Abstract
Purpose
Breast cancer is a heterogeneous disease with different gene expression profiles, treatment options and outcomes. In South Africa, tumors are classified using immunohistochemistry. In high-income countries multiparameter genomic assays are being utilized with implications for tumor classification and treatment.
Methods
In a cohort of 378 breast cancer patients from the SABCHO study, we investigated the concordance between tumor samples classified by IHC and the PAM50 gene assay.
Results
IHC classified patients as ER-positive (77.5%), PR-positive (70.6%), and HER2-positive (32.3%). These results, together with Ki67, were used as surrogates for intrinsic subtyping, and showed 6.9% IHC-A-clinical, 72.7% IHC-B-clinical, 5.3% IHC-HER2-clinical and 15.1% triple negative cancer (TNC). Typing using the PAM50 gave 19.3% luminal-A, 32.5% luminal-B, 23.5% HER2-enriched and 24.6% basal-like. The basal-like and TNC had the highest concordance, while the luminal-A and IHC-A group had the lowest concordance. By altering the cutoff for Ki67, and realigning the HER2/ER/PR-positive patients to IHC-HER2, we improved concordance with the intrinsic subtypes.
Conclusion
We suggest that the Ki67 be changed to a cutoff of 20–25% in our population to better reflect the luminal subtype classifications. This change would inform treatment options for breast cancer patients in settings where genomic assays are unaffordable.
Similar content being viewed by others
Avoid common mistakes on your manuscript.
Introduction
Breast cancer is the most commonly diagnosed cancer among South African women accounting for 27.1% of all cancers diagnosed in these women [1]. Breast cancer diagnoses on the African continent have been steadily increasing over the past decades, attributed to longer lifespans and changes in lifestyle associated with westernization. In Africa, mortality rates are higher than in Europe and the United States, largely due to late stage at diagnosis and fewer treatment options [2, 3]. Breast cancer is a heterogeneous disease, differing in gene expression patterns, growth rates, responses to treatment and clinical outcomes.
Breast tumors can be subtyped by immunohistochemistry (IHC) which investigates the expression of four biomarkers: estrogen receptor (ER), progesterone receptor (PR), human epidermal growth factor receptor 2 (HER2/neu) and a marker of proliferation, Ki67. These markers distinguish ER-positive A-like, ER-positive B-like; HER2-enriched and triple negative (TNC) tumors (Table 1) [4,5,6]. Analysis of expression of the hormone receptors (ER and PR) is a semi-quantitative method based on the Allred Score [7,8,9].
The proliferation marker Ki67 is used to distinguish between the luminal subtypes [10, 11] and was adopted as a marker by the St Gallen International Consensus on Breast Cancer [5]. Ki67 was introduced as a diagnostic marker in South Africa in 2013 and is indicative of proliferation if Ki67 expression is ≥ 14% [5, 10]. However, the optimal Ki67 cut off value to distinguish luminal A-like tumors from luminal B-like tumors remains controversial due to uncertainty about how to classify tumors with intermediate (10–30%) Ki67 levels [12]. The 2015 St Gallen’s suggested a cutoff of 20–29% be used to distinguish A-like and B-like subtypes, along with clinical validation [13]. In addition, IHC for Ki67 analysis lacks reproducibility across laboratories [14]. Immunohistochemical results can be affected by the duration of fixation, type of fixative used, speed of assay and completeness of dehydration [15]. Moreover, the assessment is subject to interpretation by the histopathologist. In South Africa, the Department of Health 2018 recommendations are to use a Ki67 cutoff of 14% [16], although there is ongoing debate to the best cutoff of Ki67 to distinguish between luminal subtypes [17]. Ki67 cutoffs of both 14% and 20% are currently used at different centers.
The last decade has seen the development of many commercialized multigene tests to guide treatment and provide prognostic information for patients with breast cancer. The PAM50/ Prosigna assay has a 50-gene signature that groups tumors into intrinsic molecular subtypes luminal-A, luminal-B, HER2-enriched and basal-like [18]. The PAM50 assay is less subjective than the IHC-based techniques, but is much more expensive and labor intensive than IHC. In South African public hospitals, IHC continues to be used for clinical subtyping because of its lower cost.
A recent study from South Africa found that 64.9% of patients were diagnosed by IHC4 as B-like, 15.3% as TNC, 13.8% as A-like, and 6.0% as HER2-enriched [19]. An earlier country-wide study, found that black South African women had higher levels of ER-negative and PR-negative tumors than women of European, South Asian or admixture heritage, but did not have significantly different HER2 levels [15]. More recently, a study showed that white South African women had similar IHC profiles to European women and white American women, with more aggressive subtypes predominant in young women and less aggressive subtypes in older women, whereas black South African women did not have substantial profile changes according to age [20].
This study examines the concordance between PAM50 molecular subtyping assigned and the IHC results currently used for the management of breast cancer diagnosed within the South African Public Health System, focusing on varying Ki67 cutoffs. The data generated should help to inform cutoff values for IHC and may lead to better management of breast cancer in South Africa and other settings where genomic subtyping is unaffordable.
Methods
Study participants
The South African Breast Cancer and HIV Outcomes (SABCHO) cohort [21] studied patients recruited at the breast clinic of Chris Hani Baragwanath Academic Hospital (CHBAH), Soweto, South Africa. Participants were consenting women with biopsy-confirmed breast cancer who self-identified as Black African. Exclusion criteria were age < 18 years or current pregnancy. Clinical staging was according to the American Joint Committee on Cancer (AJCC) system [22]. The study was approved by the Human Research Ethics Committee (Medical) at the University of the Witwatersrand (M161116).
IHC classification of tumors
Histopathological characteristics for 384 patients, obtained from the National Health Laboratory Service (NHLS), included histological type, tumor grade, ER, PR, HER2 scoring and Ki67. All tissues for this study were processed at CHBAH NHLS Laboratory, following College of American Pathologist guidelines. Immunostaining was performed on the Benchmark XT automatic platform. The tumors were classified according to the St Gallen’s Guidelines [5, 13, 23]. The Allred score was used to determine ER/PR status, with a value of 0–2 considered negative, and 3–8 considered positive [8, 24, 25]. Tumors were HER2 positive if they scored 3 + by IHC, or 2 + by IHC with fluorescent in situ hybridization (FISH) confirmation. The Ki67 antibody used was 30–9 (Roche diagnostic, Ventana, USA), and multiple scorers at the same laboratory assessed the Ki67 stains. Percentage of proliferation was determined by visual estimation [17]. The cut-off for the proliferation marker Ki67 is unresolved. The multidisciplinary team at CHBAH uses a Ki67 score of 20% in conjunction with the Allred score, grade and age of patient as a cut off for chemotherapeutic treatment in HR positive breast cancers. We additionally explored cutoffs of 10%, 15%, 20%, 25% and 30%, because of the uncertainty surrounding those values for clinical decision making [12].
We assigned IHC used for clinical decision making as follows: Clin-A (HR + /HER2-/Ki67 ≤ 14%); Clin-B (HR + /HER2-/Ki67 > 14%, or HR + /HER2 + /Ki67 any); Clin-HER2 (HR-/HER2 + /Ki67 any); and Clin-TNC (HR-/HER2-/Ki67 any). The IHC subtyping surrogates were assigned as: A-like (HR + /HER2-/Ki67 ≤ 10%); A- or B-like (HR + /HER2-/10% < Ki67 ≤ 30%); B-like (HR + /HER2-/Ki67 > 30%); B/HER2-like (HR + /HER2 + /Ki67 any); HER2-like (HR-/HER2 + /Ki67 any); TNC (HR-/HER2-/Ki67 any). Both the clinical IHC subtypes as well as the IHC subtyping surrogates were compared with the PAM50 Intrinsic subtypes: luminal-A; luminal-B; HER2-enriched and basal-like (Table 1).
PAM50 intrinsic subtyping
FFPE blocks were cut into 5 µm serial sections; the area of tumor was identified and marked on an H&E section. If available, primary surgery blocks were preferentially chosen. If the surgery section was unavailable, or if the patient received neoadjuvant chemotherapy or radiation therapy prior to surgery, a biopsy section was used.
RNA was purified from the FFPE sections using the All Prep® DNA/RNA FFPE kit (Qiagen, Hilden, Germany). The RNA concentration was calculated using the optical density at 260 nm on the Nanodrop 2000™ spectrophotometer (Thermo Fisher Scientific, Waltham, MA). The extract was deemed suitable for further analysis if the concentration of RNA was greater than 12.5 ng/µl and the A260/280 ratio was 1.7–2.3. Following RNA extraction, 384 samples were of sufficient quantity and quality for molecular typing.
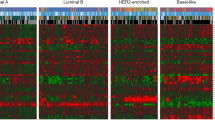
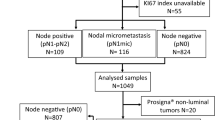
The PAM50 gene expression was measured on the nCounter SPRINT™ (Nanostring Technologies, Seattle, WA), as per the Prosigna® Breast Cancer Prognostic Gene signature assay Package insert [18]. (The 50 genes and 8 housekeeping genes are shown in supplementary Table S1 and an example of the resultant heat map are shown in supplementary Fig. S1.) nSOLVER 4.0 was used to retrieve the RCF files and perform QC analysis, background subtraction and normalization. Of the 384 samples, 378 passed QC and underwent further analysis; classification of intrinsic subtype was done at Nanostring (Seattle, WA). Quality control (QC) of the data was performed by NanoString Technologies, Inc. using their proprietary software, nSolver. For mRNA samples, as used in this study, QC is performed at a number of stages. Imaging QC flags samples if less than 75% of the imaging surface can be read. Binding density QC calculates the barcodes/micron2, samples with binding densities between 0.05 and 1.8 are usable with optimal binding densities being around 1.4 barcodes/micron2. The PAM50 panel includes both positive and negative controls which are assessed by geometric mean. Positive controls are synthetic RNA targets, spiked in at known concentrations, that are used to ensure proper hybridization and lack of RNase contamination in the samples and to establish limits of detection (the 0.5 fM positive control must be more than 2 standard deviations above the mean of the negative controls to pass QC). Positive controls are also used in normalization QC by generating scaling factors that must be between 0.3 and 3 to pass QC. Negative controls are probes for which no known target exists in biological samples and are used to establish background levels of detection.
Statistical analysis
Continuous variables were assessed for normality using the Shapiro-Wilks test. The data were described by mean ± standard deviation for normally distributed variables and median (interquartile range) for non-normally distributed variables. Categorical variables were described as frequencies and percentages. Statistical analyses were done using STATA v14.2 (College Station, Texas). Significance between the groups was determined using Pearson’s χ2 test or the Kruskall Wallis rank test, and post hoc analysis using Dunn’s Pairwise Comparison test. A p-value < 0.05 was considered significant. Agreement in subtype call between the IHC and PAM50 subtyping methods was assessed using the kappa statistic. To allow for comparable groups with this method, the IHC results were classified as follows: Clin-A (HR + /HER2-/Ki67 ≤ 14%), Clin-B (HR + /HER2-/Ki67 > 14%), Clin-HER2 (HR any/HER2 + /Ki67 any) and TNC (HR-/HER2-/Ki67 any).
Results
Characteristics of the study cohort
The clinicopathological characteristics are shown in Table 2. The mean age of study participants was 49.7 years. Most patients had stage II or III cancers, and were more likely to have grade-2 or -3 tumors between 20 and 50 mm (AJCC T2), with some nodal involvement.
The intrinsic subtyping distribution by the PAM50 assay was 19.3% luminal-A (n = 73), 32.5% luminal-B (n = 123), 23.5% HER2-enriched (n = 89) and 25.6% basal-like (n = 93) (Fig. 1a, Table 2). When classified by IHC, most patients (79.6%) were HR positive (with, or without, HER2) (Fig. 1b). Although the intrinsic subtypes (Fig. 1a) show roughly equal numbers of luminal-A (19.3%), luminal-B (32.5%), HER2-enriched (23.5%) and basal-like (24.6%) subtypes, the clinical IHC results show a massive predominance of Clin-B subtype (72.7%), and only 6.9% Clin-A, 5.3% Clin-HER2 and 15.1% Clin-TNC. High grade (3) Clin-A subtype, treated as Clin-B by the multidisciplinary team, only accounted for 0.53% (Table 2) of the total cohort, and did not meaningfully affect the concordance with the molecular subtypes.
Cohort subtypes by a Intrinsic subtyping by the PAM50 assay and b Clinical IHC subtypes. a The percentage distribution of intrinsic subtypes was luminal-B (32.5%, n = 123), basal-like (24.6%, n = 93), HER2-enriched (23.6%, n = 89), and luminal-A (19.3%, n = 73). However, using immunohistochemistry b as a surrogate for intrinsic subtypes, only 6.9% (n = 26) of the samples tested were categorized as Clin-A (ER/PR pos, HER2 neg and Ki67 ≥ 14%). Most of the samples (72.7%, n = 274) were Clin-B, i.e. ER/PR pos, HER2 neg, Ki67 > 14% or ER/PR pos, HER2 pos, any Ki67. A small minority (5.3%, n = 20) were Clin-HER2 (ER/PR neg, HER2 pos). The TNC (ER/PR neg, HER2 neg, Ki67 any) accounted for the remaining 15.1% (n = 57)
Comparison of immunohistochemistry and intrinsic subtypes
The luminal-B intrinsic subtype and the IHC B-like (Fig. 2a) were highly concordant. The intrinsic HER2-enriched showed the best concordance with the IHC B/HER2-like and the HR-/HER2-like (62.9% and 19.1%, respectively), while the intrinsic basal-like was most concordant with the IHC TNC (53.8%). Immunohistochemistry currently classifies the B/HER2-like as B-like tumors because they are HR positive but it may be more appropriate to classify these B/HER2-like tumors as HER2 positive tumors and to treat them accordingly. The intrinsic luminal-A subtype was not strongly associated with any one IHC subtype, raising questions about appropriate Ki67 cutoff values.
Comparison between immunohistochemical subtypes and molecular subtypes. a Frequency of immunohistochemical analysis subtypes (y-axis) within the PAM50 molecular defined tumor subtypes (x-axis). The luminal-A intrinsic subtype had the greatest spread of IHC types, with 28.8% IHC A-like, 28.8% IHC A- or B-like, 19.2% IHC B-like, 19.2% IHC B/HER2, 0% HER2-like (HR-/HER2 +) and 4.1% TNC. The luminal B intrinsic subtype was mainly B-like (50.8%), with 25.4% A- or B- like, and 20.5% B/HER2-like. The HER2-enriched intrinsic subtype was mainly B/HER2-like (62.9%), followed by HER2-like (HR-/HER2 + , 19.1%), and the basal-like was mainly TNC (53.8%) or B-like (33.3%). b Intrinsic subtype frequency (y-axis) concordance with each IHC-Analysis subgroup classification (x-axis). Most of the A-like (HR + /HER2-/Ki67 ≤ 10%) group had the luminal-A subtype (80.8%). The A- or B- like group (HR + /HER2-/10% < Ki67 ≤ 30%) had slightly more luminal-B (56.4%) then luminal-A (38.2%) subtypes. The B-like group (HR + /HER2-/Ki67 < 30%) had mainly luminal-B subtypes (53%). B/HER2-like (HR + /HER2 +) tumors were mainly HER2-enriched (54.9%), as was expected, while the HER2 group (HR-/HER2 +) was predominantly HER2-enriched (85%). The TNC group had overwhelming basal-like subtypes (87.7%)
By comparison, the IHC-like groups were well reflected by the intrinsic subtypes (Fig. 2b). The A-like group was mainly composed of luminal-A intrinsic subtypes; A- or B- like was primarily distributed between luminal-A (38.2%) and luminal-B (56.4%) intrinsic subtypes, and the IHC B-like was mainly comprised of luminal-B. The HR positive/HER2 + (B/HER2-like) group consisted mainly of the intrinsic HER2-enriched subtype, followed by the luminal-B subtype. The HR negative / HER2 positive (HER2-like) group was predominantly HER2-enriched, and the TNC group mainly basal-like, as expected.
Characteristics by intrinsic subtype
Expression of the proliferation marker, Ki67, was lowest in luminal-A tumors [20% (10–32.5%)], highest in the basal-like subtype [70% (50–80%)], and intermediate in the luminal-B [40% (30–55%)] and HER2-enriched [50% (40–62.5%)] subtypes, as expected (Table 3). Categorical analysis of Ki67 expression showed that the luminal-A tumors had the greatest spread, while close to 80% of the luminal-B tumors had Ki67 levels > 30%. The HER2-enriched and basal-like tumors expressed Ki67 at high values (over 30%), as expected. The Allred scores in luminal-A and luminal-B subtypes were predominantly high (scores of 7,8), while HER2-enriched subtypes had a greater spread of HR expression scores and basal-like subtypes were mainly negative or low scoring (Table 3).
Luminal-A (69.9%) and luminal-B (61.8%) subtypes were more likely to have lower T stages (T1 or T2), compared to HER2-enriched (36.0%) and basal-like (47.3%) subtypes. All intrinsic subtypes had T4 tumors, indicative of the late stage at presentation in this setting (Table 3). Tumors with a luminal subtype were more likely to be of lower grade (grade 1 or 2) than basal-like subtypes (75.0% grade 3). Histologically, only the luminal-A subtypes had a significant proportion of invasive lobular carcinomas (11.1%) and invasive mucinous carcinomas (6.9%). Age and nodal involvement were not associated with intrinsic subtype in this cohort (Table 3).
Comparisons of Ki67 cutoff levels
The kappa test was used to compare the classification of the luminal subtype using IHC and PAM50 based on Ki67 levels (Supplementary Table S2). The IHC groups were split into luminal-A and luminal-B subtypes using Ki67 cutoffs of 10%, 15%, 20%, 25% and 30% and the kappa statistic was used to compare these classifications to the subtypes assigned by the PAM50 analysis. The agreement between the methods ranged from 43 to 49%. The best concordance of the IHC and intrinsic subtypes, was when the cutoff was at 25% Ki67 (κ = 0.128, p = 0.003) and the worst at a cutoff of 10% (κ = 0.079, p = 0.033) (Supplementary Table S2). Thus, a Ki67 cutoff of 25% appears best for separating the luminal-A and -B subtypes in our setting. Using the 25% cutoff results in 15.5% IHC A-like and 37.3% B-like (Fig. 3b), closer in value to the intrinsic subtype proportions of luminal-A (19%) and luminal-B (32%) (Fig. 1a) than the current clinical cutoff of 14% (Fig. 1b). Moreover, when IHC HR + /HER2 + samples are separated from the Clin-B (Fig. 1b) into the B/HER2-like group (Fig. 3), the B-like group becomes smaller, but the B/HER2-like group (26.9%) and HER2-like group (5.3%) together, are more reflective of the HER2-enriched intrinsic subtype (Fig. 1b).
IHC Analysis subtypes with different Ki67 cutoff values to distinguish between IHC A-like and IHC B-like groups. IHC A-like with Ki67 ≥ 20% and IHC B-like with Ki67 < 20% is shown in (a); while IHC A-like with Ki67 ≥ 25% and IHC B-like with Ki67 < 25% is shown in (b). When the cutoff for Ki67 between IHC A-like and B-like is at 20% (a), 13.3% (n = 50) of the ER/PR pos, HER2 neg cohort is A-like and 39.5% (n = 148) is B-like. When the cutoff is at 25% (b), 15.5% (n = 58) of the ER/PR pos, HER2 neg cohort is A-like and 37.3% (n = 140) is B-like. When the ER/PR pos, HER2 pos (B/HER2-like) was classified separately from B-like group, it comprised 26.9% (n = 101) of the cohort. The HER2 (ER/PR neg, HER2 pos) group made up 5.3% (n = 20) of the cohort, and 14.9% (n = 56) of the cohort was triple negative (ER/PR neg, HER2 neg)
Discussion
The ability to diagnose breast cancer subtypes accurately and appropriately, fundamentally affects cancer treatment decisions. PAM50 is widely used for molecular diagnosis of breast cancer subtypes in high income countries (HICs) [26] because its results are reproducible and unaffected by inter- and intra-laboratory variability [27]. Within resource-constrained settings, IHC is used as a proxy for intrinsic subtypes because it is less expensive, the infrastructure to run IHC assays is widespread, and it requires less “hands-on” technical expertise than the PAM50 assay. We thus need accurate and population-specific information to assign proxies that optimize concordance calibration with the PAM50 intrinsic subtyping findings.
We found that the luminal-A intrinsic subtype had the greatest spread of IHC-analysis subgroups; the A-like IHC group was mainly composed of luminal-A subtype. This observation suggests that the currently used 14–20% Ki67 cutoff in South Africa may be too low. If the Ki67 cutoff were increased to 20–25%, the IHC A-like and B-like distribution would more accurately reflect the intrinsic subtypes. Subtyping strongly affects treatment options. Patients with luminal-A subtypes are likely to benefit from primary endocrine therapies in place of chemotherapy as first choice systemic treatment, whereas the benefits of chemotherapy to patients with luminal-B subtypes may offset chemotherapy side effects [28]. The ambiguity in the Ki67 cutoff is not unique to the South African public health care system. German guidelines state that primary invasive tumors that are HR + , HER2- are considered low risk if Ki67 ≤ 10%, high risk if ≥ 25%, and intermediate risk if 10–25% as Ki67 does not differentiate risk groups accurately in this range [12]. By contrast, the 14% cutoff was the best to distinguish between luminal-A and luminal-B in Spanish and Italian patients using Prosigna™ assays [29]. These results reinforced the original PCR findings of Cheang et al. [10] that the 14% cutoff was optimal. However, like Noske et al. [12], we observed better concordance at higher Ki67 levels.
In HICs, where most breast cancers are diagnosed in early stages, the ASCO recommendations [14] suggested that PAM50 could be used to inform chemotherapy decisions, much better than IHC in node negative luminal subtypes. Pu et al. [30] found that survival rates were consistently worse in the luminal-B subtype, irrespective of menopausal status. The 2019 St Gallen report recommended that patients with ER ≥ 1% receive endocrine therapy, although it might have limited benefits [28]. This recommendation is in line with the South African policy, which regards ER or PR ≥ 1% as hormone receptor positive [31]. The Allred score shows ER and/or PR expression is high in luminal-A and luminal-B subtypes, as expected. The PAM50 basal-like subtype was predominantly negative for the Allred score, but also had a portion of low (3,4) Allred scores. This second finding is interesting, as it may suggest that the Allred cutoff to distinguish between A-like, B-like IHC subtypes and TNC subtypes could be increased to an Allred score ≤ 4. A larger study is needed to confirm this.
Most tumors of the HER2-enriched luminal subtype are assigned to the B/HER-like IHC-analysis group. This finding is obvious when looking at the Allred score, where most of the HER2-enriched luminal subtypes had high HR positivity. While the multidisciplinary teams follow the St Gallen’s recommendations and treat HR + /HER2 + as Clin-B, the PAM50 intrinsic subtypes do not make this subtle distinction. In South African public health care, patients in this group received adjuvant endocrine therapy until 2019, when anti-HER2 therapies were introduced. A mere 19% of the HER2 enriched subtype would be HR negative and would not benefit from endocrine therapy.
Patient subtyping should be interpreted cautiously. Mistaking luminal-A patients for luminal-B may result in overtreatment with chemotherapy. Confusion of HER2 with luminal-B subtypes may result in under treatment by HER2 targeted therapy (e.g., trastuzumab) and/or overtreatment endocrine therapy [32]. Trastuzumab is expensive and inconsistently available in the South African public sector [33], so the option of using endocrine therapies if trastuzumab is unavailable would be an advantage for HER2 positive patients.
A Swedish cohort, [34] found 81–85% concordance between molecular luminal-A and IHC-A subtypes. However, 35–52% of their luminal-B intrinsic subtypes were classified as IHC-A. Ki67 distinguished between good and bad prognostic groups with node negative cancer, but its use is very controversial [34]. Lundgren et al. [35] found that concordance with luminal subtypes improved when histological grade was included. Well differentiated tumors (grade 1) tended to have low Ki67 levels [12]. Intermediate (grade 2) and poorly differentiated tumors (grade 3) had higher Ki67 levels and a wider range of Ki67 values [12]. In our study histological grades were generally high, so including grade with clinical IHC subtype had a negligible effect on concordance.
Previously, women of African ancestry were thought to have fewer hormone receptor positive breast cancers than women of European ancestry. West African women and African-American women appear more likely to have TNC cancers [36,37,38,39,40,41]. However, research has shown that most sub-Saharan Africans (South African, Kenyan, Sudanese) [15, 21, 42,43,44,45] have HR positive cancers. In our cohort, 79.5% were HR positive, and more likely to be B-like (i.e., HR positive, high Ki67), even when the cutoff of Ki67 is 30%. Such cancers are more aggressive and have a poorer prognosis than those classified as luminal-A or IHC A-like.
Because our study was part of a HIV outcome study, HIV positive and HIV negative cases were age matched within a 5 year band. Our study participants were therefore younger (49.9 years ± 11 years) than South African women with breast cancer on average. Younger patients are thought to have more clinically aggressive disease and poorer outcomes. Korean breast cancer patients are much more likely to be premenopausal than others [46], and this younger population shows poorer outcomes. Sub-Saharan Africa shows huge disparities in IHC subtyping [47]. In Uganda, breast cancer patients had mean age of 45, with IHC of 38% A or B; 5% B/HER2; 22% HER2 and 34% TNC [48]. Two separate Nigerian groups found very different IHC expression: a study in Ibadan, found 77.6% A or B; 2.6% B/HER2; 4% HER2 and 15.8% TNC [49]; while a different study in Lagos found 38% HR pos; 18.3% HER2 pos and 47.4% TNC [50]. Patients in Mozambique [51], had IHC of 51% A or B; 24% HER2 pos and 25% TNC; and Angola reported 25.7% A-like; 19.3% B-like; 7.9% B/HER2; 15.7% HER2-like and 31.4% TNC [52]; while in Zimbabwe, the IHC was 68% HR positive and 17% TNC [53]. Work on 985 participants in South Africa showed 13.8% A-like; 43.9% B-like, 19.0% B/HER2; 6.0% HER2-like and 15.3% TNC, although this work included individuals of different ethnicities [19]. Recent work in South Africa [20] found that black South Africans had expression of about 49–53% HR + /HER2- (A- or B-like), 13–18% HR + /HER2 + (B/HER2-like), 7–12% HR-/HER2 + and 23–27% TNC, regardless of age. By comparison, South African whites had 30–65% HR + /HER2- (A- or B-like), 9–29% HR + /HER2 + , 4–13% HR-/HER2 + and 14–29% TNC. White women under 40 had higher expression of the more aggressive TNC and HER2 tumors, while women over 60 had more A-like and B-like tumors. Our results, with exclusively black participants, did not show differences in between the distribution of subtypes with age, which is consistent with the results found by Achilonu et al. [20].
Limitations of this study include the small sample size and lower age of participants. This may have artificially increased the proportion of HER2 positive tumors. However, these limitations may have had reduced impact on the main focus of this study; which was the discordance between PAM50 intrinsic subtyping and IHC surrogates.
Our study is, as far as we know, the first to compare IHC with PAM50 in black southern African women. Most of our study participants had hormone receptor positive breast cancer, and even tumors with the HER2-enriched subtype were more likely to be HR positive than HR negative. PAM50 is widely used for breast cancer subtyping, with IHC often used in resource constrained settings. The cost and labor of the PAM50 method make it prohibitive for the South African public health care sector and its inability to distinguish between HER2-positive B-subtypes and HR negative/HER2 positive subtypes must also give pause. We found the lowest concordance between molecular and IHC subtyping for the luminal-A group and recommend raising the cutoff for Ki67 to 20–25% to distinguish between A-like and B-like tumors, to better reflect the luminal subtypes.
Data availability
Data are available upon reasonable request.
Abbreviations
- AJCC:
-
American Joint Committee on Cancer
- CHBAH:
-
Chris Hani Baragwanath Academic Hospital
- ER:
-
Estrogen receptor
- FFPE:
-
Formalin-fixed paraffin embedded
- FISH:
-
Fluorescent in situ hybridization
- HER2:
-
Human epidermal growth factor receptor 2
- HIC:
-
High-income countries
- HR:
-
Hormone receptor
- IHC:
-
Immunohistochemistry
- Neg:
-
Negative
- Pos:
-
Positive
- PR:
-
Progesterone receptor
- SABCHO:
-
South African Breast Cancer and HIV Outcomes
- TNC:
-
Triple negative breast cancer
References
Ferlay J, Ervik M, Lam F, Colombet M, Mery L, Piñeros M, et al. (2020) Global cancer observatory: cancer today. Lyon, France: International Agency for Research on Cancer. No Title. https://Gco.iarc.fr/Today/
Stefan DC (2015) Cancer care in Africa: an overview of resources. J Glob Oncol 1:30–36. https://doi.org/10.1200/jgo.2015.000406
Anyigba CA, Awandare GA, Paemka L (2021) Breast cancer in sub-Saharan Africa: the current state and uncertain future. Exp Biol Med 246:1377–1387. https://doi.org/10.1177/15353702211006047
Perou CM, Sørlie T, Eisen MB, van de Rijn M, Jeffrey SS, Rees CA et al (2000) Molecular portraits of human breast tumours. Nature 406:747–752. https://doi.org/10.1038/35021093
Goldhirsch A, Wood WC, Coates AS, Gelber RD, Thurlimann B, Senn HJ (2011) Strategies for subtypes-dealing with the diversity of breast cancer: highlights of the St Gallen international expert consensus on the primary therapy of early breast cancer 2011. Ann Oncol 22:1736–1747. https://doi.org/10.1093/annonc/mdr304
Viale G (2012) The current state of breast cancer classification. Ann Oncol 23:x207–x210. https://doi.org/10.1093/annonc/mds326
Allred D, Harvey J, Berardo M, Clark G (1998) Prognostic and predictive factors in breast cancer by immunohistochemical analysis. Mod Pathol 11:155–168
Allred DC (2010) Issues and updates: evaluating estrogen receptor-α, progesterone receptor, and HER2 in breast cancer. Mod Pathol 23:S52–S59. https://doi.org/10.1038/modpathol.2010.55
Shousha S (2008) Oestrogen receptor status of breast carcinoma: Allred/H score conversion table. Histopathology 53:346–347. https://doi.org/10.1111/j.1365-2559.2008.03075.x
Cheang MCU, Chia SK, Voduc D, Gao D, Leung S, Snider J et al (2009) Ki67 index, HER2 status, and prognosis of patients with luminal B breast cancer. J Natl Cancer Inst 101:736–750. https://doi.org/10.1093/jnci/djp082
Dowsett M, Nielsen TO, A’Hern R, Bartlett J, Coombes RC, Cuzick J et al (2011) Assessment of Ki67 in breast cancer: recommendations from the international Ki67 in breast cancer working Group. J Natl Cancer Inst 103:1656–1664. https://doi.org/10.1093/jnci/djr393
Noske A, Anders S-I, Ettl J, Hapfelmeier A, Steiger K, Specht K et al (2020) Risk stratification in luminal-type breast cancer: Comparison of Ki-67 with EndoPredict test results. Breast 49:101–107. https://doi.org/10.1016/j.breast.2019.11.004
Coates AS, Winer EP, Goldhirsch A, Gelber RD, Gnant M, Piccart-Gebhart MJ et al (2015) Tailoring therapies-improving the management of early breast cancer: St Gallen international expert consensus on the primary therapy of early breast cancer 2015. Ann Oncol 26:1533–1546. https://doi.org/10.1093/annonc/mdv221
Harris LN, Ismaila N, McShane LM, Andre F, Collyar DE, Gonzalez-Angulo AM et al (2016) Use of biomarkers to guide decisions on adjuvant systemic therapy for women with early-stage invasive breast cancer: American Society of clinical Oncology clinical practice guideline. J Clin Oncol 34:1134–1150. https://doi.org/10.1200/JCO.2015.65.2289
Dickens C, Duarte R, Zietsman A, Cubasch H, Kellett P, Schuz J et al (2014) Racial comparison of receptor-defined breast cancer in Southern African women: Subtype prevalence and age—incidence analysis of nationwide cancer registry data. Cancer Epidemiol Biomarkers Prev 23:2311–2321. https://doi.org/10.1158/1055-9965.EPI-14-0603
Department of Health Republic of South Africa (2018) Clinical guidelines for breast cancer. Control Manage: 1–123.
Van Den Berg EJ, Duarte R, Dickens C, Joffe M, Mohanlal R (2021) Ki67 Immunohistochemistry quantification in breast carcinoma: a comparison of visual estimation, counting, and ImmunoRatio. Appl Immunohistochem Mol Morphol 29:105–111. https://doi.org/10.1097/PAI.0000000000000864
Prosigna Insert (2015) Prosigna ® Breast cancer prognostic gene signature assay: 1–18.
Phakathi B, Cubasch H, Nietz S, Dickens C, Dix-Peek T, Joffe M et al (2019) Clinico-pathological characteristics among South African women with breast cancer receiving anti-retroviral therapy for HIV. Breast 43:123–129. https://doi.org/10.1016/j.breast.2018.12.005
Achilonu OJ, Singh E, Nimako G, Eijkemans RMJC, Musenge E (2022) Rule-based information extraction from free-text pathology reports reveals trends in South african female breast cancer molecular subtypes and Ki67 expression. Biomed Res Int 2022:1–17. https://doi.org/10.1155/2022/6157861
Cubasch H, Ruff P, Joffe M, Norris S, Chirwa T, Nietz S et al (2017) South African breast cancer and HIV outcomes study: methods and baseline assessment. J Glob Oncol 3:114–124. https://doi.org/10.1200/JGO.2015.002675
Amin MB, Edge S, Greene F, Byrd DR, Brookland RK, Washington MK et al (eds) (2017) AJCC cancer staging manual, 8th edn. Springer International Publishing, American Joint Commission on Cancer
Harbeck N, Thomssen C, Gnant M, St. Gallen (2013) Brief preliminary summary of the consensus discussion. Breast Care 2013(8):102–109. https://doi.org/10.1159/000351193
Harvey J, Clark G, Osborne C, Allred D (1999) Estrogen receptor status by immunohistochemistry is superior to the ligand-binding assay for predicting response to adjuvant endocrine therapy in breast cancer. J Clin Oncol 17:1474–1481. https://doi.org/10.1200/JCO.1999.17.5.1474
Fitzgibbons PL, Dillon DA, Alsabeh R, Berman MA, Hayes DF, Hicks DG et al (2014) Template for reporting results of biomarker testing of specimens from patients with carcinoma of the breast. Arch Pathol Lab Med 138:595–601. https://doi.org/10.5858/arpa.2013-0566-CP
Bastien RRL, Rodríguez-Lescure Á, Ebbert MTW, Prat A, Munárriz B, Rowe L et al (2012) PAM50 breast cancer subtyping by RT-qPCR and concordance with standard clinical molecular markers. BMC Med Genomics 5:44. https://doi.org/10.1186/1755-8794-5-44
Nielsen T, Wallden B, Schaper C, Ferree S, Liu S, Gao D et al (2014) Analytical validation of the PAM50-based prosigna breast cancer prognostic gene signature assay and nCounter analysis system using formalin-fixed paraffin-embedded breast tumor specimens. BMC Cancer 14:177. https://doi.org/10.1186/1471-2407-14-177
Burstein HJ, Curigliano G, Loibl S, Dubsky P, Gnant M, Poortmans P et al (2019) Estimating the benefits of therapy for early-stage breast cancer: the St. Gallen International Consensus Guidelines for the primary therapy of early breast cancer 2019. Ann Oncol 30:1541–1557. https://doi.org/10.1093/annonc/mdz235
Fernandez-Martinez A, Pascual T, Perrone G, Morales S, de La Haba J, González-Rivera M et al (2017) Limitations in predicting PAM50 intrinsic subtype and risk of relapse score with Ki67 in estrogen receptor-positive HER2- negative breast cancer. Oncotarget 8:21930–21937. https://doi.org/10.18632/oncotarget.15748
Pu M, Messer K, Davies SR, Vickery TL, Pittman E, Parker BA et al (2020) Research-based PAM50 signature and long-term breast cancer survival. Breast Cancer Res Treat 179:197–206. https://doi.org/10.1007/s10549-019-05446-y
Department of Health Republic of South Africa (2017) Breast Cancer Control Policy.
Paquet ER, Hallett MT (2015) Absolute assignment of breast cancer intrinsic molecular subtype. J Natl Cancer Inst 107:1–9. https://doi.org/10.1093/jnci/dju357
Wiseman RJ, Riddin J, Jugathpal J, Parrish AG, Ruff P, Blockman M (2020) Adjuvant trastuzumab in early HER2-positive breast cancer: journeying towards the optimal duration of therapy in South Africa. South African Med J 110:271–273. https://doi.org/10.7196/SAMJ.2020.V110I4.14621
Robertson S, Stålhammar G, Darai-Ramqvist E, Rantalainen M, Tobin NP, Bergh J et al (2018) Prognostic value of Ki67 analysed by cytology or histology in primary breast cancer. J Clin Pathol 71:787–794. https://doi.org/10.1136/jclinpath-2017-204976
Lundgren C, Bendahl PO, Borg Å, Ehinger A, Hegardt C, Larsson C et al (2019) Agreement between molecular subtyping and surrogate subtype classification: a contemporary population-based study of ER-positive/HER2-negative primary breast cancer. Breast Cancer Res Treat 178:459–467. https://doi.org/10.1007/s10549-019-05378-7
Huo D, Hu H, Rhie SK, Gamazon ER, Cherniack AD, Liu J et al (2017) Comparison of breast cancer molecular features and survival by African and European ancestry in the cancer genome atlas. JAMA Oncol 3:1654–1662. https://doi.org/10.1001/jamaoncol.2017.0595
Parada H, Sun X, Fleming JM, Williams-DeVane CLR, Kirk EL, Olsson LT et al (2017) Race-associated biological differences among luminal A and basal-like breast cancers in the Carolina breast cancer study. Breast Cancer Res 19:1–9. https://doi.org/10.1186/s13058-017-0914-6
Troester MA, Sun X, Allott EH, Geradts J, Cohen SM, Tse CK et al (2017) Racial differences in PAM50 subtypes in the Carolina breast cancer study. J Natl Cancer Inst 110:1–7. https://doi.org/10.1093/jnci/djx135
Ping J, Guo X, Ye F, Long J, Lipworth L, Cai Q et al (2021) Differences in gene-expression profiles in breast cancer between African and European-ancestry women. Carcinogenesis 41:887–893. https://doi.org/10.1093/CARCIN/BGAA035
Nwagu GC, Bhattarai S, Swahn M, Ahmed S, Aneja R (2021) Prevalence and mortality of triple-negative breast cancer in West Africa: biologic and sociocultural factors. JCO Glob Oncol. https://doi.org/10.1200/go.21.00082
Sung H, DeSantis CE, Fedewa SA, Kantelhardt EJ, Jemal A (2019) Breast cancer subtypes among Eastern-African–born black women and other black women in the United States. Cancer 125:3401–3411. https://doi.org/10.1002/cncr.32293
Awadelkarim KD, Elhaj A, Aceto G, Mariani-Costantini R, Abdalla EE (2012) Hereditary breast cancer in sub-saharan Africa. Curr Womens Health Rev 8:44–54. https://doi.org/10.2174/157340412799079219
McCormack VA, Joffe M, van den Berg E, Broeze N, Silva IDS, Romieu I et al (2013) Breast cancer receptor status and stage at diagnosis in over 1,200 consecutive public hospital patients in Soweto, South Africa: a case series. Breast Cancer Res 15:R84. https://doi.org/10.1186/bcr3478
Sayed S, Moloo Z, Wasike R, Bird P, Oigara R, Govender D et al (2014) Is breast cancer from Sub Saharan Africa truly receptor poor? Prevalence of ER/PR/HER2 in breast cancer from Kenya. Breast 23:591–596. https://doi.org/10.1016/j.breast.2014.06.006
Popli P, Gutterman EM, Omene C, Ganesan S, Mills D, Marlink R (2021) Receptor-defined breast cancer in five East African countries and its implications for treatment: systematic review and meta-analysis. JCO Glob Oncol. https://doi.org/10.1200/go.20.00398
Kim HK, Park KH, Kim Y, Park SE, Lee HS, Lim SW et al (2019) Discordance of the PAM50 intrinsic subtypes compared with immunohistochemistry-based surrogate in breast cancer patients: Potential implication of genomic alterations of discordance. Cancer Res Treat 51:737–747. https://doi.org/10.4143/crt.2018.342
Vanderpuye V, Grover S, Hammad N, Prabhakar P, Simonds H, Olopade F et al (2017) An update on the management of breast cancer in Africa. Infect Agent Cancer 12:1–12. https://doi.org/10.1186/s13027-017-0124-y
Galukande M, Wabinga H, Mirembe F, Karamagi C, Asea A (2014) Molecular breast cancer subtypes prevalence in an indigenous Sub Saharan African population. Pan Afr Med J 17:249. https://doi.org/10.11604/pamj.2014.17.249.330
Adebamowo CA, Famooto A, Ogundiran TO, Aniagwu T, Nkwodimmah C, Akang EE (2008) Immunohistochemical and molecular subtypes of breast cancer in Nigeria. Breast Cancer Res Treat 110:183–188. https://doi.org/10.1007/s10549-007-9694-5
Adeniji AA, Dawodu OO, Habeebu MY, Oyekan AO, Bashir MA, Martin MG et al (2020) Distribution of breast cancer subtypes among Nigerian women and correlation to the risk factors and clinicopathological characteristics. World J Oncol 11:165–172. https://doi.org/10.14740/wjon1303
Brandão M, Guisseve A, Bata G, Alberto M, Ferro J, Garcia C et al (2020) Breast cancer subtypes: Implications for the treatment and survival of patients in Africa—a prospective cohort study from Mozambique. ESMO Open 5:1–13. https://doi.org/10.1136/esmoopen-2020-000829
Miguel F, Lopes LV, Ferreira E, Ribas E, Pelaez AF, Leal C et al (2017) Breast cancer in Angola, molecular subtypes: a first glance. Ecancermedicalscience 11:1–10. https://doi.org/10.3332/ecancer.2017.763
Elmore SNC, Mushonga M, Iyer HS, Kanda C, Chibonda S, Chipidza F et al (2021) Breast cancer in Zimbabwe: patterns of care and correlates of adherence in a national referral hospital radiotherapy center cohort from 2014 to 2018. Cancer Med 10:3489–3498. https://doi.org/10.1002/cam4.3764
Acknowledgements
Special thanks to the patients attending the Batho Pele Breast clinic at Chris Hani Baragwanath Hospital for their willingness to be part of the study. Many thanks to the staff at the Batho Pele Clinic for their care and support of this project and to the staff at NHLS for IHC records and FFPE samples. We would like to thank Dr Briana M. Hudson at Nanostring for assigning intrinsic subtypes, and Dr Eva Kantelhardt and the team at Univeritätsklinikum Halle, Halle, Germany, who generously allowed TDP to work in their lab and gave advice on the process of PAM50 microarray before we started the project. RD wishes to thank Prof Valcárcel at the Centre for Genomic Regulation, Barcelona, for his support and mentorship as part of the Mujeres Por África scholarship programme, whose generous funding allowed a Fellowship placement in the Valcárcel Lab.
Funding
Open access funding provided by University of the Witwatersrand. This study received support from the NIH of the National Cancer Institute (Grant no: 01-CA192627 and P30-CA136696) to Prof. Jacobson, Dr. Joffe, Prof. Neugut, Prof. Ruff; University of the Witwatersrand/ South African Medical Research Council Common Epithelial Cancer Research Center Grant (CERC) to Prof. Ruff; and a South African National Research Foundation major equipment grant (105646) to Prof. Duarte.
Author information
Authors and Affiliations
Contributions
Concept design RD, TDP, BP; Collecting patient data MJ, HC; Histology EVB; Analysis and interpretation of the IHC and PAM50 data TDP, BP, TA, RD, CD; Clinical perspective MJ, HC, PR, AN, JJ, BP; Manuscript primarily written by TDP, RD, BP, CD, TA with input from all other authors.
Corresponding author
Ethics declarations
Competing interest
Dr. Neugut has consulted for Otsuka Pharmaceuticals, GlaxoSmithKline, United Biosource Corp., Eisai, Hospira, and Value Analytics. He is a member of the Medical Advisory Board of EHE Intl. He receives research funding from Otsuka Pharmaceuticals. Dr. Ruff has received Research Funding from MSD (Inst), Janssen Oncology (Inst), Roche (Inst), AstraZeneca (Inst), Novartis (Inst), Pfizer (Inst) and travel, accommodations expenses from Merck Serono, MSD Oncology, Pfizer, Dr Reddy’s Laboratories, AstraZeneca, Roche. No other conflicts of interest were reported.
Ethical approval
All participants consented to take part in the SABCHO study, and use of FFPE samples used in this study and the study was approved by the Human Research Ethics Committee (Medical) at the University of the Witwatersrand, # 161116. The study was performed in accordance with the declaration of Helsinki.
Consent to publish
All patients gave informed consent for the publication of the results and clinical information. Patient information was deidentified before analysis.
Additional information
Publisher's Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Supplementary Information
Below is the link to the electronic supplementary material.
Rights and permissions
Open Access This article is licensed under a Creative Commons Attribution 4.0 International License, which permits use, sharing, adaptation, distribution and reproduction in any medium or format, as long as you give appropriate credit to the original author(s) and the source, provide a link to the Creative Commons licence, and indicate if changes were made. The images or other third party material in this article are included in the article's Creative Commons licence, unless indicated otherwise in a credit line to the material. If material is not included in the article's Creative Commons licence and your intended use is not permitted by statutory regulation or exceeds the permitted use, you will need to obtain permission directly from the copyright holder. To view a copy of this licence, visit http://creativecommons.org/licenses/by/4.0/.
About this article
Cite this article
Dix-Peek, T., Phakathi, B.P., van den Berg, E.J. et al. Discordance between PAM50 intrinsic subtyping and immunohistochemistry in South African women with breast cancer. Breast Cancer Res Treat 199, 1–12 (2023). https://doi.org/10.1007/s10549-023-06886-3
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s10549-023-06886-3