Abstract
Purpose
Compared to white women, Black women have increased risk of developing hypertensive diseases of pregnancy (HDOP) and have a higher incidence of aggressive breast cancer subtypes. Few studies of HDOP and breast cancer risk have included large numbers of Black women. This study examined the relation of HDOP to incidence of breast cancer overall and by estrogen receptor (ER) status in Black women.
Methods
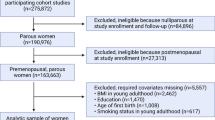
We followed 42,982 parous women in the Black Women’s Health Study, a nationwide prospective study of Black women. Multivariable Cox proportional hazards regression models were used to estimate hazard ratios (HRs) and 95% confidence intervals (CIs) to assess associations of self-reported HDOP, including preeclampsia and gestational hypertension, with breast cancer incidence overall and by ER subtype, adjusted for age and established breast cancer risk factors.
Results
Over 20 years of follow-up, we identified 2376 incident breast cancer cases. History of HDOP (11.7%) was not associated with breast cancer risk overall (HR 0.98; 95% CI 0.87, 1.11). HRs for invasive ER+ and ER– breast cancer were 1.11 (95% CI 0.93, 1.34) and 0.81 (95% CI 0.61, 1.07), respectively.
Conclusions
HDOP was not associated with risk of overall breast cancer in Black women. A suggestive inverse association with ER– breast cancer may reflect an anti-tumorigenic hormone profile in HDOP, but those results require confirmation in other studies.
Similar content being viewed by others
Data availability
The data underlying this article cannot be shared publicly to protect the confidentiality of of individuals who participated in the study. The data will be shared on reasonable request to the corresponding author.
References
Folk DM (2018) Hypertensive disorders of pregnancy: overview and current recommendations. J Midwifery & Women’s Health 63:289–300. https://doi.org/10.1111/jmwh.12725
Umesawa M, Kobashi G (2017) Epidemiology of hypertensive disorders in pregnancy: prevalence, risk factors, predictors and prognosis. Hypertens Res 40:213–220. https://doi.org/10.1038/hr.2016.126
Butwick AJ, Druzin ML, Shaw GM, Guo N (2020) Evaluation of US state-level variation in hypertensive disorders of pregnancy. JAMA Netw Open 3:e2018741. https://doi.org/10.1001/jamanetworkopen.2020.18741
Bello NA, Zhou H, Cheetham TC et al (2021) Prevalence of hypertension among pregnant women when using the 2017 American college of cardiology/American heart association blood pressure guidelines and association with maternal and fetal outcomes. JAMA Netw Open 4:e213808. https://doi.org/10.1001/jamanetworkopen.2021.3808
Fingar K, Mabry-Hernandez I, Ngo-Metzger Q, et al (2017) Delivery Hospitalizations Involving Preeclampsia and Eclampsia, 2005–2014. HCUP Statistical Brief. Agency for Healthcare Research and Quality, Rockville, MD
DeSantis CE, Fedewa SA, Goding Sauer A et al (2016) Breast cancer statistics, 2015 Convergence of incidence rates between black and white women: Breast Cancer Statistics 2015. CA A Cancer J Clinicians 66:31–42. https://doi.org/10.3322/caac.21320
DeSantis CE, Ma J, Gaudet MM et al (2019) Breast cancer statistics 2019. CA A Cancer J Clinicians 69:438–451. https://doi.org/10.3322/caac.21583@10.1002/(ISSN)1097-0142.breastcancercollection
Siegel RL, Miller KD, Jemal A (2018) Cancer statistics, 2018: Cancer Statistics. CA Cancer J Clin 68:7–30. https://doi.org/10.3322/caac.21442
DeSantis CE, Jemal A (2019) Re: black–white breast cancer incidence trends: effects of ethnicity. J Nat Cancer Instit 111:99–100. https://doi.org/10.1093/jnci/djy162
Bejaimal SAD, Wu CF, Lowe J et al (2016) Short-term risk of cancer among women with previous gestational diabetes: a population-based study. Diabet Med 33:39–46. https://doi.org/10.1111/dme.12796
Brasky TM, Li Y, Jaworowicz DJ et al (2013) Pregnancy-related characteristics and breast cancer risk. Cancer Causes Control 24:1675–1685. https://doi.org/10.1007/s10552-013-0242-9
Innes KE, Byers TE (2004) First pregnancy characteristics and subsequent breast cancer risk among young women. Int J Cancer 112:306–311. https://doi.org/10.1002/ijc.20402
Kim JS, Kang EJ, Woo OH et al (2013) The relationship between preeclampsia, pregnancy-induced hypertension and maternal risk of breast cancer: a meta-analysis. Acta Oncol 52:1643–1648. https://doi.org/10.3109/0284186X.2012.750033
Behrens I, Basit S, Jensen A et al (2016) Hypertensive disorders of pregnancy and subsequent risk of solid cancer-A nationwide cohort study: Hypertensive disorders of pregnancy and solid cancer. Int J Cancer 139:58–64. https://doi.org/10.1002/ijc.30065
Cnattingius S (2005) Pregnancy characteristics and maternal risk of breast cancer. JAMA 294:2474. https://doi.org/10.1001/jama.294.19.2474
Troisi R, Doody DR, Mueller BA (2013) A linked-registry study of gestational factors and subsequent breast cancer risk in the mother. Cancer Epidemiol Biomarkers Prev 22:835–847. https://doi.org/10.1158/1055-9965.EPI-12-1375
Innes KE, Byers TE (1999) Preeclampsia and breast cancer risk. Epidemiology 10:722–732
Wright LB, Schoemaker MJ, Jones ME et al (2018) Breast cancer risk in relation to history of preeclampsia and hyperemesis gravidarum: Prospective analysis in the Generations Study. Int J Cancer 143:782–792. https://doi.org/10.1002/ijc.31364
Vatten LJ, Romundstad PR, Trichopoulos D, Skjærven R (2002) Pre-eclampsia in pregnancy and subsequent risk for breast cancer. Br J Cancer 87:971–973. https://doi.org/10.1038/sj.bjc.6600581
Yang H, He W, Eriksson M et al (2018) Inherited factors contribute to an inverse association between preeclampsia and breast cancer. Breast Cancer Res 20:6. https://doi.org/10.1186/s13058-017-0930-6
Pacheco NLP, Andersen A-MN, Kamper-Jørgensen M (2015) Preeclampsia and breast cancer: The influence of birth characteristics. The Breast 24:613–617. https://doi.org/10.1016/j.breast.2015.06.006
Opdahl S, Romundstad PR, Alsaker MDK, Vatten LJ (2012) Hypertensive diseases in pregnancy and breast cancer risk. Br J Cancer 107:176–182. https://doi.org/10.1038/bjc.2012.195
Hajiebrahimi M, Cnattingius S, Lambe M, Bahmanyar S (2016) Pregnancy history and risk of premenopausal breast cancer-a nested case-control study. Int J Epidemiol 45:816–824. https://doi.org/10.1093/ije/dyv293
Serrand C, Mura T, Fabbro-Peray P et al (2021) Assessment of all-cause cancer incidence among individuals with preeclampsia or eclampsia during first pregnancy. JAMA Netw Open 4:e2114486. https://doi.org/10.1001/jamanetworkopen.2021.14486
Troisi R, Bjørge T, Gissler M et al (2018) The role of pregnancy, perinatal factors and hormones in maternal cancer risk: a review of the evidence. J Intern Med 283:430–445. https://doi.org/10.1111/joim.12747
Troisi R, Gulbech Ording A, Grotmol T et al (2018) Pregnancy complications and subsequent breast cancer risk in the mother: a Nordic population-based case-control study. Int J Cancer 143:1904–1913. https://doi.org/10.1002/ijc.31600
Ma H, Henderson KD, Sullivan-Halley J et al (2010) Pregnancy-related factors and the risk of breast carcinoma in situ and invasive breast cancer among postmenopausal women in the California Teachers Study cohort. Breast Cancer Res 12:R35. https://doi.org/10.1186/bcr2589
Calderon-Margalit R, Friedlander Y, Yanetz R et al (2009) Preeclampsia and subsequent risk of cancer: update from the Jerusalem Perinatal Study. Am J Obstet Gynecol 200:63.e1–5. https://doi.org/10.1016/j.ajog.2008.06.057
Kang EJ, Seo JH, Kim LY et al (2016) Pregnancy-associated risk factors of postpartum breast cancer in korea: a nationwide health insurance database study. PLoS ONE 11:e0168469. https://doi.org/10.1371/journal.pone.0168469
Sun M, Fan Y, Hou Y, Fan Y (2018) Preeclampsia and maternal risk of breast cancer: a meta-analysis of cohort studies. J Matern Fetal Neonatal Med 31:2484–2491. https://doi.org/10.1080/14767058.2017.1342806
Paltiel O, Friedlander Y, Tiram E et al (2004) Cancer after pre-eclampsia: follow up of the Jerusalem perinatal study cohort. BMJ 328:919. https://doi.org/10.1136/bmj.38032.820451.7C
Lin L-T, Hu L-Y, Tang P-L et al (2017) Do racial differences exist in the association between pregnancy-induced hypertension and breast cancer risk? Hypertens Pregnancy 36:138–144. https://doi.org/10.1080/10641955.2016.1258411
Walfisch A, Kessous R, Davidson E et al (2015) Pre-eclampsia and Future Female Malignancy. Hypertens Pregnancy 34:456–463. https://doi.org/10.3109/10641955.2015.1071838
Rosenberg L, Adams-Campbell L (1972) The Black Women’s health study: a follow-up study for causes and preventions of illness. J Am Med Womens Assoc 50:56–58
Gillon TER, Pels A, von Dadelszen P et al (2014) Hypertensive disorders of pregnancy: a systematic review of international clinical practice guidelines. PLoS ONE 9:e113715. https://doi.org/10.1371/journal.pone.0113715
Bellamy L, Casas J-P, Hingorani AD, Williams DJ (2007) Pre-eclampsia and risk of cardiovascular disease and cancer in later life: systematic review and meta-analysis. BMJ 335:974. https://doi.org/10.1136/bmj.39335.385301.BE
Kamper-Jørgensen M, Gammill HS, Nelson JL (2018) Preeclampsia and scleroderma: a prospective nation-wide analysis. Acta Obstet Gynecol Scand 97:587–590. https://doi.org/10.1111/aogs.13296
Weissgerber TL, Mudd LM (2015) Preeclampsia and Diabetes. Curr Diab Rep 15:579. https://doi.org/10.1007/s11892-015-0579-4
S Ananth Karumanchi, Kee-Hak Kim, Phyllis August Preeclampsia: Pathogenesis. In: UpToDate. https://www.uptodate.com/contents/preeclampsia-pathogenesis. Accessed 22 Jul 2020
Shu C, Han S, Xu P et al (2021) Estrogen and preeclampsia: potential of estrogens as therapeutic agents in preeclampsia. DDDT 15:2543–2550. https://doi.org/10.2147/DDDT.S304316
Lan K-C, Lai Y-J, Cheng H-H et al (2020) Levels of sex steroid hormones and their receptors in women with preeclampsia. Reprod Biol Endocrinol 18:12. https://doi.org/10.1186/s12958-020-0569-5
Jobe SO, Tyler CT, Magness RR (2013) Aberrant synthesis, metabolism, and plasma accumulation of circulating estrogens and estrogen metabolites in preeclampsia implications for vascular dysfunction. Hypertension 61:480–487. https://doi.org/10.1161/HYPERTENSIONAHA.111.201624
Hertig A, Liere P, Chabbert-Buffet N et al (2010) Steroid profiling in preeclamptic women: evidence for aromatase deficiency. Am J Obstet Gynecol 203:477.e1-477.e9. https://doi.org/10.1016/j.ajog.2010.06.011
Wan J, Hu Z, Zeng K et al (2018) The reduction in circulating levels of estrogen and progesterone in women with preeclampsia. Pregnancy Hypertension 11:18–25. https://doi.org/10.1016/j.preghy.2017.12.003
Berkane N, Liere P, Oudinet J-P et al (2017) From Pregnancy to Preeclampsia: A Key Role for Estrogens. Endocr Rev 38:123–144. https://doi.org/10.1210/er.2016-1065
Hübinette A, Lichtenstein P, Brismar K et al (2003) Serum insulin-like growth factors in normal pregnancy and in pregnancies complicated by preeclampsia. Acta Obstet Gynecol Scand 82:1004–1009
Bando H, Weich HA, Brokelmann M et al (2005) Association between intratumoral free and total VEGF, soluble VEGFR-1, VEGFR-2 and prognosis in breast cancer. Br J Cancer 92:553–561. https://doi.org/10.1038/sj.bjc.6602374
Furuya M, Kurasawa K, Nagahama K et al (2011) Disrupted balance of angiogenic and antiangiogenic signalings in preeclampsia. J Pregnancy 2011:1–10. https://doi.org/10.1155/2011/123717
Harmon AC, Cornelius DC, Amaral LM et al (2016) The role of inflammation in the pathology of preeclampsia. Clin Sci 130:409–419. https://doi.org/10.1042/CS20150702
Chappell LC, Seed PT, Briley AL et al (1999) Effect of antioxidants on the occurrence of pre-eclampsia in women at increased risk: a randomised trial. The Lancet 354:810–816. https://doi.org/10.1016/S0140-6736(99)80010-5
Roberts J, Cooper D (2001) Pathogenesis and genetics of pre-eclampsia. The Lancet 357:53–56. https://doi.org/10.1016/S0140-6736(00)03577-7
Hubel CA, Roberts JM, Taylor RN et al (1989) Lipid peroxidation in pregnancy: New perspectives on preeclampsia. Am J Obstet Gynecol 161:1025–1034. https://doi.org/10.1016/0002-9378(89)90778-3
Lee JD, Cai Q, Shu XO, Nechuta SJ (2017) The role of biomarkers of oxidative stress in breast cancer risk and prognosis: a systematic review of the epidemiologic literature. Journal of Women’s Health 26:467–482. https://doi.org/10.1089/jwh.2016.5973
Redman CW (2005) Latest advances in understanding preeclampsia. Science 308:1592–1594. https://doi.org/10.1126/science.1111726
Boij R, Svensson J, Nilsson-Ekdahl K et al (2012) Biomarkers of coagulation, inflammation, and angiogenesis are independently associated with preeclampsia. Am J Reprod Immunol 68:258–270. https://doi.org/10.1111/j.1600-0897.2012.01158.x
Troisi R, Weiss HA, Hoover RN et al (1998) Pregnancy characteristics and maternal risk of breast cancer. Epidemiology 9:641–647
Troisi R, Innes KE, Roberts JM, Hoover RN (2007) Preeclampsia and maternal breast cancer risk by offspring gender: do elevated androgen concentrations play a role? Br J Cancer 97:688–690. https://doi.org/10.1038/sj.bjc.6603921
Terry MB, Perrin M, Salafia CM et al (2007) Preeclampsia, pregnancy-related hypertension, and breast cancer risk. Am J Epidemiol 165:1007–1014. https://doi.org/10.1093/aje/kwk105
Diehl CL, Brost BC, Hogan MC et al (2008) Preeclampsia as a risk factor for cardiovascular disease later in life: validation of a preeclampsia questionnaire. Am J Obstet Gynecol 198:e11–e13. https://doi.org/10.1016/j.ajog.2007.09.038
Dietz P, Bombard J, Mulready-Ward C et al (2014) Validation of self-reported maternal and infant health indicators in the pregnancy risk assessment monitoring system. Matern Child Health J 18:2489–2498. https://doi.org/10.1007/s10995-014-1487-y
Coolman M, de Groot CJM, Jaddoe VW et al (2010) Medical record validation of maternally reported history of preeclampsia. J Clin Epidemiol 63:932–937. https://doi.org/10.1016/j.jclinepi.2009.10.010
Carter EB, Stuart JJ, Farland LV et al (2015) Pregnancy complications as markers for subsequent maternal cardiovascular disease: validation of a maternal recall questionnaire. Journal of Women’s Health 24:702–712. https://doi.org/10.1089/jwh.2014.4953
Barton JR, O’Brien JM, Bergauer NK et al (2001) Mild gestational hypertension remote from term: Progression and outcome. Am J Obstet Gynecol 184:979–983. https://doi.org/10.1067/mob.2001.112905
Magee LA, von Dadelszen P, Singer J et al (2016) The CHIPS randomized controlled trial (Control of Hypertension in Pregnancy Study): is severe hypertension just an elevated blood Pressure? Hypertension 68:1153–1159. https://doi.org/10.1161/HYPERTENSIONAHA.116.07862
Brown MA, Magee LA, Kenny LC et al (2018) Hypertensive disorders of pregnancy: ISSHP classification, diagnosis, and management recommendations for international practice. Hypertension 72:24–43. https://doi.org/10.1161/HYPERTENSIONAHA.117.10803
Acknowledgements
Data on breast cancer pathology were obtained from several state cancer registries (AZ, CA, CO, CT, DE, DC, FL, GA, IL, IN, KY, LA, MD, MA, MI, NJ, NY, NC, OK, PA, SC, TN, TX, VA). The BWHS study protocol was approved by the Boston University Medical Campus Institutional Review Board (IRB) and by the IRBs of participating cancer registries as required. The content is solely the responsibility of the authors and does not necessarily represent the official views of the National Cancer Institute, the National Institutes of Health, or the state cancer registries. We thank participants and staff of the BWHS for their contributions. We would also like to thank Rinka Murakami for her assistance with the literature search.
Funding
This work was supported by the National Institutes of Health (CA058420, CA164974, and CA151135). Julie R. Palmer received support from the Susan G. Komen Foundation (SAC180086) and the Karin Grunebaum Cancer Research Foundation. Zahna Bigham received support from the Medical Scientist Training Program at Tufts University (T32 GM00844826) and the Susan G. Komen Foundation (GTDR15333918). Karen M. Freund received support from the American Cancer Society (# CRP-17–112-06-COUN) and the Susan G. Komen Foundation (GTDR15333918).
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
Conflict of interest
Karen M. Freund receives support from the American Cancer Society (# CRP-17–112-06-COUN) and the Susan G. Komen Foundation (GTDR15333918). She received a $1000 honorarium from the National Minority Quality Forum to support the work of the National Minority Quality Forum in developing a framework on addressing cancer health disparities in 2019, which was prior to initiation of the current research.
Ethical approval
All study procedures received approval by the Boston University Institutional Review Board.
Informed consent
Informed consent was obtained from all study participants.
Additional information
Publisher's Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Rights and permissions
About this article
Cite this article
Bigham, Z., Robles, Y., Freund, K.M. et al. Hypertensive diseases of pregnancy and risk of breast cancer in the Black Women’s Health Study. Breast Cancer Res Treat 194, 127–135 (2022). https://doi.org/10.1007/s10549-022-06606-3
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s10549-022-06606-3