pendergrass K, Garnett S, Lindemann JP, Sapunar F, Martin M (2010) Results of the CONFIRM phase III trial comparing fulvestrant 250 mg with fulvestrant 500 mg in postmenopausal women with estrogen receptor-positive advanced breast cancer. J Clin Oncol 28:4594–4600. https://doi.org/10.1200/JCO.2010.28.8415
Robertson JFR, Bondarenko IM, Trishkina E, Dvorkin M, Panasci L, Manikhas A, Shparyk Y, Cardona-Huerta S, Cheung KL, Philco-Salas MJ, Ruiz-Borrego M, Shao Z, Noguchi S, Rowbottom J, Stuart M, Grinsted LM, Fazal M, Ellis MJ (2016) Fulvestrant 500 mg versus anastrozole 1 mg for hormone receptor-positive advanced breast cancer (Falcon): an international, randomised, double-blind, phase 3 trial. Lancet 388:2997–3005. https://doi.org/10.1016/S0140-6736(16)32389-3
Rugo HS, Rumble RB, Macrae E, Barton DL, Connolly HK, Dickler MN, Fallowfield L, Fowble B, Ingle JN, Jahanzeb M, Johnston SR, Korde LA, Khatcheressian JL, Mehta RS, Muss HB, Burstein HJ (2016) Endocrine therapy for hormone receptor-positive metastatic breast cancer: American Society of Clinical Oncology guideline. J Clin Oncol 34:3069–3103. https://doi.org/10.1200/JCO.2016.67.1487
Fry DW, Harvey PJ, Keller PR, Elliott WL, Meade M, Trachet E, Albassam M, Zheng X, Leopold WR, Pryer NK, Toogood PL (2004) Specific inhibition of cyclin-dependent kinase 4/6 by PD 0332991 and associated antitumor activity in human tumor xenografts. Mol Cancer Ther 3:1427–1438. https://doi.org/10.1158/1535-7163.1427.3.11
Toogood PL, Harvey PJ, Repine JT, Sheehan DJ, VanderWel SN, Zhou H, Keller PR, McNamara DJ, Sherry D, Zhu T, Brodfuehrer J, Choi C, Barvian MR, Fry DW (2005) Discovery of a potent and selective inhibitor of cyclin-dependent kinase 4/6. J Med Chem 48:2388–2406. https://doi.org/10.1021/jm049354h
Cristofanilli M, Turner NC, Bondarenko I, Ro J, Im SA, Masuda N, Colleoni M, DeMichele A, Loi S, Verma S, Iwata H, Harbeck N, Zhang K, Theall KP, Jiang Y, Bartlett CH, Koehler M, Slamon D (2016) Fulvestrant plus palbociclib versus fulvestrant plus placebo for treatment of hormone-receptor-positive, HER2-negative metastatic breast cancer that progressed on previous endocrine therapy (PALOMA-3): Final analysis of the multicentre, double-blind, phase 3 randomised controlled trial. Lancet Oncol 17:425–439. https://doi.org/10.1016/S1470-2045(15)00613-0
Turner NC, Slamon DJ, Ro J, Bondarenko I, Im SA, Masuda N, Colleoni M, DeMichele A, Loi S, Verma S, Iwata H, Harbeck N, Loibl S, André F, Puyana Theall K, Huang X, Giorgetti C, Huang Bartlett C, Cristofanilli M (2018) Overall survival with palbociclib and fulvestrant in advanced breast cancer. N Engl J Med 379:1926–1936. https://doi.org/10.1056/NEJMoa1810527
Malorni L, Curigliano G, Minisini AM, Cinieri S, Tondini CA, D’Hollander K, Arpino G, Bernardo A, Martignetti A, Criscitiello C, Puglisi F, Pestrin M, Sanna G, Moretti E, Risi E, Biagioni C, McCartney A, Boni L, Buyse M, Migliaccio I, Biganzoli L, Di Leo A (2018) Palbociclib as single agent or in combination with the endocrine therapy received before disease progression for estrogen receptor-positive, HER2-negative metastatic breast cancer: TREnd trial. Ann Oncol 29:1748–1754. https://doi.org/10.1093/annonc/mdy214
Mamiya H, Tahara RK, Tolaney SM, Choudhry NK, Najafzadeh M (2017) Cost-effectiveness of palbociclib in hormone receptor-positive advanced breast cancer. Ann Oncol 28:1825–1831. https://doi.org/10.1093/annonc/mdx201
Finn RS, Dering J, Conklin D, Kalous O, Cohen DJ, Desai AJ, Ginther C, Atefi M, Chen I, Fowst C, Los G, Slamon DJ (2009) PD 0332991, a selective cyclin D kinase 4/6 inhibitor, preferentially inhibits proliferation of luminal estrogen receptor-positive human breast cancer cell lines in vitro. Breast Cancer Res 11:R77. https://doi.org/10.1186/bcr2419
Finn RS, Martin M, Rugo HS, Jones S, Im SA, Gelmon K, Harbeck N, Lipatov ON, Walshe JM, Moulder S, Gauthier E, Lu DR, Randolph S, Diéras V, Slamon DJ (2016) Palbociclib and letrozole in advanced breast cancer. N Engl J Med 375:1925–1936. https://doi.org/10.1056/NEJMoa1607303
Sledge GW Jr, Toi M, Neven P, Sohn J, Inoue K, Pivot X, Burdaeva O, Okera M, Masuda N, Kaufman PA, Koh H, Grischke EM, Frenzel M, Lin Y, Barriga S, Smith IC, Bourayou N, Llombart-Cussac A (2017) MONARCH 2: Abemaciclib in combination with fulvestrant in women with HR+/HER2- advanced breast cancer who had progressed while receiving endocrine therapy. J Clin Oncol 35:2875–2884. https://doi.org/10.1200/JCO.2017.73.7585
Slamon DJ, Neven P, Chia S, Fasching PA, De Laurentiis M, Im SA, Petrakova K, Bianchi GV, Esteva FJ, Martín M, Nusch A, Sonke GS, De la Cruz-Merino L, Beck JT, Pivot X, Vidam G, Wang Y, Rodriguez Lorenc K, Miller M, Taran T, Jerusalem G (2018) Phase III randomized study of ribociclib and fulvestrant in hormone receptor-positive, human epidermal growth factor receptor 2-negative advanced breast cancer: MONALEESA-3. J Clin Oncol 36:2465–2472. https://doi.org/10.1200/JCO.2018.78.9909
van Ommen-Nijhof A, Konings IR, van Zeijl CJJ, Uyl-de Groot CA, van der Noort V, Jager A, Sonke GS, SONIA study steering committee (2018) Selecting the optimal position of CDK4/6 inhibitors in hormone receptor-positive advanced breast cancer—the SONIA study: Study protocol for a randomized controlled trial. BMC Cancer 18:1146. https://doi.org/10.1186/s12885-018-4978-1
Llombart-Cussac A, Pérez-García JM, Bellet M, Dalenc F, Gil-Gil M, Ruíz-Borrego M, Gavilá J, Sampayo-Cordero M, Aguirre E, Schmid P, Marmé F, Di Cosimo S, Gligorov J, Schneeweiss A, Albanell J, Zamora P, Wheatley D, Martínez-de Dueñas E, Amillano K, Malfettone A, Cortés J, Steering Committee PARSIFAL, Investigato T (2021) Fulvestrant-palbociclib vs letrozole-palbociclib as initial therapy for endocrine-sensitive, hormone receptor-positive, ERBB2-negative advanced breast cancer: a randomized clinical trial. JAMA Oncol 7:1791–1799. https://doi.org/10.1001/jamaoncol.2021.4301
Bidard FC, Hardy-Bessard AC, Dalenc F, Bachelot T, Pierga JY, de la Motte RT, Sabatier R, Dubot C, Frenel JS, Ferrero JM, Ladoire S, Levy C, Mouret-Reynier MA, Lortholary A, Grenier J, Chakiba C, Stefani L, Plaza JE, Clatot F, Teixeira L, D’Hondt V, Vegas H, Derbel O, Garnier-Tixidre C, Canon JL, Pistilli B, André F, Arnould L, Pradines A, Bièche I, Callens C, Lemonnier J, Berger F, Delaloge S, Bidard F, Pistilli B, Dalenc F, Bachelot T, De La Motte RT, Sabatier R, Dubot C, Frenel J, Ferrero J, Ladoire S, Levy C, Mouret-reynier M, Hardy-bessard A, Lortholary A, Grenier J, Chakiba C, Stefani L, Soulie P, Jacquin J, Plaza JE, Clatot F, Teixeira L, D’hondt V, Vegas H, Derbel O, Garnier Tixidre C, Delbaldo C, Moreau L, Cheneau C, Paitel J, Bernard-marty C, Spaeth D, Genet D, Moullet I, Bonichon-lamichhane N, Deiana L, Greilsamer C, Venat-bouvet L, Delecroix V, Melis A, Orfeuvre H, Nguyen S, Legouffe E, Zannetti A, Le Scodan R, Dohollou N, Dalivoust P, Arsene O, Marques N, Petit T, Mollon D, Dauba J, Bonnin N, Morvan F, Gardner M, Marti A, Levache C, Lachaier E, Achille M, Valmar C, Bouaita R, Medioni J, Foa C, Bernard-marty C, Del Piano F, Gozy M, Escande A, Leduc N, Lucas B, Mille D, Ammarguellat H, Najem A, Trouboul F, Barthelemy P, Desclos H, Mayeur D, Lorchel F, Guinet F, Laurenty A, Boudrant A, Gisserot O, Alleaume C, De Gramont A (2022) Switch to fulvestrant and palbociclib versus no switch in advanced breast cancer with rising ESR1 mutation during aromatase inhibitor and palbociclib therapy (PADA-1): a randomised, open-label, multicentre, phase 3 trial. Lancet Oncol 23:1367–1377. https://doi.org/10.1016/S1470-2045(22)00555-1
Bidard FC, Kaklamani VG, Neven P, Streich G, Montero AJ, Forget F, Mouret-Reynier MA, Sohn JH, Taylor D, Harnden KK, Khong H, Kocsis J, Dalenc F, Dillon PM, Babu S, Waters S, Deleu I, García Sáenz JA, Bria E, Cazzaniga M, Lu J, Aftimos P, Cortés J, Liu S, Tonini G, Laurent D, Habboubi N, Conlan MG, Bardia A (2022) Elacestrant (oral selective estrogen receptor degrader) versus Standard Endocrine Therapy for estrogen receptor-Positive, Human epidermal growth factor Receptor 2-Negative Advanced Breast Cancer: Results from the Randomized Phase III EMERALD Trial. J Clin Oncol 40:3246–3256. https://doi.org/10.1200/JCO.22.00338
Acknowledgements
We greatly appreciate all women who participated in this trial. We also thank all investigators and their collaborators for their dedication to this study, Mebics for their data entry assistance, and the Japan Breast Cancer Research Group (JBCRG) for their administrative assistance.
Funding
This work was supported by the Japan Breast Cancer Research Group (JBCRG), which participated in the conduction of the study, and AstraZeneca.
Author information
Authors and Affiliations
Contributions
KW and MO: writing—review & editing, writing—original draft, conceptualization, formal analysis. NN: writing—review & editing, writing—original draft, conceptualization. YK, KK, NI, TT, and TI: writing—review & editing, conceptualization. HT, SO, UT, YY, MT, and TO: Writing—review & editing. HI: writing—review & editing, writing—original draft, project administration, conceptualization. NM: writing—review & editing, project administration, conceptualization, formal analysis. SS: writing—review & editing, writing—original draft, project administration, conceptualization, formal analysis.
Corresponding author
Ethics declarations
Conflict of interest
Kenichi Watanabe received personal fees from Chugai, Eli Lilly, Nippon Kayaku, Kyowa-Kirin, Novartis, Taiho, Eisai, Pfizer and Shionogi, outside the submitted work. Naoki Niikura received research funding to Tokai University from Novartis, Chugai, Daiichi Sankyo, Pfizer, Eisai, Eli Lilly and Mochida, honoraria, consultancy, and speaker fees from AstraZeneca, Novartis, Eisai, Eli Lilly, Chugai, Daiichi Sankyo, and Pfizer, outside the submitted work. Yuichiro Kikawa received consulting fee from Daiichi Sankyo, personal fees from AstraZeneca, Novartis, Taiho, Chugai, Daiichi Sankyo, Eisai and Kyowa-Kirin, outside the submitted work. Mari Oba received payment for educational lecture from AstraZeneca and Pfizer, outside the submitted work. Kokoro Kobayashi received personal fees from Pfizer, Chugai, Novartis, Taiho, Eli Lilly and AstraZeneca, outside the submitted work. Hiroshi Tada received research funding to Tohoku University from Taiho, Kyowa-Kirin and Eisai, personal fees from Chugai, Pfizer, Eli Lilly and Daiichi Sankyo, outside the submitted work. Uhi Toh received personal fees from Chugai, Eisai, Eli Lilly, Pfizer, Daiichi Sankyo and Taiho, outside the submitted work. Yutaka Yamamoto received research funding to Kumamoto University Hospital from Chugai, Kyowa-Kirin, Eisai, Daiichi Sankyo, Nippon-Kayaku, Taiho, Takeda, Eli Lilly, Pfizer and Novartis, honoraria for lectures from AstraZeneca, Chugai, Kyowa-Kirin, Novartis, Eli Lilly, Pfizer, Daiichi Sankyo, Nippon Kayaku, Taiho, Eisai, Takeda, MSD, Sysmex and Exact Science, outside the submitted work. Hiroshi Ishiguro received contract fees to Saitama Medical University International Medical Center from Eisai, speaker fees from Pfizer, outside the submitted work. Norikazu Masuda received research funding to Nagoya University Hospital from Chugai, Eli Lilly, AstraZeneca, Pfizer, Daiichi Sankyo, MSD, Eisai, Novartis, Sanofi and Kyowa-Kirin, personal fees from Chugai, Pfizer, AstraZeneca, Eli Lilly and Eisai, Representative of a board of directors of Japan Breast Cancer Research Group (JBCRG) unpaid, Board of Directors of Japanese Breast Cancer Society (JBCS) unpaid, outside the submitted work. Shigehira Saji received Grants from Eisai, Takeda and Eli Lilly, Contracted clinical trials from MSD and AstraZeneca, Grant and Contracted clinical trials from Taiho, Chugai and Daiichi Sankyo to Fukushima Medical University, personal fees from Chugai, Kyowa-Kirin, MSD, Novartis, Eisai, Takeda, Daiichi Sankyo, Eli Lilly, AstraZeneca, Pfizer, Taiho, Ono and Nippon Kayaku, personal fees for Participation on a Data Safety Monitoring Board or Advisory Board from Chugai/Roche, AstraZeneca, Eli Lilly, Pfizer, Kyowa-Kirin and Daiichi Sankyo, Executive board member of JBCRG, JBCS, Japanese Society of Medical Oncology (JSMO) and Breast International Group (BIG), outside the submitted work. The other authors have nothing to declare.
Ethical approval
This study was conducted according to the tenets of the declaration of Helsinki and approved by the institutional review board of Fukushima medical university.
Consent to participations
All patients provided written informed consent prior to participation.
Consent to publications
Our manuscript did not contain any individual person’s data in any form (including any individual details, images or videos.
Additional information
Publisher's Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Supplementary Information
Below is the link to the electronic supplementary material.
Rights and permissions
Open Access This article is licensed under a Creative Commons Attribution 4.0 International License, which permits use, sharing, adaptation, distribution and reproduction in any medium or format, as long as you give appropriate credit to the original author(s) and the source, provide a link to the Creative Commons licence, and indicate if changes were made. The images or other third party material in this article are included in the article's Creative Commons licence, unless indicated otherwise in a credit line to the material. If material is not included in the article's Creative Commons licence and your intended use is not permitted by statutory regulation or exceeds the permitted use, you will need to obtain permission directly from the copyright holder. To view a copy of this licence, visit http://creativecommons.org/licenses/by/4.0/.
About this article
Cite this article
Watanabe, K., Niikura, N., Kikawa, Y. et al. Fulvestrant plus palbociclib in advanced or metastatic hormone receptor-positive/human epidermal growth factor receptor 2-negative breast cancer after fulvestrant monotherapy: Japan Breast Cancer Research Group-M07 (FUTURE trial). Breast Cancer Res Treat 199, 253–263 (2023). https://doi.org/10.1007/s10549-023-06911-5
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s10549-023-06911-5