Abstract
Breast cancer is the most common cancer diagnosed in women worldwide, with approximately 5–10% of cases attributed to high penetrance hereditary breast cancer (HBC) genes. The tremendous advances in precision oncology have broadened indications for germline genetic testing to guide both systemic and surgical treatment, with increasing demand for cancer genetic services. The HBC continuum of care includes (1) identification, access, and uptake of genetic counseling and testing; (2) the delivery of genetic counseling and testing services; and (3) initiation of guideline-adherent follow-up care and family communication of results. Challenges to delivering care on the HBC care continuum include factors such as access to services, cost, discrimination and bias, and lack of education and awareness, which can be mitigated through implementing a multi-level approach. This includes strategies such as increasing awareness and utilization of genetic counseling and testing, developing new methods to meet the growing demand for genetic services, and improving the uptake of follow-up care by increasing patient and provider awareness of the management recommendations.
Similar content being viewed by others
Introduction
Breast cancer is the most common cancer diagnosed in women worldwide, with high penetrance inherited cancer predisposing genes accounting for approximately 5–10% of cases [1, 2]. An additional 20% of cases are thought to be familial; thus, they not attributable to a single inherited high penetrance gene and include additional genetic contributors including moderate penetrance genes and polygenic inheritance [3,4,5]. The indications to test for hereditary breast cancer (HBC) have expanded to encompass testing to guide cancer treatment which in turn has further increased the demand for breast cancer risk assessment and testing services.
Breast cancer risk spans a continuum. Although no standard definition currently exists, for the purposes of this paper, genes considered to be highly penetrant are defined as > 4-fold risk (and generally 10–20 fold risk) and those considered moderately penetrant have a 2–4-fold risk of cancer [6, 7]. Prior studies suggest that the majority of HBC genes are attributed to the BRCA1 and BRCA2 (BRCA) [8]. There are also “non-BRCA” inherited breast cancer genes which include both high (e.g., PALB2, TP53, PTEN, and CDH1) [9] and moderate (e.g., ATM and CHEK2) penetrance genes [7]. Additionally, there are single nucleotide polymorphisms (SNPs) identified within or outside of genes, which individually impart < 2-fold risk, considered as ‘low penetrance’ [7], which in combination may be used to generate a polygenic risk score (PRS).
Delivery of hereditary breast cancer services across the care continuum
The delivery of services focused on HBC may be considered through the lens of a ‘care delivery continuum’ (as outlined in Fig. 1). This continuum includes (1) identification, access, and uptake of genetic counseling and testing; (2) the delivery of genetic counseling and testing services; and (3) initiation of guideline-adherent follow-up care and family communication of results, upon completion of risk assessment and testing.
Identification of individuals at risk for HBC
Identification of individuals with pathogenic or likely pathogenic (P/LP) variants in an HBC gene (often referred to as ‘gene carriers’) offers an opportunity to manage patients at increased risk for cancer through early detection, chemoprevention, and risk-reducing surgeries (Fig. 2) [10]. For example, individuals with a BRCA P/LP variant have a 60–70% lifetime risk of developing breast cancer [11], up to a 50% risk of developing a second primary breast cancer [12], and up to a 44% lifetime risk of developing ovarian cancer [11, 12]. Thus, identification of a P/LP variant in a HBC gene informs cancer risks, which then guides cancer risk management (as outlined in Fig. 2). Analogous to the BRCA genes, other HBC genes have specific ranges of lifetime cancer risks and corresponding management recommendations to mitigate these elevated risks [7]. Yet, despite meeting the national guidelines for genetic testing referral, few patients with breast cancer who meet guideline criteria for HBC testing are actually tested, with even lower rates among minority, rural, and underserved populations [2, 13,14,15,16,17,18,19,20,21,22,23]. Relatively higher genetic testing rates at academic centers [24, 25] are not reflective of the much lower national testing rates reported through administrative databases and registries [14, 18, 20]. In fact, a recent study based on national claims data reported that genetic testing rates were less than 20% in patients with breast or ovarian cancer who met national criteria for testing [14].
Genetic counseling and testing
The traditional model for cancer genetic risk assessment services for women with breast cancer has involved a pre-test genetic counseling session during which an evaluation is done and informed consent for testing is obtained, followed by a post-test genetic counseling session, during which results are disclosed and interpreted in the context of the personal and family history [7, 26]. Multiple professional organizations endorse the importance of genetic counseling in the context of genetic testing, with components of discussion items aligned across multiple professional organizations, including the National Comprehensive Cancer Network (NCCN), National Society of Genetic Counselors (NSGC), American Society of Clinical Oncology (ASCO), and the Commission on Cancer/National Accreditation Program for Breast Centers (CoC/NAPBC) [7, 26,27,28].
The plummeting cost of DNA sequencing in conjunction with expanding indications for genetic testing has led to increased demand for genetic services which has outpaced the supply of certified and credentialed genetics health professionals (GHPs) to provide these services [29]. A recent survey of genetic counselors across specialties reported that 54% perceived their current delivery model is inadequate to address the needs of their patients and 65% reported plans to change their model [30]. The national shortage of GHPs [31] coupled with limited access to GHPs in rural areas [32] and community oncology practices in many states [33] has resulted in the majority of genetic tests being ordered without the inclusion of a GHP. In fact, we and others have previously reported that the minority of breast cancer patients are tested through a GHP [34, 35]. Similar to our findings which showed that only 20% of young breast cancer survivors had genetic testing services provided by a GHP [34], another study showed that approximately 21% of patients who received genetic testing reported that a genetic counselor ordered their genetic test [35]. Yet there are insurance policies which mandate pre-test genetic counseling be conducted with involvement of a GHP, which may disproportionately reduce genetic testing rates among minority and underserved populations who have decreased access to genetic services [36, 37].
Moreover, the increasing use and decreasing cost of next-generation sequencing-based tests has shifted the paradigm toward use of multi-gene panel tests. This in turn has led to the option of testing for genes beyond the clinical indication based on personal or family history of cancer [38]; as well as inclusion of high and moderate penetrance genes, ‘preliminary evidence’ genes with uncertain or unproven cancer associations, and single nucleotide polymorphisms (SNPs) identified through genome wide association studies (GWAS) to generate a PRS. Given that data to generate PRS are based on existing data in Caucasian populations, risk predictions are also limited to this population and not standardized across labs [39]. In fact, a recent study of breast cancer patients reported that PRS did not improve risk prediction among women of African ancestry compared to European ancestry [40]. Moreover, accuracy to predict disease risk using data generated primarily from European GWAS has been reported to be about a quarter among Black patients [41].
With increasing numbers of genes clinically available for testing through multi-gene panels, there has been an upsurge of testing for genes of uncertain clinical utility and genes that may not be clinically indicated based on personal or family history thereby raising the complexity of pre-test genetic counseling [27]. Alongside these developments, the traditional pre-test genetic counseling model has continued to be refined for effective integration into clinical practice [27]. Furthermore, interpretation of results becomes increasingly complex as broad germline panels are ordered, there is a need for recognition that “bigger is not always better”. In fact, current NCCN guidelines acknowledge that “not all genes included on available multi-gene tests are necessarily clinically actionable” [7]. Additionally, variant of uncertain significance (VUS) results, which become increasingly common as more genes are tested, have added another layer of complexity to the pre-test genetic counseling risk assessment [42]. These uncertainties must be shared with patients as part of the process of informed consent for testing [29], recognizing that VUS results do not inform medical care and results should be interpreted similar to negative test results.
VUS results may present a complication for patients if not properly explained, and there is data to suggest significant gaps in both provider understanding and confidence to guide medical management patients with VUS results. A study based in the United Kingdom reported that 71% of providers expressed uncertainty about the clinical utility of BRCA VUS results and 39% did not know how to communicate results to patients with no family history [43]. Another registry-based study of breast cancer survivors reported that 50% of average-risk breast cancer patients with a BRCA VUS underwent bilateral mastectomy, which highlights the limited understanding and interpretation of VUS results among some providers [35].
There are many factors to consider when ordering genetic testing for patients, given the variations in multi-gene panel tests offered across laboratories, including: (1) multi-gene panel tests offered; (2) genes included on the various panels; (3) testing methodologies; (4) detection rates; and (5) additional offerings including RNA testing and paired tumor/germline testing [44]. Furthermore, results interpretation vary across genetic testing laboratories due to different internal approaches to variant classification along with different sets of patient data. This can result in discrepant results where one lab may call a variant likely pathogenic, which would lead to changes in medical management, while another lab calls the exact same variant a VUS which typically would not alter medical management [45]. Moreover, even the terminology to classify results differs across labs, with some using the American College of Medical Genetics variant terminology [46], while others use their own internal “home grown” terminology. Additionally, as data on specific variants become more robust, some labs are choosing to provide additional commentary beyond the typical “pathogenic” or “VUS” classifications, such as “moderate risk variant”, “special interpretation”, or “carrier”. While this information is critical to include in the interpretation of test results, there is often a lack of differentiation between two very different concepts: pathogenicity versus penetrance. While classification of pathogenicity is an indication of gene function (or dysfunction), penetrance indicates level of cancer risks in the context of a P/LP variant. An example is the CHEK2 I157T variant. Most major labs agree that this variant is associated with lower cancer risks than other pathogenic CHEK2 mutations, particularly the 1100delC variant. However, in the absence of any guiding recommendations, communication of this information varies with labs reporting it as: (1) a “Special Interpretation” comment (with an asterisk to a ‘see below’ comment for explanation); (2) “moderate risk mutation”; (3) “pathogenic (low penetrance) variant”; or (4) VUS. These disparate ways to document the same variant illustrating the challenges ahead as more robust genotype/phenotype data become available.
When performing testing through next-generation sequencing, it is important to recognize that variations larger than a few base pairs in size cannot readily be recognized across all testing platforms. Thus, most laboratories supplement next-generation sequencing with additional techniques to provide evaluation of larger, structural genomic mutations [29]. Additionally, some germline testing labs are now offering upfront RNA analysis in addition to their standard testing which has the potential to detect intronic pathogenic mutations and clarify VUS’s up front so they are not reported (particularly splice variants) [47]. One study found that concurrent RNA analysis led to 1 in 43 patients having different medical management than standard testing [47].
Consequently, providers offering genetic testing services, as well as those who order the tests in the clinics as part of routine patient care, must be familiar with the different labs’ testing approaches to select the most appropriate lab for their patients’ genetic testing needs [29]. As more genes are tested for, the chance for detecting a VUS increases [48,49,50]. Additionally, the likelihood of finding a VUS with larger multi-gene cancer panels is even higher for racial and ethnic minority groups [49, 50], who may also have lower diagnostic yield when compared to patients from European ancestry [51]. Standardizing the quality of genetic services provided to all racial and ethnic groups is of paramount importance as gene-based care expands.
Delivery of follow-up care
The purpose of genetic testing is to provide personal genetic information to individuals, with the goal of improving outcomes for individuals and their at-risk family members through cancer risk management, cancer treatment, and family communication of genetic test results (see Fig. 2). Appropriate delivery of follow-up care after genetic testing is critical, without which outcomes from genetic testing will not be improved.
Cancer risk management
The identification of HBC may empower individuals and their families with options to detect cancers early or prevent them [52,53,54]. In an effort to guide appropriate cancer risk management, a clinical validity framework has been developed through the Clinical Genome Resource (ClinGen) to classify genes based on the strength of evidence for association to a particular disease into definitive, strong, moderate, limited, disputed, or no reported evidence [55]. High and moderate penetrance genes are generally established to have an increased risk of HBC, in contrast to other genes with insufficient data to establish an association with breast cancer and penetrance [7]. Consequently, penetrance data in conjunction with clinical utility inform risk management [56], and management recommendations are based on both lifetime breast cancer risks and age distribution of risks. For example, earlier age of breast cancer screening with breast MRI and consideration of prophylactic surgery is advised for those with high penetrance HBC genes; in contrast, breast MRI at later ages is advised for those with moderate penetrance HBC genes with additional guidance based on family history and other modifying factors [7, 46, 57]. It is also important that ‘preliminary evidence’ genes with unconfirmed or uncertain cancer risks on multi-gene panel tests, are not used to guide cancer risk surveillance and management [7]. Among female BRCA1/2 carriers, risk-reducing mastectomy and risk-reducing salpingo-oophorectomy are two surgical options that reduce the risk of developing breast and ovarian cancer by ~ 90% [58]. While rates of contralateral prophylactic mastectomy for breast cancer patients have increased [59], cancer risk management guidance is imperative to prevent over- or under-treatment.
We and others have previously shown overtreatment through risk-reducing surgeries among women with BRCA1/2 VUS results and moderate penetrance HBC genes [35, 60,61,62]. In fact, our recently published study showed that 52% of women with a ATM or CHEK2 P/LP variant had contralateral prophylactic mastectomies [60]. Similarly, 43% of non-BRCA carriers of a P/LP variant had bilateral mastectomies [61] and 10–15% of women with moderate penetrance or VUS results had prophylactic oophorectomies [62], which suggests potential overtreatment. On the other hand, studies have also shown reduced uptake of cancer risk management strategies when indicated, especially among minority groups [13]. In fact, we previously reported on the reduced uptake of risk-reducing salpingo-oophorectomy among young Black women with breast cancer, compared to Whites and Hispanics [13]. These studies highlight the importance of promoting guideline-adherent, risk-appropriate gene-based care across all populations.
Cancer treatment
Identification of HBC may impact therapeutic options, including the expansion of genetic testing to guide eligibility for specific drugs based on genetic test results [63]. For example, PARP inhibitors are now FDA approved for use among women with germline BRCA1/2 P/LP variants with high-risk, localized and metastatic HER2 breast cancer, after they were shown to improve breast cancer outcomes [63,64,65].
Family communication
In addition to the impact of identifying HBC on cancer risk management and treatment, this information may be shared with at-risk family members to identify those with P/LP variants in whom cancer risk management strategies may be implemented to improve outcomes [66, 67]. We have previously shown BRCA carriers are likely to disclose genetic test results with at least one relative [68], while women with P/LP variants in non-BRCA genes had lower rates of family sharing and family testing (i.e., cascade testing) [69]. In one study, 97% of BRCA carriers informed at least one relative, yet only 48% had cascade testing [70]. Without the identification of family members with P/LP variants (through cascade testing), the promise of cancer risk management strategies to improve outcomes cannot be realized. Furthermore, our prior study in young Black women with breast cancer showed lower rates of family disclosures [68], which is unfortunate given the implications for prevention and early detection in an already high-risk population.
Strategies to address increasing demand for inherited cancer services
Identification, access, & uptake
Barriers to identification of HBC carriers and access to care include cost, geographic access to services, potential provider discrimination and bias, and lack of patient and provider education and awareness (Fig. 3). A multi-level approach to address barriers to identification, access, and uptake relevant to genetic counseling and testing services includes increasing awareness and utilization of services through community outreach, as well as patient and provider education (Table 1).
Patient-level strategies to increase genetic counseling and testing uptake for breast cancer patients include increasing patient awareness of genetic testing and patient-centered education tools tailored to meet the needs of a widely diverse patient population. Future work to better understand the patient experience, needs of patients during genetic counseling and testing, patient-reported outcomes, and the barriers patients face in receiving genetic services is necessary.
Provider-level strategies include targeted education to improve overall proficiency in genetics across the healthcare workforce including nurses, advanced practice providers and physicians in internal medicine, and numerous specialty fields including radiology, surgery, and obstetrics/gynecology. Educational provider tools might include in-person didactic learning presentations, webinars, printed education materials, and opportunities for feedback.
System-level approaches to improve uptake of genetic testing among appropriate breast cancer patients include the implementation of electronic health record (EHR) prompts, integrated risk assessment tools in the EHR, web-based screening applications and telehealth [71,72,73,74,75]. Technology-based solutions including efforts to identify and alert treating physicians through EHR prompts have shown promise to increase the number of appropriate referrals of cancer patients for genetic counseling [76].
Delivery of genetic counseling and genetic testing
To meet the demand for genetic services for HBC and overcome barriers to providing appropriate, effective, and equitable services, multi-level solutions (Table 1) at the system, provider, and patient levels have been proposed. Point-of-care genetic testing, defined as testing in the context of existing appointments and care through providers without formal training in genetics (i.e., non-GHP), is a model increasingly being used across clinics. As most hereditary cancer genetic counseling and testing is provided by non-GHPs, this model is supported through non-GHPs partnering with GHPs to provide decision support [77]. Furthermore, technology-based solutions may be used to streamline pre-test genetic education, as we and others have previously reported on [78, 79], and is an example of an alternative delivery model (ADM) which has tremendous potential to increase throughput and utilize the expertise of GHPs where they may have the most impact.
ADMs were developed to enable genetic counselors to work at the top of their scope of practice while improving access to their services, and various ADMs serve to solve different problems [80]. One ADM which can help lower wait times involves genetic counseling assistants (GCAs). GCAs can be used to complete administrative tasks and pre- and post-appointment activities that traditionally were completed by genetic counselors including family history collection/pedigrees, obtaining relevant records prior to consult and in some models, result disclosure after genetic counseling. This model has been found to increase patient volume and save costs per patient [81]. The goal of some ADMs is to reduce geographic and access barriers to patients receiving genetic counseling. In particular, the COVID-19 pandemic created barriers to many in-person medical services, including cancer genetics services. Studies of telephone genetic counseling related to BRCA testing found that it is non-inferior to in-person genetic counseling when cancer-specific distress and genetic knowledge were measured [82]. Ultimately, there will not be one single solution to the various challenges, but clinics are likely to use a combination of these models to improve and expand access to genetics services.
Follow-up care
Strategies to increase the uptake of follow-up care include increasing patient and provider awareness of the management recommendations. The integration of technology in the management of HBC has the potential to improve the follow-up care for patients by providing patients and providers with updates on changes in the management of HBC that are relevant to each patient. For example, there are digital health companies that provide personalized materials based on genetic test results to both patients and providers on up-to-date HBC management options [83]. In addition, implementation of EHR prompts is a system-based tool that can be used to standardize and automate recommendations based on genetic test results. As a result of our prior work [69, 78, 84], we developed a public facing website (www.geneshare.net) to provide tools and resources to enhance family communication of genetic test results. As a further extension of these efforts, we have secured funding to conduct a clinical trial to test interventions focused on guideline-adherent cancer risk management and family communication among those with inherited cancer predisposing genes (NCI U01CA254832).
Conclusion
Given the tremendous advancements in precision oncology, there is an increasing demand for cancer genetic services. There are, however, barriers to equitable access and uptake of cancer genetic services. Strategies focused on identification of individuals at risk for HBC, delivery of genetic services, and appropriate follow-up care are paramount to improve the quality of care delivered to patients with HBC.
Data availability
Data sharing not applicable to this article as no data sets were generated or analyzed during the current study.
References
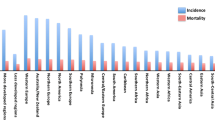
Bray F, Ferlay J, Soerjomataram I, Siegel RL, Torre LA, Jemal A (2018) Global cancer statistics 2018: GLOBOCAN estimates of incidence and mortality worldwide for 36 cancers in 185 countries. CA Cancer J Clin 68(6):394–424
Felix GES, Zheng Y, Olopade OI (2018) Mutations in context: implications of BRCA testing in diverse populations. Fam Cancer 17(4):471–483
Filippini SE, Vega A (2013) Breast cancer genes: beyond BRCA1 and BRCA2. Front Biosci (Landmark edition) 18:1358–1372
Stratton MR, Rahman N (2008) The emerging landscape of breast cancer susceptibility. Nat Genet 40(1):17–22
Gallagher S, Hughes E, Wagner S et al (2020) Association of a polygenic risk score with breast cancer among women carriers of high- and moderate-risk breast cancer genes. JAMA Netw Open 3(7):e208501–e208501
Piccinin C, Panchal S, Watkins N, Kim RH (2019) An update on genetic risk assessment and prevention: the role of genetic testing panels in breast cancer. Expert Rev Anticancer Ther 19(9):787–801
NCC Network (2021) Genetic/familial high-risk assessment: breast, ovarian and pancreatic. (Version2.2021). Available from https://www-nccn-org.proxy.library.vanderbilt.edu/. Accessed 14 Feb 2021
Ford D, Easton DF, Stratton M et al (1998) Genetic heterogeneity and penetrance analysis of the BRCA1 and BRCA2 genes in breast cancer families. The Breast Cancer Linkage Consortium. Am J Hum Genet 62(3):676–689
Ellsworth RE, Decewicz DJ, Shriver CD, Ellsworth DL (2010) Breast cancer in the personal genomics era. Curr Genomics 11(3):146–161
Thavaneswaran S, Rath E, Tucker K et al (2019) Therapeutic implications of germline genetic findings in cancer. Nat Rev Clin Oncol 16(6):386–396
Chen S, Parmigiani G (2007) Meta-analysis of BRCA1 and BRCA2 penetrance. J Clin Oncol 25(11):1329–1333
Kuchenbaecker KB, Hopper JL, Barnes DR et al (2017) Risks of breast, ovarian, and contralateral breast cancer for BRCA1 and BRCA2 mutation carriers. JAMA 317(23):2402–2416
Cragun D, Weidner A, Lewis C et al (2017) Racial disparities in BRCA testing and cancer risk management across a population-based sample of young breast cancer survivors. Cancer 123(13):2497–2505
Childers CP, Childers KK, Maggard-Gibbons M, Macinko J (2017) National estimates of genetic testing in women with a history of breast or ovarian cancer. J Clin Oncol 35:3800–3806
Bellcross CA, Kolor K, Goddard KA, Coates RJ, Reyes M, Khoury MJ (2011) Awareness and utilization of BRCA1/2 testing among U.S. primary care physicians. Am J Prev Med 40(1):61–66
Bellcross CA, Leadbetter S, Alford SH, Peipins LA (2013) Prevalence and healthcare actions of women in a large health system with a family history meeting the 2005 USPSTF recommendation for BRCA genetic counseling referral. Cancer Epidemiol Biomarkers Prev 22(4):728–735
Trivers KF, Baldwin LM, Miller JW et al (2011) Reported referral for genetic counseling or BRCA 1/2 testing among United States physicians: a vignette-based study. Cancer 117(23):5334–5343
Wood ME, Kadlubek P, Pham TH et al (2014) Quality of cancer family history and referral for genetic counseling and testing among oncology practices: a pilot test of quality measures as part of the American Society of Clinical Oncology Quality Oncology Practice Initiative. J Clin Oncol 32(8):824–829
Jones T, Lockhart JS, Mendelsohn-Victor KE et al (2016) Use of cancer genetics services in African-American young breast cancer survivors. Am J Prev Med 51:427–436
Levy DE, Byfield SD, Comstock CB et al (2011) Underutilization of BRCA1/2 testing to guide breast cancer treatment: black and Hispanic women particularly at risk. Genet Med 13(4):349–355
Jagsi R, Griffith KA, Kurian AW et al (2015) Concerns about cancer risk and experiences with genetic testing in a diverse population of patients with breast cancer. J Clin Oncol 33(14):1584–1591
McCarthy AM, Bristol M, Domchek SM et al (2016) Health care segregation, physician recommendation, and racial disparities in BRCA1/2 testing among women with breast cancer. J Clin Oncol 34:2610–2618
Febbraro T, Robison K, Wilbur JS et al (2015) Adherence patterns to National Comprehensive Cancer Network (NCCN) guidelines for referral to cancer genetic professionals. Gynecol Oncol 138(1):109–114
Schwartz MD, Lerman C, Brogan B et al (2005) Utilization of BRCA1/BRCA2 mutation testing in newly diagnosed breast cancer patients. Cancer Epidemiol Biomarkers Prev 14(4):1003–1007
Susswein LR, Skrzynia C, Lange LA, Booker JK, Graham ML 3rd, Evans JP (2008) Increased uptake of BRCA1/2 genetic testing among African American women with a recent diagnosis of breast cancer. J Clin Oncol 26(1):32–36
Riley BD, Culver JO, Skrzynia C et al (2012) Essential elements of genetic cancer risk assessment, counseling, and testing: updated recommendations of the National Society of Genetic Counselors. J Genet Couns 21(2):151–161
Robson ME, Bradbury AR, Arun B et al (2015) American Society of Clinical Oncology policy statement update: genetic and genomic testing for cancer susceptibility. J Clin Oncol 33(31):3660–3667
American College of Surgeons. National Accreditation Program for Breast Centers. NAPBC Standards Manual 2018 Edition. 2018:77. https://accreditation.facs.org/accreditationdocuments/NAPBC/Portal%20Resources/2018NAPBCStandardsManual.pdf. Accessed 10 July 2021
Fecteau H, Pal T (2015) Clinical considerations in the conduct of cancer next-generation sequencing testing and genetic counseling. In: Wu W, Choudhry H (eds) Next generation sequencing in cancer research, volume 2: from basepairs to bedsides. Springer International Publishing, Cham
Boothe E, Greenberg S, Delaney CL, Cohen SA (2021) Genetic counseling service delivery models: a study of genetic counselors’ interests, needs, and barriers to implementation. J Genet Couns 30(1):283–292
Penon-Portmann M, Chang J, Cheng M, Shieh JT (2019) Genetics workforce: distribution of genetics services and challenges to health care in California. Genet Med. https://doi.org/10.1038/s41436-019-0628-5
Villegas C, Haga SB (2019) Access to genetic counselors in the southern United States. J Pers Med 9(3):33
Hoskovec JM, Bennett RL, Carey ME et al (2018) Projecting the supply and demand for certified genetic counselors: a workforce study. J Genet Couns 27(1):16–20
Reid S, Cragun D, Tezak A et al (2020) Disparities in BRCA counseling across providers in a diverse population of young breast cancer survivors. Genet Med. https://doi.org/10.1038/s41436-020-0762-0
Kurian AW, Li Y, Hamilton AS et al (2017) Gaps in incorporating germline genetic testing into treatment decision-making for early-stage breast cancer. J Clin Oncol 35(20):2232–2239
Whitworth P, Beitsch P, Arnell C et al (2017) Impact of payer constraints on access to genetic testing. J Oncol Pract 13(1):e47–e56
Stenehjem DD, Au T, Sainski AM et al (2018) Impact of a genetic counseling requirement prior to genetic testing. BMC Health Serv Res 18(1):165
Cragun D, Kinney AY, Pal T (2017) Care delivery considerations for widespread and equitable implementation of inherited cancer predisposition testing. Expert Rev Mol Diagn 17(1):57–70
Hughes E, Judkins T, Wagner S et al (2018) Abstract PD1-08: development and validation of a combined residual risk score to predict breast cancer risk in unaffected women negative for mutations on a multi-gene hereditary cancer panel. Cancer Res 78(4 Supplement):PD1-08-PD01-08
Du Z, Gao G, Adedokun B et al (2021) Evaluating polygenic risk scores for breast cancer in women of African ancestry. J Natl Cancer Inst. https://doi.org/10.1093/jnci/djab050
Martin AR, Kanai M, Kamatani Y, Okada Y, Neale BM, Daly MJ (2021) Publisher correction: clinical use of current polygenic risk scores may exacerbate health disparities. Nat Genet 53(5):763
Mersch J, Brown N, Pirzadeh-Miller S et al (2018) Prevalence of variant reclassification following hereditary cancer genetic testing. JAMA 320(12):1266–1274
Eccles BK, Copson E, Maishman T, Abraham JE, Eccles DM (2015) Understanding of BRCA VUS genetic results by breast cancer specialists. BMC Cancer 15(1):936
Hall MJ, Forman AD, Pilarski R, Wiesner G, Giri VN (2014) Gene panel testing for inherited cancer risk. J Natl Compr Canc Netw 12(9):1339–1346
Balmaña J, Digiovanni L, Gaddam P et al (2016) Conflicting interpretation of genetic variants and cancer risk by commercial laboratories as assessed by the prospective registry of multiplex testing. J Clin Oncol 34(34):4071–4078
Richards S, Aziz N, Bale S et al (2015) Standards and guidelines for the interpretation of sequence variants: a joint consensus recommendation of the American College of Medical Genetics and Genomics and the Association for Molecular Pathology. Genet Med 17(5):405–424
Karam R, Conner B, LaDuca H et al (2019) Assessment of diagnostic outcomes of RNA genetic testing for hereditary cancer. JAMA Netw Open 2(10):e1913900–e1913900
Kurian AW, Hughes E, Handorf EA et al (2017) Breast and ovarian cancer penetrance estimates derived from germline multiple-gene sequencing results in women. JCO Precis Oncol 1:1–12
Caswell-Jin JL, Gupta T, Hall E et al (2018) Racial/ethnic differences in multiple-gene sequencing results for hereditary cancer risk. Genet Med 20(2):234–239
Kurian AW, Ward KC, Abrahamse P et al (2021) Time trends in receipt of germline genetic testing and results for women diagnosed with breast cancer or ovarian cancer, 2012–2019. J Clin Oncol. https://doi.org/10.1200/JCO.20.02785
Ndugga-Kabuye MK, Issaka RB (2019) Inequities in multi-gene hereditary cancer testing: lower diagnostic yield and higher VUS rate in individuals who identify as Hispanic, African or Asian and Pacific Islander as compared to European. Fam Cancer 18(4):465–469
Watson M, Kash KM, Homewood J, Ebbs S, Murday V, Eeles R (2005) Does genetic counseling have any impact on management of breast cancer risk? Genet Test 9(2):167–174
Roukos DH, Briasoulis E (2007) Individualized preventive and therapeutic management of hereditary breast ovarian cancer syndrome. Nat Clin Pract Oncol 4(10):578–590
Narod SA, Offit K (2005) Prevention and management of hereditary breast cancer. J Clin Oncol 23(8):1656–1663
Lee K, Seifert BA, Shimelis H et al (2019) Clinical validity assessment of genes frequently tested on hereditary breast and ovarian cancer susceptibility sequencing panels. Genet Med 21(7):1497–1506
Tung N, Domchek SM, Stadler Z et al (2016) Counselling framework for moderate-penetrance cancer-susceptibility mutations. Nat Rev Clin Oncol 13(9):581–588
Cybulski C, Wokołorczyk D, Jakubowska A et al (2011) Risk of breast cancer in women with a CHEK2 mutation with and without a family history of breast cancer. J Clin Oncol 29(28):3747–3752
Domchek SM, Friebel TM, Singer CF et al (2010) Association of risk-reducing surgery in BRCA1 or BRCA2 mutation carriers with cancer risk and mortality. JAMA Oncol 304(9):967–975
Tuttle TM, Habermann EB, Grund EH, Morris TJ, Virnig BA (2007) Increasing use of contralateral prophylactic mastectomy for breast cancer patients: a trend toward more aggressive surgical treatment. J Clin Oncol 25(33):5203–5209
Cragun D, Weidner A, Tezak A, Clouse K, Pal T (2020) Cancer risk management among female BRCA1/2, PALB2, CHEK2, and ATM carriers. Breast Cancer Res Treat 182(2):421–428
Kurian AW, Ward KC, Abrahamse P et al (2020) Association of germline genetic testing results with locoregional and systemic therapy in patients with breast cancer. JAMA Oncol 6(4):e196400
Domchek SM, Brower J, Symecko H et al (2020) Uptake of oophorectomy in women with findings on multigene panel testing: results from the Prospective Registry of Multiplex Testing (PROMPT). J Clin Oncol 38(15_suppl):1508
Robson M, Im S-A, Senkus E et al (2017) Olaparib for metastatic breast cancer in patients with a germline BRCA mutation. N Engl J Med 377(6):523–533
Tutt ANJ, Garber JE, Kaufman B et al (2021) Adjuvant olaparib for patients with BRCA1- or BRCA2-mutated breast cancer. N Engl J Med 384(25):2394–2405
Litton JK, Rugo HS, Ettl J et al (2018) Talazoparib in patients with advanced breast cancer and a germline BRCA mutation. N Engl J Med 379(8):753–763
Domchek SM, Friebel TM, Singer CF et al (2010) Association of risk-reducing surgery in BRCA1 or BRCA2 mutation carriers with cancer risk and mortality. JAMA 304(9):967–975
Finch AP, Lubinski J, Moller P et al (2014) Impact of oophorectomy on cancer incidence and mortality in women with a BRCA1 or BRCA2 mutation. J Clin Oncol 32(15):1547–1553
Conley CC, Ketcher D, Reblin M et al (2020) The big reveal: family disclosure patterns of BRCA genetic test results among young Black women with invasive breast cancer. J Genet Couns. https://doi.org/10.1002/jgc4.1196
Cragun D, Weidner A, Tezak A, Clouse K, Pal T (2021) Family communication of genetic test results among women with inherited breast cancer genes. J Genet Couns 30(3):701–709
Lieberman S, Lahad A, Tomer A et al (2018) Familial communication and cascade testing among relatives of BRCA population screening participants. Genet Med 20(11):1446–1454
Cragun D, Pal T (2013) Identification, evaluation, and treatment of patients with hereditary cancer risk within the United States. ISRN Oncol 2013:260847
Centers for Disease Control and Prevention (2017) Bring Your Brave Campaign. https://www.cdc.gov/cancer/breast/young_women/bringyourbrave/health_care_provider_education/risk_assessment_tools.htm. Accessed 1 June 2021
Biswas S, Atienza P, Chipman J et al (2016) A two-stage approach to genetic risk assessment in primary care. Breast Cancer Res Treat 155(2):375–383
Brannon Traxler L, Martin ML, Kerber AS et al (2014) Implementing a screening tool for identifying patients at risk for hereditary breast and ovarian cancer: a statewide initiative. Ann Surg Oncol 21(10):3342–3347
DeFrancesco MS, Waldman RN, Pearlstone MM et al (2018) Hereditary cancer risk assessment and genetic testing in the community-practice setting. Obstet Gynecol. https://doi.org/10.1097/AOG.0000000000002916
Powell CB, Littell R, Hoodfar E, Sinclair F, Pressman A (2013) Does the diagnosis of breast or ovarian cancer trigger referral to genetic counseling? Int J Gynecol Cancer 23(3):431–436
Pal T, Radford C, Weidner A, Tezak AL, Cragun D, Wiesner GL (2018) The Inherited Cancer Registry (ICARE) initiative: an academic-community partnership for patients and providers. Oncol Issues 33(6):54–63
Cragun D, Weidner A, Tezak A, Zuniga B, Wiesner GL, Pal T (2020) A web-based tool to automate portions of pretest genetic counseling for inherited cancer. J Natl Compr Cancer Netw 18(7):841–847
Watson CH, Ulm M, Blackburn P et al (2016) Video-assisted genetic counseling in patients with ovarian, fallopian and peritoneal carcinoma. Gynecol Oncol 143(1):109–112
Stoll K, Kubendran S, Cohen SA (2018) The past, present and future of service delivery in genetic counseling: keeping up in the era of precision medicine. Am J Med Genet C 178(1):24–37
Hallquist MLG, Tricou EP, Hallquist MN et al (2020) Positive impact of genetic counseling assistants on genetic counseling efficiency, patient volume, and cost in a cancer genetics clinic. Genet Med 22(8):1348–1354
Bracke X, Roberts J, McVeigh TP (2020) A systematic review and meta-analysis of telephone vs in-person genetic counseling in BRCA1/BRCA2 genetic testing. J Genet Couns. https://doi.org/10.1002/jgc4.1343
MyGeneCounsel (2019) White paper: how often do medical management guidelines change for people with germline genetic findings? https://www.mygenecounsel.com/wp-content/uploads/2019/10/How-Often-Do-Medical-Management-Guidelines-Change.pdf?utm_source=mailchimp&utm_campaign=0300b2cee1f0&utm_medium=page. Accessed 10 Dec 2019
Dean M, Tezak AL, Johnson S et al (2021) Sharing genetic test results with family members of BRCA, PALB2, CHEK2, and ATM carriers. Patient Educ Couns 104(4):720–725
Acknowledgements
Sonya Reid’s research was supported by a NIH training grant (5K12CA090625-20).
Author information
Authors and Affiliations
Corresponding authors
Ethics declarations
Conflict of interest
The authors declare that they have no conflict of interest.
Additional information
Publisher's Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Rights and permissions
About this article
Cite this article
Reid, S., Spalluto, L.B., Lang, K. et al. An overview of genetic services delivery for hereditary breast cancer. Breast Cancer Res Treat 191, 491–500 (2022). https://doi.org/10.1007/s10549-021-06478-z
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s10549-021-06478-z