Abstract
Purpose
Women with preeclampsia are more likely to deliver preterm. Reports of inverse associations between preeclampsia and breast cancer risk, and positive associations between preterm birth and breast cancer risk are difficult to reconcile. We investigated the co-occurrence of preeclampsia/gestational hypertension with preterm birth and breast cancer risk using data from the Premenopausal Breast Cancer Collaborative Group.
Methods
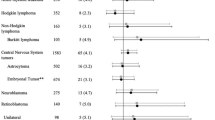
Across 6 cohorts, 3096 premenopausal breast cancers were diagnosed among 184,866 parous women. We estimated multivariable hazard ratios (HR) and 95% confidence intervals (CI) for premenopausal breast cancer risk using Cox proportional hazards regression.
Results
Overall, preterm birth was not associated (HR 1.02, 95% CI 0.92, 1.14), and preeclampsia was inversely associated (HR 0.86, 95% CI 0.76, 0.99), with premenopausal breast cancer risk. In stratified analyses using data from 3 cohorts, preterm birth associations with breast cancer risk were modified by hypertensive conditions in first pregnancies (P-interaction = 0.09). Preterm birth was positively associated with premenopausal breast cancer in strata of women with preeclampsia or gestational hypertension (HR 1.52, 95% CI: 1.06, 2.18), but not among women with normotensive pregnancy (HR = 1.09, 95% CI: 0.93, 1.28). When stratified by preterm birth, the inverse association with preeclampsia was more apparent, but not statistically different (P-interaction = 0.2), among women who did not deliver preterm (HR = 0.82, 95% CI 0.68, 1.00) than those who did (HR = 1.07, 95% CI 0.73, 1.56).
Conclusion
Findings support an overall inverse association of preeclampsia history with premenopausal breast cancer risk. Estimates for preterm birth and breast cancer may vary according to other conditions of pregnancy.


Similar content being viewed by others
Data availability
The data that support the findings of this study are not publicly available due to privacy or ethical restrictions. Study data may be shared upon reasonable request to senior authors.
Abbreviations
- BP:
-
Blood pressure
- BWHS:
-
Black Women’s Health Study
- CI:
-
Confidence interval
- ER:
-
Estrogen receptor
- GEN:
-
Generations Study
- HR:
-
Hazard ratio
- MCCS:
-
Melbourne Collaborative Cohort Study
- NHS2:
-
Nurses’ Health Study II
- RR:
-
Relative risk
- SIS:
-
Sister Study
- SWLS:
-
Swedish Women’s Lifestyle and Health Study
- UK:
-
United Kingdom
- USA:
-
United States of America
References
Roberts JM, Pearson GD, Cutler JA, Lindheimer MD, National Heart L, Blood I (2003) Summary of the NHLBI working group on research on hypertension during pregnancy. Hypertens Pregnancy 22(2):109–127
Folk DM (2018) Hypertensive disorders of pregnancy: overview and current recommendations. J Midwifery Womens Health 63(3):289–300
Ananth CV, Keyes KM, Wapner RJ (2013) Pre-eclampsia rates in the United States, 1980–2010: age-period-cohort analysis. BMJ 347:f6564
Wang F, Zhang W, Cheng W, Huo N, Zhang S (2021) Preeclampsia and cancer risk in women in later life: a systematic review and meta-analysis of cohort studies. Menopause 28(9):1070–1078
Nechuta S, Paneth N, Velie EM (2010) Pregnancy characteristics and maternal breast cancer risk: a review of the epidemiologic literature. Cancer Causes Control 21(7):967–989
Falk RT, Staff AC, Bradwin G, Karumanchi SA, Troisi R (2016) A prospective study of angiogenic markers and postmenopausal breast cancer risk in the prostate, lung, colorectal, and ovarian cancer screening trial. Cancer Causes Control 27(8):1009–1017
Vatten LJ (2009) Romundstad PlR, jenum PlA, eskild a: angiogenic balance in pregnancy and subsequent breast cancer risk and survival: a population study. Cancer Epidemiol Biomark Prev 18(7):2074–2078
Preterm Birth [https://www.who.int/news-room/fact-sheets/detail/preterm-birth]
Martin JAH BEO, J.K.: Births in the United States. In. Edited by Statistics NCfH. Hyattsville, MD; 2019.
Wright LB, Schoemaker MJ, Jones ME, Ashworth A, Swerdlow AJ (2018) Breast cancer risk in relation to history of preeclampsia and hyperemesis gravidarum: prospective analysis in the generations Study. Int J Cancer 143(4):782–792
Hajiebrahimi M, Cnattingius S, Lambe M, Bahmanyar S (2016) Pregnancy history and risk of premenopausal breast cancer-a nested case-control study. Int J Epidemiol 45(3):816–824
Hsieh CC, Wuu J, Lambe M, Trichopoulos D, Adami HO, Ekbom A (1999) Delivery of premature newborns and maternal breast-cancer risk. Lancet 353(9160):1239
Innes KE, Byers TE (2004) First pregnancy characteristics and subsequent breast cancer risk among young women. Int J Cancer 112(2):306–311
Melbye M, Wohlfahrt J, Andersen AM, Westergaard T, Andersen PK (1999) Preterm delivery and risk of breast cancer. Br J Cancer 80(3–4):609–613
Troisi R, Gulbech Ording A, Grotmol T, Glimelius I, Engeland A, Gissler M, Trabert B, Ekbom A, Madanat-Harjuoja L, Sorensen HT et al (2018) Pregnancy complications and subsequent breast cancer risk in the mother: a Nordic population-based case-control study. Int J Cancer 143(8):1904–1913
Vatten LJ, Romundstad PR, Trichopoulos D, Skjaerven R (2002) Pregnancy related protection against breast cancer depends on length of gestation. Br J Cancer 87(3):289–290
Cnattingius S, Torrang A, Ekbom A, Granath F, Petersson G, Lambe M (2005) Pregnancy characteristics and maternal risk of breast cancer. JAMA 294(19):2474–2480
Le Marchand L, Kolonel LN, Myers BC, Mi MP (1988) Birth characteristics of premenopausal women with breast cancer. Br J Cancer 57(4):437–439
Swerdlow AJ, Wright LB, Schoemaker MJ, Jones ME (2018) Maternal breast cancer risk in relation to birthweight and gestation of her offspring. Breast Cancer Res 20(1):110
Troisi R, Doody DR, Mueller BA (2013) A linked-registry study of gestational factors and subsequent breast cancer risk in the mother. Cancer Epidemiol Biomarkers Prev 22(5):835–847
Ardalan A, Bungum T (2016) Gestational age and the risk of maternal breast cancer: a population-based case-control study. Breast J 22(6):657–661
Kessous R, Walfisch A, Meirovitz M, Davidson E, Sergienko R, Sheiner E (2017) Preterm delivery and future maternal risk of female malignancies. Arch Gynecol Obstet 295(1):205–210
Polednak AP, Janerich DT (1983) Characteristics of first pregnancy in relation to early breast cancer. A case-control study J Reprod Med 28(5):314–318
Lapillonne H, Golsteyn RM, Lapillonne A (1999) Duration of pregnancy and risk of breast cancer. Lancet 353(9169):2075
Nichols HB, Schoemaker MJ, Wright LB, McGowan C, Brook MN, McClain KM, Jones ME, Adami HO, Agnoli C, Baglietto L et al (2017) The premenopausal breast cancer collaboration: a pooling project of studies participating in the national cancer institute cohort consortium. Cancer Epidemiol Biomarkers Prev 26(9):1360–1369
Roswall N, Sandin S, Adami HO, Weiderpass E (2017) Cohort profile: the Swedish women’s lifestyle and health cohort. Int J Epidemiol 46(2):e8
Swerdlow AJ, Jones ME, Schoemaker MJ, Hemming J, Thomas D, Williamson J, Ashworth A (2011) The breakthrough generations study: design of a long-term uk cohort study to investigate breast cancer aetiology. Br J Cancer 105(7):911–917
Giles GG, English DR (2002) The Melbourne collaborative cohort study. IARC Sci Publ 156:69–70
Colditz GA, Hankinson SE (2005) The nurses’ health study: lifestyle and health among women. Nat Rev Cancer 5(5):388–396
Sandler DP, Hodgson ME, Deming-Halverson SL, Juras PS, D’Aloisio AA, Suarez LM, Kleeberger CA, Shore DL, DeRoo LA, Taylor JA et al (2017) The sister study cohort: baseline methods and participant characteristics. Environ Health Perspect 125(12):127003
Rosenberg L, Adams-Campbell L, Palmer JR (1995) The black women’s health study: a follow-up study for causes and preventions of illness. J Am Med Womens Assoc (1972) 50(2):56–58
Milne RL, Fletcher AS, MacInnis RJ, Hodge AM, Hopkins AH, Bassett JK, Bruinsma FJ, Lynch BM, Dugue PA, Jayasekara H et al (2017) Cohort profile: the melbourne collaborative cohort study (health 2020). Int J Epidemiol 46(6):1757–1757i
Greenland S, Pearl J, Robins JM (1999) Causal diagrams for epidemiologic research. Epidemiology 10(1):37–48
Buse A (1982) The likelihood ratio, wald, and lagrange multiplier tests: an expository note. Am Stat 36(3):153–157
Schoenfeld D (1980) Chi-squared goodness-of-fit tests for the proportional hazards regression model. Biometrika 67(1):145–153
Harville DA (1977) Maximum likelihood approaches to variance component estimation and to related problems. J Am Stat Assoc 72(358):320–338
Laird NM, Ware JH (1982) Random-effects models for longitudinal data. Biometrics 38(4):963–974
Smith-Warner SA, Spiegelman D, Ritz J, Albanes D, Beeson WL, Bernstein L, Berrino F, van den Brandt PA, Buring JE, Cho E et al (2006) Methods for pooling results of epidemiologic studies: the pooling project of prospective studies of diet and cancer. Am J Epidemiol 163(11):1053–1064
Cochran WG (1954) The combination of estimates from different experiments. Biometrics 10(1):101–129
DerSimonian R, Laird N (1986) Meta-analysis in clinical trials. Control Clin Trials 7(3):177–188
Higgins J, Thompson S, Deeks J, Altman D (2002) Statistical heterogeneity in systematic reviews of clinical trials: a critical appraisal of guidelines and practice. J Health Serv Res Policy 7(1):51–61
Vatten LJ, Romundstad PR, Trichopoulos D, Skjaerven R (2002) Pre-eclampsia in pregnancy and subsequent risk for breast cancer. Br J Cancer 87(9):971–973
Opdahl S, Romundstad PR, Alsaker MD, Vatten LJ (2012) Hypertensive diseases in pregnancy and breast cancer risk. Br J Cancer 107(1):176–182
Pacheco NL, Andersen AM, Kamper-Jorgensen M (2015) Preeclampsia and breast cancer: the influence of birth characteristics. Breast 24(5):613–617
Schoemaker MJ, Nichols HB, Wright LB, Brook MN, Jones ME, O’Brien KM, Adami HO, Baglietto L, Bernstein L et al Premenopausal Breast Cancer Collaborative (2018) Association of body mass index and age with subsequent breast cancer risk in premenopausal women. JAMA Oncol 4(11):e181771
Levine RJ, Maynard SE, Qian C, Lim K-H, England LJ, Yu KF, Schisterman EF, Thadhani R, Sachs BP, Epstein FH et al (2004) Circulating angiogenic factors and the risk of preeclampsia. N Engl J Med 350(7):672–683
Valensise H, Vasapollo B, Gagliardi G, Novelli GP (2008) Early and late preeclampsia: two different maternal hemodynamic states in the latent phase of the disease. Hypertension 52(5):873–880
Bertrand KA, O’Brien KM, Wright LB, Palmer JR, Blot WJ, Eliassen AH, Rosenberg L, Sandin S, Tobias D, Weiderpass E et al (2020) Gestational diabetes and risk of breast cancer before after 55. Int J Epidemiol. https://doi.org/10.1093/ije/dyab165
Acknowledgements
The authors would like to thank all study participants, staff, and participating cancer registries. The Nurses' Health Study II thank study participants, staff, and the following state cancer registries: AL, AZ, AR, CA, CO, CT, DE, FL, GA, ID, IL, IA, IA, KY, LA, ME, MD, MA, MI, NE, NH, NJ, NY, NC, ND, OH, OK, OR, PA, RI, SC, TN, TX, VA, WA, and WY. The Black Women's Health Study obtained pathology data on breast cancer from state cancer registries in AZ, CA, CO, CT, DE, DC, FL, GA, IL, IN, KY, LA, MD, MA, MI, NJ, NY, NC, OK, PA, SC, TN, TX, and VA. The Melbourne Collaborative Cohort Study cases and their vital status were ascertained through the Victorian Cancer Registry and the Australian Institute of Health and Welfare, including the Australian Cancer Database. The authors assume full responsibility for analyses and interpretation of these data. They thank the National Cancer Institute Cohort Consortium for facilitating this collaboration.
Funding
Support for this research comes, in part, by the National Institutes of Health (R01CA204258; R01CA058420; U01CA164974; P01CA151135; U01CA176726; UM1CA186107; R01CA50385) and the Intramural Research Program of the National Institutes of Health, National Institute of Environmental Health Sciences (Z01 ES044005); the Avon Foundation (02–2014-080); the National Center for Advancing Translational Sciences (KL2-TR001109); the National Program of Cancer Registries of the Centers for Disease Control and Prevention and the Department of Energy; Breast Cancer Now and the United Kingdom National Health Service funding to the Royal Marsden/Institute of Cancer Research National Institute for Health Research Biomedical Research Centre; the Institute of Cancer Research (02–2014-080); Karolinska Institutet Distinguished Professor Award (2368/10–221); VicHealth, Cancer Council Victoria and the Australia National Health and Medical Research Council (209057, 396414, and 1074383); Breast Cancer Research Foundation (17–138); the Swedish Research Council and Swedish Cancer Foundation; The coordination of EPIC (the European Prospective Investigation into Cancer and Nutrition) is financially supported by the European Commission (DG-SANCO) and the International Agency for Research on Cancer. The national cohorts are supported by the Swedish Cancer Society, Swedish Research Council, and county councils of Skåne and Va¨ sterbotten (Sweden); and grant 14136 to European Prospective Study into Cancer and Nutrition (EPIC)–Norfolk and grants C570/A16491 and C8221/A19170 to EPIC-Oxford from Cancer Research UK and grant 1000143 to EPIC-Norfolk and MR/M012190/1 to EPIC-Oxford from the Medical Research Council (United Kingdom).
Author information
Authors and Affiliations
Contributions
The work reported in the paper has been performed by the authors, unless clearly specified in the text. HBN, DPS, AJS, and MJS contributed to study conceptualization, methodology, and supervision. HBN and MH conducted the formal analysis. HBN drafted the original manuscript, which was critically reviewed and approved by all authors.
Corresponding author
Ethics declarations
Competing interests
The authors have no relevant financial or non-financial interests to disclose.
Ethical approval
Individual study protocols were approved by the relevant institutional review boards and obtained informed consent from participants.
Additional information
Publisher's Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Supplementary Information
Below is the link to the electronic supplementary material.
Rights and permissions
Springer Nature or its licensor (e.g. a society or other partner) holds exclusive rights to this article under a publishing agreement with the author(s) or other rightsholder(s); author self-archiving of the accepted manuscript version of this article is solely governed by the terms of such publishing agreement and applicable law.
About this article
Cite this article
Nichols, H.B., House, M.G., Yarosh, R. et al. Hypertensive conditions of pregnancy, preterm birth, and premenopausal breast cancer risk: a premenopausal breast cancer collaborative group analysis. Breast Cancer Res Treat 199, 323–334 (2023). https://doi.org/10.1007/s10549-023-06903-5
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s10549-023-06903-5