Abstract
Breast cancer is the leading cause of cancer in women in Spain and its annual incidence is rapidly increasing. Thanks to the screening programs in place, nearly 90% of breast cancer cases are detected in early and potentially curable stages, despite the COVID-19 pandemic possibly having impacted these numbers (not yet quantified). In recent years, locoregional and systemic therapies are increasingly being directed by new diagnostic tools that have improved the balance between toxicity and clinical benefit. New therapeutic strategies, such as immunotherapy, targeted drugs, and antibody–drug conjugates have also improved outcomes in some patient subgroups. This clinical practice guideline is based on a systematic review of relevant studies and on the consensus of experts from GEICAM, SOLTI, and SEOM.
Similar content being viewed by others
Introduction
Breast cancer is a major public health problem given its high incidence, prevalence, and mortality, representing the most common cancer among women in Spain and accounting for 35,000 new cases per year. Moreover, it is the leading cause of cancer-related mortality in the female population, responsible for 6651 cancer deaths per year [1].
Breast cancer is a heterogeneous disease with marked clinical and biological heterogeneity, leading to many therapeutic decisions being individualized depending on molecular and clinical characteristics. Despite the success in implementing early breast cancer detection campaigns, up to one in three patients will develop metastases. Moreover, approximately one in 8–9 new diagnoses currently present as metastatic disease; these figures may be worse because of screening delays across the country due to COVID19 pandemic [2].
The aim of these guidelines was to summarize and categorize current evidence that arises useful clinical therapeutic recommendations in the clinical practice.
Methodology
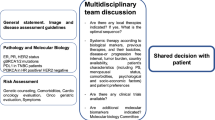
This guideline is based on a systematic review of relevant published studies and with the consensus of ten oncologists who are experts in treatment of breast cancer from GEICAM, SOLTI, and SEOM, as well as an external review panel comprising two experts designated by SEOM. The Infectious Diseases Society of America-US Public Health Service Grading System for Ranking Recommendations in Clinical Guidelines Infectious Diseases Society of America-US Public Health Service Grading System for Ranking Recommendations in Clinical Guidelines [3] has been used to assign levels of evidence and grades of recommendation (Table 1).
Diagnosis and staging
To diagnose breast cancer, a clinical, radiological, and pathological examination is necessary. Staging should be conducted according to TNM and the AJCC system [4]. A proper anamnesis with personal and family history and a complete physical examination (palpation of the breasts, regional lymph nodes, and assessment for distant metastases) should be performed. Furthermore, the following radiological tests should be performed to establish an accurate diagnosis:
-
1.
Bilateral mammography and ultrasound of the breast and regional lymph nodes (I, A) [5]. New techniques, such as 3D mammography or 3D ultrasound, increase diagnostic accuracy, but are not routinely implemented.
-
2.
Core needle biopsy (preferably under ultrasound or stereotactic guidance) (I, A).
-
3.
Fine needle aspiration or core biopsy of suspicious lymph nodes is recommended (II, A).
-
4.
Breast magnetic resonance imaging (MRI) is optional (I, B) and should be only considered in cases of positive axillary nodes; occult primary breast cancer; Paget’s disease of the nipple; lobular carcinoma; multifocal, multicentric lesions, and breast cancer implants. It is also recommended pre- and post-neoadjuvant treatment to define the extent of disease and monitor treatment response (III, A) [6].
-
5.
Additional studies: Evaluation of cardiac function is imperative when using anthracyclines or antiHER2-targeted therapies (I, A) [7]. Laboratory tests (complete blood count, liver and renal function, alkaline phosphatase, and calcium) are routinely performed, but do not appear to improve detection of occult metastatic disease (III, C) [8]. Additional systemic staging should be contemplated when disease is detected in stage III or when signs, symptoms, or laboratory values indicate possible metastasis. This more comprehensive study includes chest, abdominal, and pelvic imaging, and bone scan (III, B). PET/CT may be of use when traditional imaging test are inconclusive (III,A) or in cases of locally-advanced tumors [9, 10].
Pathology and molecular biology
The pathological diagnosis should be made according to the World Health Organization (WHO) classification. The two most frequent subtypes are invasive carcinoma of no special type, which accounts for approximately 70–75%, and lobular carcinoma, representing between 12 and 15% of all breast cancers. The other ≤ 5% are rare histologies, each with its distinct pathologic features and prognosis [11, 12]. Tumor grade and the presence of in situ carcinoma are also relevant features to determine.
Estrogen receptor (ER) and progesterone receptor (PgR) expression should be ascertained by immunohistochemistry (IHC), and reporting of the new category ER Low Positive should be done for those tumors with 1 to 10% positive staining [13]. HER2 status should also be determined as per ASCO-CAP guidelines (I, A) [14]. Proliferation markers such as Ki67 yield additional, useful information. Nevertheless, the high inter-observer variability in the Ki67 determination must be taken into consideration when using it for decision-making [15].
Recent years have witnessed the emergence of new markers in an attempt to substantiate differences in pathogenesis, treatment response, and prognosis:
Tumor-infiltrating lymphocytes (TILs) have proven to predict pathological complete response (pCR) to CT and good prognosis in triple negative and HER2-positive breast cancer [16, 17]. Nevertheless, its use for treatment selection is discouraged at present [18].
In the early, HR positive, HER2-negative setting, various platforms are available (Oncotype®, ProsignaTM®, Mammaprint®, and Endopredict®) and can be of value for adjuvant treatment decision in pre- or post-menopausal patients with node-negative disease and in post-menopausal patients with 1–3 positive lymph nodes [19,20,21].
In HER2-positive disease, the HER2DX 27-gene test has recently emerged as a useful clinical tool [22,23,24,25]. The HER2DX test provides two independent scores indicating prognosis when treated with trastuzumab-based CT (HER2DX risk-score), and the probability of achieving a pathological complete response following trastuzumab-based therapy (HER2DX pCR-score). Thus, HER2DX can help to identify suitable candidates for escalation and de-escalation treatment strategies in some clinical situations, even when this tool needs additional validation (II, B).
Local–regional therapy
Surgery
Surgical treatment of breast cancer (BC) may consist of tumor excision with surrounding normal breast tissue BCS or mastectomy [26].
Long-term follow-up of randomized clinical trials has revealed similar survival rates for women treated with either BCS or mastectomy (I, A) [27]. Mastectomy is indicated in the following cases: locally advanced tumors, tumor multicentricity, small breast size for tumor volume, inability to achieve negative surgical margins after multiple resections, and contraindications to radiotherapy [28, 29].
Currently, an increasing percentage of women with BC stage II or III receive primary neoadjuvant systemic therapy (NST). In these patients, surgical and radiation treatments are based on the tumor’s initial stage and response to NST. The absence of ink in the tumor comprises a sufficient surgical margin in most cases of BC (I, A) [30].
Patients with BC and germline BRCA1/2 mutations can be considered for BCS, with local control similar to that of non-carriers (I, A). The increased risk of contralateral BC and of new cancers in the ipsilateral breast warrant discussing bilateral mastectomy with the patient (I, A). Nipple-sparing mastectomy is a reasonable approach in these women, provided there is adequate distance from tumor surgical margin [31].
Sentinel lymph node biopsy (SLNB) is standard for patients undergoing BCS with clinically negative axilla assessed by ultrasound imaging (I, A) [32]. Axillary lymph node dissection (ALND) can be omitted after SLNB with one or two positive lymph nodes following mastectomy provided that regional nodal irradiation (RNI), including the axilla, is planned (I, A). ALND may be omitted after SLNB with one or two positive lymph nodes post-BCS for tumors > 5 cm if RNI is planned (III, B). In women undergoing mastectomy with positive sentinel lymph nodes for whom radiation is not planned, complete axillary dissection is recommended (III, B) [30, 33].
Clinically node-positive patients after NST are advised to undergo complete axillary dissection (I, A). SLNB is a post- NST staging procedure for cN0 patients (I, A). In those with a clinically positive axillary node (cN1) who achieve a complete clinical response after NST, axillary dissection can be avoided if ≥ 3 sentinel nodes are identified and all are negative, or when the marked involved node(s) at diagnoses is/are removed, in addition to the sentinel node, and all of them are free of tumor cells [34]. Any residual nodal disease after NST on sentinel node biopsy usually warrant ALND (RT trials are on-going). Patients with cN2 axillary disease should undergo ALND, regardless of response to NST (I, A) [30, 35, 36].
Adjuvant radiotherapy
After BCS, adjuvant RT is the standard treatment (I, A) [37, 38]. Hypofractionated whole breast irradiation (WBI) represents the preferred approach, with a treatment duration of 3–4 weeks (I, A). Currently, five-fraction WBI regimens have also emerged as standard of care for certain patients based on data from the FAST and FAST-Forward trials (I, A) [39]. Omission of breast irradiation in elderly patients with low risk ER-positive tumors is considered a safe option, although a higher incidence of local recurrence is expected (I, A) [40].
In cases of involvement of ≥ 4 axillary lymph nodes, regional nodal irradiation (RNI) is recommended, as it increases survival in node-positive BC (I, A) [41]. In cases of 1–3 positive lymph nodes, if there are adverse prognostic factors, such as triple negative, HER2, luminal B cancers, and in women with residual disease after NST, experts recommend RNI, regardless of whether mastectomy or BCS have been performed (I, B). Similarly, postmastectomy radiotherapy to the chest wall and regional lymph nodes is recommended in cases of ≥ 4 node-positive nodes (I, A).
Principles of adjuvant systemic therapy
Breast cancer (BC) is a heterogeneous disease, with different subtypes having a distinct biological, molecular, and clinical outcome. Systemic adjuvant treatment is commonly used in early breast cancer with the intention of lowering the rate of locoregional or systemic relapses and death derived from the disease. Treatment decisions are based on clinical (age, comorbidities) and pathologic factors (tumor size, nodal status, grade, Ki67, HR status, and HER2 status). Multigenic tests provide information beyond standard clinical and pathologic prognostic factors that can aid in making treatment decisions.
Prognostic gene expression-based assays
Gene expression-based assays, such as OncotypeDx Recurrence Score, Mammaprint, Endopredict, and Prosigna can be used to gain additional prognostic and/or predictive information regarding the benefit of adjuvant CT in early HR-positive and HER2-negative BC (I, A) (Table 2). New data have recently been reported to inform adjuvant ET and CT use on the basis of patient age, menopausal status, and number of axillary nodes involved (II,B) [19, 42,43,44,45,46,47,48,49] (Tables 2 and 3).
Recommendations:
-
Genomic platforms are not recommended for the following: clinically low-risk tumors (pT1a, b, node negative, low grade, ER-high) and/or patients with health conditions who are not candidates for CT (I, D).
-
Genomic platforms are not recommended for the following: 1–3 involved nodes coexisting with other high-risk factors and/or premenopausal patients, or patients with > 3 positive nodes for whom adjuvant CT is indicated (I, A).
-
Oncotype Dx is recommended in premenopausal patients with node negative tumors (IA). Based on TailorX results, CT has some benefit for distant recurrence if the RS is 16–25 (II, B).
-
Oncotype DX, MammaPrint, and EndoPredict can be useful to guide adjuvant treatment in postmenopausal or > 50 year patients with node negative or 1–3 positive nodes (I, A; I, A; II, B) [50].
-
Prosigna may be used in postmenopausal patients with node-negative tumors (II, B) [51].
-
Dynamic changes in Ki67 after 2 weeks of perioperative ET in postmenopausal women can be considered a surrogate prognostic factor based on the POETIC trial (II, B) [52].
Systemic treatment for early-stage luminal-type breast cancer
Adjuvant endocrine therapy for early-stage breast cancer
There is robust evidence that ET improves survival of early-stage luminal breast cancer (BC). Adjuvant ET should be offered to all ER + patients regardless of age, menopausal status, CT exposure, hormone expression level (ER or PgR) (if any or both are positive defined as ER and/or PgR > 1/10%), and/or Her2 status (I,A) [53]. There are several ET options. The individual choice should be adjusted to menopause status, comorbidity, and risk of recurrence. Adjuvant systemic therapy is best started without undue delays, as data reveal an important decrease in efficacy when it is administered > 12 weeks after surgery (I, A) [54] (Fig. 1).
Recommendations for premenopausal patients:
-
Tamoxifen for 5 years is the most widely established adjuvant ET for low-risk premenopausal patients (I, A) [55]. Consider tamoxifen until 10 years in high-risk tumors in the presence of ovarian function (at the expense of greater toxicity) (I, B) [56, 57].
-
In high-risk premenopausal patients who recover menses or ovarian function after CT (in the first 12–18 months), the addition of ovarian function suppression + ET should be offered (I, A), being the most effective combination ovarian function suppression (OFS) with AI [58, 59].
-
In patients treated with AI + chemical OFS, clinicians should control estrogen levels biochemically at regular intervals (I,A), mainly in younger patients during the first year of treatment. LHRH analogues should be administered in the monthly schedule for these patients, for a total duration of 2. 5 to 5 years (I, A)
-
In patients becoming postmenopausal during the first 2–5 years of tamoxifen, a switch to aromatase inhibitor should be considered, depending on risk of late recurrence (II,A).Total duration of adjuvant ET should be 7.5 to 8 years if intermediate or high clinical risk of relapse (I, A)
Recommendations for postmenopausal patients:
-
For postmenopausal women, AIs (both non-steroidal and steroidal) are superior to tamoxifen (I, A), although tolerance and toxicity profiles should be individualized.
-
AIs can be used upfront (non-steroidal AI and exemestane), after 2–3 years of tamoxifen (non-steroidal AI and exemestane), or as extended adjuvant therapy, after 5 years of tamoxifen (letrozole and anastrozole) (I, A), especially in intermediate- to high-risk patients [60,61,62,63,64,65].
-
Extended adjuvant therapy should be discussed with all patients. Except those with a very low risk of relapse (I, A), the optimal duration of ET should be of 7.5 to 8 years. There is only a minimal benefit from the use of AIs for more than 8 years (I, C) [66]. The predictive benefit of Breast Cancer Index for extended ET has been demonstrated in various cohorts that include patients with 0–3 involved lymph nodes [67,68,69].
-
The option of 10 years of tamoxifen in postmenopausal patients could be considered in high-risk patients who decline or have a contraindication to AIs (I, A).
-
Biphosphonates are recommended in women with low-estrogen status and also in those with treatment-related bone loss (I, A) [70].
-
For high-risk patients, defined as tumors with ≥ 4 positive nodes, or 1–3 nodes and either tumor size > 5 cm, histologic grade 3, or Ki-67 > 20%, abemaciclib for 2 years in combination with ET is indicated for adjuvant treatment based on the MonarchE trial (I, A) [71]
-
In the Olympia trial, 1 year adjuvant olaparib demonstrated improved OS and DFS in patients with HER2-negative breast cancer with BRCA1 or BRCA2 germline pathogenic mutations, and high-risk clinic-pathological features (at least four pathologically-confirmed positive lymph nodes in the ER + population).Triple negative or ER + patients treated with NAC who don´t achieve a pCR ( CPS + EG score of ≥ 3 in the ER + group) are also candidates for this treatment (I, A) [72]. Despite this evidence, olaparib is still awaiting financial approval from the health authorities in Spain.
Adjuvant chemotherapy in hormone receptor-positive early BC
The use of CT as adjuvant treatment for ER + Her2-negative disease is recommended for high-risk tumors defined by either clinical or genomic profiling characteristics (I, A), considering: T2 to T4 tumors and/or axillary N2-3 involvement; high Ki67; low ER expression; younger age or premenopausal status, and intermediate- to high-risk genomic score.
Recommendations:
-
CT should be administered for 12–24 weeks (4–8 cycles) (I, A).
-
Sequential anthracycline/taxane-based regimen is the standard for most patients (I, A). Anthracycline-based regimens should not include 5-FU (EC or AC is standard) (I, A) [73, 74].
-
In selected lower-risk patients, 4 cycles of taxane-based CT or CMF may be used (II, B) [75, 76].
-
Non-anthracycline regimens may be used in patients at risk for cardiac complications (I, A) [76].
-
The use of dose-dense schedules (with granulocyte colony-stimulating factor support) should be considered in high-risk tumors (I, A) [77, 78].
In male patients, tamoxifen is the standard adjuvant systemic therapy (III, A); AIs should not be used alone in this setting. If a strong contraindication exists for the use of tamoxifen, a combination of an AI plus a luteinizing hormone-releasing hormone agonist may be considered (III, B). CT indications and regimens should follow the same recommendations as those for breast cancer in female patients (discus with patients higher toxicity and compliance) (III, A) [79,80,81].
Neoadjuvant treatment in hormone receptor-positive early BC
Neoadjuvant treatment is recommended in locally advanced tumors and in those situations where decrease the extent of surgery is needed (I, A). The timing of treatment (pre- versus postoperative) has no effect on long-term outcomes, except a possible small increase in locoregional recurrences, but without impact on survival (II, A) [82].
Recommendations:
-
NET alone may be offered to those postmenopausal patients with strongly HR-positive tumors (RE > 60% or RE 40–60% and PgR > 10%) (I, A). AIs are more effective than tamoxifen in decreasing Ki67 levels, tumor size and facilitating less extensive surgery (I, A) [83, 84].
-
The preferred ET option for postmenopausal patients is an aromatase inhibitor during at least 6–8 months or until maximum response (II, B).
-
NET is not routinely recommended in premenopausal patients, outside clinical trials. However, in highly selected patients with luminal A-like tumors and no indication for CT, who are not candidates for optimal surgery, OFS plus an aromatase inhibitor can be considered (II, C) [85].
-
Some phase II trials and one meta-analysis showed similar response rates comparing NET and CT, but a significantly lower toxicity with NET (II, B) [86].
-
The efficacy evaluation of NET has been performed according to surrogate parameters such as the decrease of the Ki67 levels during the first cycle of NET, or the preoperative endocrine prognostic index (PEPI) score after surgery (II, B) [87].
-
Different genetic signatures have been evaluated in core needle biopsy before neoadjuvant therapy, as good predictors of response to neoadjuvant therapy, especially PAM50 ROR score, although this approach is currently considered experimental (II, C) [88].
-
CT drugs and drug regimens used in the preoperative setting should be selected according to rules identical to those in the postoperative setting (I, A). A sequential regimen of anthracyclines and taxanes is recommended for the vast majority of patients (I, B).
Systemic treatment for HER2-positive early breast cancer
Neoadjuvant treatment for HER2-positive disease
Neoadjuvant treatment in HER2 positive breast cancer provides a useful information on pathological response that is a surrogate marker of DFS and potentially overall survival [89] (OS) and also, opens the window to the knowledge of residual disease and to tailor adjuvant strategies after surgery.
-
Patients with ≥ cT2 tumors or cN + should be treated with standard CT (Taxane-AC/EC or Taxane-Carboplatin) plus dual HER2 blockade, Pertuzumab (P) + Trastuzumab (T) [90]. This dual HER2 blockade efficacy has been endorsed by the latest analysis of CLEOPATRA study confirming OS benefit in the advanced setting [91] (I, A) (Fig. 2)
-
Established NAC regimens are either an anthracycline-taxane sequence plus P + T or docetaxel-carboplatin plus dual HER2 blockade, for a minimum of 9 weeks of taxane + antiHER2 therapy.
-
Recently, the TRAIN2 study suggested that an anthracycline combination does not add efficacy neither regarding pCR nor patient outcome to a sequential taxane-platinum containing regimen with dual antibody blockade [92]. The evidence for anthracycline-free CT in HER2 + early BC is reinforced in the neoadjuvant setting in TRYPHAENA trial and in the adjuvant setting in BCIRG 006. The incidence of significant declines in the left ventricular ejection fraction (LVEF) is lower without anthracycline containing regimen so this could be the chosen CT backbone if desire to avoid cardiotoxicity [93, 94] (II, B).
-
HER2DX risk score and pCR score has recently been developed and validated (both based on a 27-gene expression plus clinical feature-based classifier) and will provide accurate estimates of the risk of recurrence, and the likelihood to achieve a pCR, in early-stage HER2-positive breast cancer patients (II, B) [22,23,24,25].
Adjuvant treatment for HER2-positive disease
-
The administration of trastuzumab associated with adjuvant CT treatment demonstrated reduction in risk of relapse of 50% and also on mortality, regardless of tumor size, age, nodal and HR status [94,95,96]. The optimal duration of trastuzumab treatment has been established as 12 months (I, A) [97, 98]. It may be safely combined with either radiotherapy or ET. Adjuvant trastuzumab is recommended in all tumors with a tumor size > 1 cm regardless of nodal status (I, A). Adjuvant trastuzumab might be considered in node-negative tumor size 0.5-1 cm tumors, specially in ER- disease, although no level I evidence exists (II, B).
-
Thus, 4 cycles of AC or EC followed by 3 months of paclitaxel (P) or docetaxel (D or T) both in combination with trastuzumab (AC/EC → P/D + H), or docetaxel, carboplatin, and trastuzumab (TCH) are preferred regimens (I, A).
-
In stage I, treatment with paclitaxel for 12 weeks associated with trastuzumab should be considered based on the results of the phase II APT trial (II, B) [99].
-
In the Aphinity trial [100, 101], the addition of pertuzumab demonstrated a modest but significant benefit in invasive DFS (iDFS) in the node-positive cohort, regardless of HR status. No statistically significant difference in OS was found. Based on this trial, the EMA approved the use of 18 cycles of dual T + P treatment in the high-risk node-positive population, regardless of whether it was initiated in the adjuvant or the neoadjuvant setting (II, B). Despite this evidence, pertuzumab is still awaiting financial approval from health authorities in Spain.
-
The addition of 1 year of adjuvant neratinib improved iDFS in patients with HER2-positive breast cancer after 1 year of trastuzumab, as demonstrated in the phase III EXTENET trial [102]. The benefit was greater in patients with HR-positive and node-positive disease, at the expense of increased toxicity (diarrhea) (I, B). Neratinib has been approved by EMA, which restricted its use to HR + disease. The authorities in Spain also restrict its use to subjects who had not completed one year of trastuzumab for any reason.
-
In those patients who receive neoadjuvant treatment (minimun 6 cycles with at least 9 weeks of taxane + trastuzumab regimen) and who do not achieve pCR, 14 cycles of adjuvant T-DM1 substantially improve outcomes compared with adjuvant trastuzumab (KATHERINE trial) with a substantial difference in 3-year iDFS (88.3% vs 77%). This benefit is seen independently of adjuvant ET, radiotherapy or HER2 status in the residual disease [103] (I, A)
-
In patients with HER2-positive HR + BC, adjuvant ET should be administered following the same principles as in HER2-negative disease.
In patients with pCR, adjuvant anti-HER2 therapy with trastuzumab for a full year of total anti-HER2 therapy should be maintained (I, A). Patients with node-positive disease at diagnosis may receive pertuzumab added to trastuzumab if we extrapolate the results of the adjuvant APHINITY trial [100] (II, B).
Systemic treatment for triple negative breast cancer
Adjuvant treatment for triple‐negative disease
Triple negative breast cancer (TNBC) is a heterogeneous disease that accounts for approximately 15–20% of all breast cancers [104]. It tends to comprise high-grade tumors with a high proliferation index and a particular trend to metastasize early to different organs such as liver, lung, and central nervous system (CNS) [105].
While historically surgery and adjuvant CT have been considered the cornerstone of early TNBC treatment, NST has emerged as the preferred option not just in locally advanced tumors but in smaller tumors as well. Since systemic therapy should be considered in all stage I tumors (except in those ≤ 5 mm, with an excellent prognosis without CT) [106], administration of systemic neoadjuvant therapy could yield locoregional benefits and offer response information (Fig. 3).
Nevertheless, when upfront surgery and adjuvant CT is the preferred option, the regimen should include an anthracycline and a taxane (I, B), although a taxane/cyclophosphamide or taxane/platinum combination can represent a good alternative in patients with potential cardiac toxicity (I, B). CT should be discussed with patients with pT1b N0 (6–10 mm) tumors, weighing potential risks and benefits in this good prognosis group [106] (III, B).
Neoadjuvant treatment for triple‐negative disease
NST with CT or NAC is the preferred approach in locally advanced (stage II-III) TNBC, leading classically to pCR rates of 30–40%. Patients who achieve a pCR have an excellent prognosis. Residual disease after NAC is a recognized biomarker associated with an increased recurrence risk that can be very useful when selecting patients for post-neoadjuvant escalating therapies.
The combination of anthracyclines and taxanes is the treatment of choice (I, A), preferably with dose-dense sequential regimens [77]. The addition of platinum compounds to standard sequential anthracycline and taxane regimens has largely remained a controversial issue. Overall, based on the results of a meta-analysis that included nine randomized controlled trials investigating platinum-based versus platinum-free NAC in TNBC, an increase in pCR from 37.0 to 52.1% was observed with platinum-based regimens [107]. While none of these studies were designed to determine benefit in DFS or OS, the recently published long-term results of the Brightness trial have confirmed that improved pCR rates with the addition of carboplatin were associated with long-term EFS benefit, including in BRCA1/2 carriers [108] (I, B).
The recent incorporation of immunotherapy to NAC regimens for TNBC has changed the “chemotherapy-only” neoadjuvant approach in these patients. In the phase III KEYNOTE-522 trial, the addition of pembrolizumab demonstrated a significantly higher pCR rate (64.8% vs 51.2%) and 18-month EFS (91.3% vs. 85.4%) [109] (I, B). Although the PD-L1-positive subgroup had higher overall pCR rates, benefit was observed regardless of PD-L1 expression. The smaller phase III trial, IMpassion031, that evaluated atezolizumab as the immunotherapy agent, has confirmed a similar benefit in pCR rates [110] but without any significan impact in EFS.
As stated above, patients with residual disease after NAC have a significant risk of disease recurrence, particularly in the first 2–3 years following diagnosis. In the postneoadjuvant setting, the administration of 6–8 cycles of capecitabine represents a good therapeutic option, based on the results of the CREATE-X trial (9) and a recently published meta-analysis [111] (I, B). In the Olympia trial BRCA1/2 mutation carriers with TNBC treated with NAC who did not achieve a pCR derived a significant increase in DFS with 1 year of adjuvant olaparib (I, B) [112]. In patients treated with neoadjuvant pembrolizumab according to the Keynote-522 regimen, pembrolizumab should be administered as adjuvant treatment, although its value in patients obtaining near-pathological complete response (RCB 0 or I) is unclear (I, B) [109].
Follow-up, long-term implications, and survivorship
Breast cancer follow-up should focus on detecting disease relapse or second primary neoplasms. Although there is no universal sequence or protocol for the follow-up of these patients, taking into account both patient needs and follow-up costs, regular visits are recommended every 3–6 months in the first 2 years, every 6 months after 3–5 years, and annually thereafter (III, A). As part of monitoring, each visit should include a thorough anamnesis, record of symptoms, and a physical examination. Annual ipsilateral (after BCS) and/or contralateral mammography (after mastectomy) is recommended (II, A). A magnetic resonance imaging of the breast may be indicated for young patients, especially in cases of dense breast tissue and genetic or familial predisposition [113] (II, B). Ultrasound may be considered only as an additional study under the indication of a radiologist in doubtful cases or when there is a contraindication for MRI; contrast-enhanced mammography might also be indicated in these cases (III, B) [114]. Routine imaging of reconstructed breast is not indicated.
HR positive/HER2-negative early breast cancer algorithm. AI: aromatase inhibitors; BCS: breast conservation; CT: chemotherapy; ET: endocrine therapy; N: axillar node; OFS: ovarian function suppression; y: years; +: positive; -: negative. *Consider in premenopausal patients with luminal A-like tumors and no indication for chemotherapy, who are not candidates for optimal surgery, OFS plus an aromatase inhibitor can be considered
There are no data to indicate that either laboratory or imaging tests or any tumor markers, such as cancer antigen 15–3 (CA15-3) or carcinoembryonic antigen (CEA), result in a survival benefit (I, D). In symptomatic patients or in the case of abnormal findings on examination, appropriate and specific tests should be performed immediately (III, A) [114, 115].
It is also important to evaluate and manage the toxicities of the treatment received, both physical and psychosocial, in the short and long term. Patients on tamoxifen treatment will require age-appropriate gynecological screening. Those on an aromatase inhibitor or who experience ovarian failure secondary to treatment should undergo monitoring of bone health with a bone mineral density determination at baseline and periodically thereafter [115]. And finally, healthy lifestyle habits, such as an active lifestyle (II, B), a healthy diet, limited alcohol consumption, and achieving and maintaining an ideal body weight (20–25 BMI) can lead to optimal breast cancer outcomes and improved quality of life [114, 115].
Data availability
All data supporting the findings of this study are available within the paper.
Change history
30 October 2023
A Correction to this paper has been published: https://doi.org/10.1007/s12094-023-03334-y
Abbreviations
- AI:
-
Aromatase inhibitor
- ALND:
-
Axillary lymph node dissection
- BC:
-
Breast cancer
- BCS:
-
Breast conserving surgery
- CT:
-
Chemotherapy
- DFS:
-
Disease-free survival
- EFS:
-
Event-free survival
- ER:
-
Estrogen receptor
- ET:
-
Endocrine therapy
- GEICAM:
-
Grupo Español de Investigación en Cáncer de Mama (Spanish Group for Breast Cancer Research)
- HR:
-
Hormone receptor
- iDFS:
-
Invasive disease-free survival
- MRI:
-
Magnetic resonance imaging
- NAC:
-
Neoadjuvant chemotherapy
- NET:
-
Neoadjuvant endocrine therapy
- NST:
-
Neoadjuvant systemic therapy
- OFS:
-
Ovarian function suppression
- OS:
-
Overall survival
- PgR:
-
Progesterone receptor
- pCR:
-
Pathologic complete response
- SLNB:
-
Sentinel lymph node biopsy
- SOLTI:
-
Grupo español de estudio, tratamiento y otras estrategias experimentales en tumores sólidos (Spanish group of study, treatment and other experimental strategies in solid tumors)
- SEOM:
-
Sociedad Española de Oncología Médica (Spanish Society of Medical Oncology)
- TNBC:
-
Triple negative breast cancer
- WBI:
-
Whole breast irradiation
References
Sociedad Española de Oncología Médica (SEOM), Red Española de Registros del Cáncer (REDECAN). Las cifras del cáncer en España (2022). In: https://seom.org/images/LAS_CIFRAS_DEL_CANCER_EN_ESPANA_2022.pdf. Accessed 10 Nov 2022.
Bosch G, Posso M, Louro J, Roman M, Porta M, Castells X, et al. Impact of the COVID-19 pandemic on breast cancer screening indicators in a Spanish population-based program: a cohort study. Elife. 2022;11:1–16.
Khan AR, Khan S, Zimmerman V, Baddour LM, Tleyjeh IM. Quality and strength of evidence of the Infectious Diseases Society of America clinical practice guidelines. Clin Infect Dis. 2010;51:1147–56.
Giuliano AE, Connolly JL, Edge SB, Mittendorf EA, Rugo HS, Solin LJ, et al. Breast cancer-major changes in the american joint committee on cancer eighth edition cancer staging manual. Cancer J Clin. 2017;67:290–303.
Perry N, Broeders M, de Wolf C, Tornberg S, Holland R, von Karsa L. European guidelines for quality assurance in breast cancer screening and diagnosis. Fourth edition–summary document. Ann Oncol. 2007;19:614–22.
Sardanelli F, Boetes C, Borisch B, Decker T, Federico M, Gilbert FJ, et al. Magnetic resonance imaging of the breast: recommendations from the EUSOMA working group. Eur J Cancer. 2010;46:1296–316.
López-Fernández T, Martín García A, Santaballa Beltrán A, Montero Luis Á, García Sanz R, Mazón Ramos P. Cardio-onco-hematology in clinical practice. Position paper recommendations. Rev Esp Cardiol. 2017;70(6):47.
Louie RJ, Tonneson JE, Gowarty M, Goodney PP, Barth RJ, Rosenkranz KM. Complete blood counts, liver function tests, and chest x-rays as routine screening in early-stage breast cancer: value added or just cost? Breast Cancer Res Treat. 2015;154:99–103.
Robertson IJ, Hand F, Kell MR. FDG-PET/CT in the staging of local/regional metastases in breast cancer. Breast. 2011;20:491–4.
Koolen BB, Vrancken Peeters MJTFD, Aukema TS, Vogel VW, Oldenburg HSA, Hage JA. 18F-FDG PET/CT as a staging procedure in primary stage II and III breast cancer: Comparison with conventional imaging techniques. Breast Cancer Res Treat. 2012;131:117–26.
Lakhani SR, Ellis IO, Schnitt SJ, Tan PH, van de Vijver MJ (Ed.). WHO Classification of Tumours of the Breast. World Health Organization Classification of tumours. Lyon, France; International Agency for Research on Cancer; 2012.
Tan PH, Ellis I, Allison K, Brogi E, Fox SB, Lakhani S. The 2019 world health organization classification of tumours of the breast. Histopathology. 2020;77:181–5.
Allison KH, Hammond EH, Dowsett M, McKermin SE, Carey LA, Fitzgibbons PL, et al. Estrogen and progesterone receptor testing in breast cancer: ASCO/CAP guideline update. J Clin Oncol. 2020;38:1346–66.
Wolff AC, McShane LM, Hammond MEH, Allison KH, Fitzgibbons P, Press MF. Human epidermal growth factor receptor 2 testing in breast cancer: American Society of Clinical Oncology/College of American Pathologists clinical practice guideline focused update. Arch Pathol Lab Med. 2018;142:1364–82.
Nielsen TO, Leung SCY, Rimm DL, Dodson A, Acs B, Badve S. Assessment of Ki67 in breast cancer: updated recommendations from the international ki67 in breast cancer working group. JNCI J Natl Cancer Inst. 2021;113:808–19.
Denkert C, Minckwitz G, Darb-Esfahani S, Lederer B, Heppner BI, Weber KE. Tumour-infiltrating lymphocytes and prognosis in different subtypes of breast cancer: a pooled analysis of 3771 patients treated with neoadjuvant therapy. Lancet Oncol. 2018;19:40–50.
Wein L, Savas P, Luen SJ, Virassamy B, Salgado R, Loi S. Clinical validity and utility of tumor-infiltrating lymphocytes in routine clinical practice for breast cancer patients: current and future directions. Front Oncol. 2017;7:156.
Balic M, Thomssen C, Würstlein R, Gnant M, Harbeck N. St. Gallen/Vienna 2019: A brief summary of the consensus discussion on the optimal primary breast cancer treatment. Breast Care (Basel). 2019;(14):103–10.
Sparano JA, Gray RJ, Makower DF, Pritchard KI, Albain KS, Hayes DF, et al. Adjuvant chemotherapy guided by a 21-gene expression assay in breast cancer. N Engl J Med. 2018;379:111–21.
Piccart M, Van’t Veer L, Poncet C, Lopes Cardozo J, Delaloge S, Pierga J, et al. 70-gene signature as an aid for treatment decisions in early breast cancer: updated results of the phase 3 randomised MINDACT trial with an exploratory analysis by age. Lancet Oncol. 2021;22:476–88.
Kevin Kalinsky MD, Barlow WE. 21- gene assay to inform chemotherapy benefit in node-positive breast cancer. N Engl J Med. 2021;385:2336–47.
Prat A, Guarneri V, Pascual T, Brasó-Maristany F, Sanfeliu E, Paré L. Development and validation of the new HER2DX assay for predicting pathological response and survival outcome in early-stage HER2-positive breast cancer. Lancet Oncol. 2022;25:1–5.
Tolaney SM, Tarantino P, Graham N, Tayob N, Parè L, Villacampa G et al. Adjuvant paclitaxel and trastuzumab for node-negative, HER2-positive breast cancer: final 10-year analysis of the open-label, single-arm, phase 2 APT trial. Lancet Oncol. 2023;24(3):273–85. https://doi.org/10.1016/S1470-2045(23)00051-7.
Bueno-Muiño C, Echavarría I, López-Tarruella S, Roche-Molina M, Del Monte-Millán M, Massarrah T et al. Assessment of a genomic assay in patients with ERBB2-positive breast cancer following neoadjuvant trastuzumab-based chemotherapy with or without Pertuzumab. JAMA Oncol. 2023;27:e230187. https://doi.org/10.1001/jamaoncol.2023.0187.
Waks AG, Ogayo ER, Paré L, Marín-Aguilera M, Brasó-Maristany F, Galván P et al. Assessment of the HER2DX Assay in Patients With ERBB2-Positive Breast Cancer Treated With Neoadjuvant Paclitaxel, Trastuzumab, and Pertuzumab. JAMA Oncol. 2023;27:e230181. https://doi.org/10.1001/jamaoncol.2023.0181.
Kimball CC, Nichols CI, Vose JG, Peled AW. Trends in lumpectomy and oncoplastic breast conserving surgery in the US, 2011–2016. Ann Surg Oncol. 2018;25:3867–73.
Lautner M, Lin H, Shen Y, Parker C, Kuerer H, Shaitelman S, et al. Disparities in the use of breast-conserving therapy among patients with early-stage breast cancer. JAMA Surg. 2015;150:778–86.
Carter SA, Lyons GR, Kuerer HM, Bassett RL, Oates Thompson SA, et al. Operative and oncologic outcomes in 9861 patients with operable breast cancer: single-institution analysis of breast conservation with oncoplastic reconstruction. Ann Surg Oncol. 2016;23:3190–8.
Jonczyk MM, Jean J, Graham R, Chatterjee A. Surgical trends in breast cancer: a rise in novel operative treatment options over a 12 year analysis. Breast Cancer Res Treat. 2019;173(2):267–74.
Burstein HJ, Curigliano G, Loibl S, Dubsky P, Gnant M, Poortmans P, et al. Estimating the benefits of therapy for early-stage breast cancer: The St. Gallen international consensus guidelines for the primary therapy of early breast cancer 2019. Ann Oncol. 2019;30:1541–57.
Tung NM, Boughey JC, Pierce LJ, Robson ME, Bedrosian I, Dietz JRD, et al. Management of hereditary breast cancer: american society of clinical oncology, american society for radiation oncology, and society of surgical society of surgical oncology guideline. J Clin Oncol. 2020;38:2080–106.
Giuliano AE, Ballman KV. Effect of axillary dissection vs no axillary dissection on 10-year overall survival among women with invasive breast cancer and sentinel node metastasis: the ACOSOG Z0011 (Alliance) randomized clinical trial. JAMA. 2017;318:918–26.
Donker M, van Tienhoven G, Straver ME, Meijnen P, van de Velde CJH, Mansel RE, et al. Radiotherapy or surgery of the axilla after a positive sentinel node in breast cancer (EORTC 10981–22023 AMAROS): a randomised, multicentre, open-label, phase 3 non-inferiority trial. Lancet Oncol Elsevier. 2014;15:1303–10.
Bernet L, Piñero A, Martínez M, Sicart SV, Algara M, Palomares E. Consenso de la Sociedad Española de Senología y Patología Mamaria (SESPM) sobre la biopsia selectiva del ganglio centinela (BSGC) y el manejo axilar en el cáncer de mama (2022). Rev Senol y Patol Mamar. 2022;35:243–59.
Simons JM, Nijnatten TJA, CC P. Diagnostic accuracy of different surgical procedures for axillary staging after neoadjuvant systemic therapy in node-positive breast cancer: a systematic review and meta-analysis. Ann Surg. 2019;269:432–42.
Banys-Paluchowski M, Gasparri ML, Boniface J, Gentilini O, Stickeler E, Hartmann S, et al. Surgical management of the axilla in clinically node-positive breast cancer patients converting to clinical node negativity through neoadjuvant chemotherapy: current status, knowledge gaps, and rationale for the EUBREAST-03 AXSANA study. Cancers. 2021;13(7):1.
Shah C, Al-Hilli Z, Vicini F. Advances in breast cancer radiotherapy: implications for current and future practice. JCO Oncol Pr. 2021;17:697–706.
Shah C, Bauer-Nilsen K, McNulty RH, Vicini F. Novel radiation therapy approaches for breast cancer treatment. Semin Oncol. 2020;47:209–16.
Brunt AM, Haviland JS, Wheatley DA. Hypofractionated breast radiotherapy for 1 week versus 3 weeks (FAST-Forward): 5-year efficacy and late normal tissue effects results from a multicenter, non-inferiority, randomised, phase 3 trial. Lancet. 2020;395:1613–26.
Kunkler IH, Chir B, Williams LJ, Jack WJL, Cameron DA, Dixon JM. Breast-conserving surgery with or without irradiation in early breast cancer. N Engl J Med. 2023;388:585–94.
Whelan TJ, Olivotto IA, Parulekar WR. Regional nodal irradiation in early-stage breast cancer. N Engl J Med. 2015;373:307–16.
Andre F, Ismaila N, K A. Biomarkers for adjuvant endocrine and chemotherapy in early-stage breast cancer: ASCO guideline update. J Clin Oncol. 2022;40:1816–34.
Paik S, Shak S, Tang G, Kim C, Baker J, Cronin M, et al. A Multigene assay to predict recurrence of tamoxifen-treated, node-negative breast cancer. N Engl J Med. 2004;351:2817–26.
Paik S, Tang G, Shak S, Kim C, Baker J, Kim W, et al. Gene expression and benefit of chemotherapy in women with node-negative, estrogen receptor-positive breast cancer. J Clin Oncol. 2006;24:3726–34.
Cardoso F, Van’t Veer LJ, Bogaerts J, Slaets L, Viale G, Delaloge S, et al. 70-gene signature as an aid to treatment decisions in early-stage breast cancer. N Engl J Med. 2016;375:717–29.
Sparano JA, Gray RJ, Makower DF, Pritchard KI, Albain KS, Hayes DF, et al. Prospective validation of a 21-gene expression assay in breast cancer. N Engl J Med. 2015;373:2005–14.
Albain KS, Barlow WE, Shak S, Hortobagyi GN, Livingston RB, Yeh I-T, et al. Prognostic and predictive value of the 21-gene recurrence score assay in postmenopausal women with node-positive, oestrogen-receptor-positive breast cancer on chemotherapy: a retrospective analysis of a randomised trial. Lancet Oncol. 2010;11:55–65.
Lænkholm A-V, Jensen M-B, Eriksen JO, Rasmussen BB, Knoop AS, Buckingham W, et al. PAM50 risk of recurrence score predicts 10-year distant recurrence in a comprehensive Danish cohort of postmenopausal women allocated to 5 years of endocrine therapy for hormone receptor-positive early breast cancer. J Clin Oncol. 2018;36:735–40.
Dubsky P, Brase JC, Jakesz R, Rudas M, Singer CF, Greil R, et al. The EndoPredict score provides prognostic information on late distant metastases in ER+/HER2− breast cancer patients. Br J Cancer. 2013;109:2959–64.
Kalinsky K, Barlow WE, Gralow J, Meric-Bernstam F, Albain K, Hayes DF. 21-gene assay to inform chemotherapy benefit in node-positive breast cancer. N Engl J Med. 2021;385:2336–47.
Gnant M, Filipits M, Greil R, Stoeger H, Rudas M, Bago-Horvath Z, et al. Predicting distant recurrence in receptor-positive breast cancer patients with limited clinicopathological risk: using the PAM50 risk of recurrence score in 1478 postmenopausal patients of the ABCSG-8 trial treated with adjuvant endocrine therapy alone. Ann Oncol. 2014;25:339–45.
Smith I, Robertson J, Kilburn L, Wilcox M, Evans A, Holcombe C, et al. Long-term outcome and prognostic value of Ki67 after perioperative endocrine therapy in postmenopausal women with hormone-sensitive early breast cancer (POETIC): an open-label, multicentre, parallel-group, randomised, phase 3 trial. Lancet Oncol. 2020;21:1443–54.
Bradley R, Burrett J, Clarke M, Davies C, Duane F, Evans V, et al. Aromatase inhibitors versus tamoxifen in early breast cancer: Patient-level meta-analysis of the randomised trials. Lancet. 2015;386:1341–52.
Lohrisch C, Paltiel C, Gelmon K. Impact on survival of time from definitive surgery to initiation of adjuvant chemotherapy for early-stage breast cancer. J Clin Oncol. 2006;24:4888–94.
Early Breast Cancer Trialists. Collaborative group (EBCTCG). Effects of chemotherapy and hormonal therapy for early breast cancer on recurrence and 15 year survival: an overview of the randomised trials. Lancet. 2005;365:1687–717.
Davies C, Pan H, Godwin J, Gray R, Arriagada R, Raina V, et al. Long-term effects of continuing adjuvant tamoxifen to 10 years versus stopping at 5 years after diagnosis of oestrogen receptor-positive breast cancer: ATLAS, a randomised trial. Lancet. 2013;381:805–16.
Gray R, Rea D, Handley D, Bowden S, Perry P. aTTom: long-term effects of continuing adjuvant tamoxifen to 10 years versus stopping at 5 years in 6953 women with early breast cancer. J Clin Oncol. 2013. https://doi.org/10.1200/jco.2013.31.15_suppl.5.
Francis PA, Pagani O, Fleming GF, Walley BA, Colleoni M, Láng I, et al. Tailoring adjuvant endocrine therapy for premenopausal breast cancer. N Engl J Med. 2018;379:122–37.
Cuzick J, Ambroisine L, Davidson N, Jakesz R, Kaufmann M, LHRH-agonists in Early Breast Cancer Overview group, et al. Use of luteinising-hormone-releasing hormone agonists as adjuvant treatment in premenopausal patients with hormone-receptor-positive breast cancer: a meta-analysis of individual patient data from randomised adjuvant trials. Lancet. 2007;369:1711–23.
Howell A, Cuzick J, Baum M, Buzdar A, Dowsett M, Forbes JF, et al. Results of the ATAC (Arimidex, Tamoxifen, Alone or in Combination) trial after completion of 5 years’ adjuvant treatment for breast cancer. Lancet. 2005;365:60–2.
Mouridsen H, Giobbie-Hurder A, Goldhirsch A, Thürlimann B, Paridaens R, BIG 1-98 Collaborative Group, et al. Letrozole therapy alone or in sequence with tamoxifen in women with breast cancer. N Engl J Med. 2009;361:766–76.
Derks MGM, Blok EJ, Seynaeve C, Nortier JWR, Kranenbarg EM-K, Liefers G-J, et al. Adjuvant tamoxifen and exemestane in women with postmenopausal early breast cancer (TEAM): 10 year follow-up of a multicentre, open-label, randomised, phase 3 trial. Lancet Oncol. 2017;18:1211–20.
Boccardo F, Rubagotti A, Puntoni M, Guglielmini P, Amoroso D, Fini A, et al. Switching to anastrozole versus continued tamoxifen treatment of early breast cancer: preliminary results of the Italian tamoxifen anastrozole trial. J Clin Oncol. 2005;23:5138–47.
Coombes RC, Hall E, Gibson LJ, Paridaens R, Jassem J, Delozier T, et al. A randomized trial of exemestane after two to three years of tamoxifen therapy in postmenopausal women with primary breast cancer. N Engl J Med. 2004;350:1081–92.
Jakesz R, Jonat W, Gnant M, Mittlboeck M, Greil R, Tausch C, et al. Switching of postmenopausal women with endocrine-responsive early breast cancer to anastrozole after 2 years’ adjuvant tamoxifen: combined results of ABCSG trial 8 and ARNO 95 trial. The Lancet. 2005;366:455–62.
Corona SP, Roviello G, Strina C. Efficacy of extended aromatase inhibitors for hormone-receptor-positive breast cancer: A literature-based meta-analysis of randomized trials. Breast. 2019;46:19–24.
Zhang Y, Schroeder BE, Jerevall PL. A novel Breast Cancer Index for prediction of distant recurrence in HR+ early-stage breast cancer with one to three positive nodes. Clin Cancer Res. 2017;23:7217–24.
Sgroi DC, Sestak I, Cuzick J. Prediction of late distant recurrence in patients with oestrogen-receptor-positive breast cancer: a prospective comparison of the breast-cancer index (BCI) assay, 21-gene recurrence score, and IHC4 in the TransATAC study population. Lancet Oncol. 2013;14:1067–76.
Bartlett JMS, Sgroi DC, Treuner K. Breast Cancer Index and prediction of benefit from extended endocrine therapy in breast cancer patients treated in the adjuvant tamoxifen-to offer more? (aTTom) trial. Ann Oncol. 2019;30:1776–83.
Dhesy-Thind S, Fletcher GG, Blanchette PS, Clemons MJ, Dillmon MS, Frank ES, et al. Use of adjuvant bisphosphonates and other bone-modifying agents in breast cancer: a Cancer Care Ontario and American Society of Clinical Oncology clinical practice guideline. J Clin Oncol. 2017;35:2062–81.
Johnston S, Harbeck N, Hegg R. Abemaciclib combined with endocrine therapy for the adjuvant treatment of HR+, HER2−, node-positive, high-risk, early breast cancer (monarchE). J Clin Oncol. 2020;38:3987–98.
Andrew Tutt NJ, MB, Ch B JEG. Adjuvant olaparib for patients with BRCA1- or BRCA2-mutated breast cancer. N Engl J Med. 2021;384:2394–405.
Curigliano G, Burstein HJ, Winer EP, Gnant M, Dubsky P, Loibl S, et al. De-escalating and escalating treatments for early-stage breast cancer: The St Gallen international expert consensus conference on the primary therapy of early breast cancer. Ann Oncol. 2017;28:1700–12.
Nitz U, Gluz O, Huober J. Final analysis of the prospective WSGAGO EC-doc versus FEC phase III trial in intermediate-risk (pN1) early breast cancer: efficacy and predictive value of Ki67 expression. Ann Oncol. 2017;28:2899.
Samuel JA, Wilson JW, Bandos H. Abstract S3–02: nSABP B-36: a randomized phase III trial comparing six cycles of 5-fluorouracil (5-FU), epirubicin, and cyclophosphamide (FEC) to four cycles of Adriamycin and cyclophosphamide (AC) in patients (pts) with node negative breast cancer. Cancer Res. 2015;75:3–02.
Jones S, Holmes FA, O’Shaughnessy J. Shaughness. Docetaxel with cyclophosphamide is associated with an overall survival benefit compared with doxorubicin and cyclophosphamide: 7 year follow-up of US. J Clin Oncol. 2009;27:1177–83.
Early Breast Cancer Trialists. Collaborative Group (EBCTCG). Increasing the dose intensity of chemotherapy by more frequent administration or sequential scheduling: a patient-level meta-analysis of 37 298 women with early breast cancer in 26 randomised trials. Lancet. 2019;393:1440–52.
Peto R, Davies C, J G,. Comparisons between different polychemotherapy regimens for early breast cancer: meta-analyses of longterm outcome among 100,000 women in 123 randomised trials. Lancet. 2012;379:432–44.
Eggemann H, Ignatov A, Smith BJ. Adjuvant therapy with tamoxifen compared to aromatase inhibitors for 257 male breast cancer patients. Breast Cancer Res Treat. 2013;137:465–70.
Korde LA, Zujewski JA, Kamin L, Sousa B, Moser E, Cardoso F. Multidisciplinary meeting on male breast cancer: summary and research recommendations. J Clin Oncol. 2010;28:2114–22.
Sousa B, Moser E, Cardoso F. An update on male breast cancer and future directions for research and treatment. Eur J Pharmacol. 2013;717:71–83.
Gianni L, Baselga J, Eiermann W. Phase III trial evaluating the addition of paclitaxel to doxorubicin followed by cyclophosphamide, methotrexate, and fluorouracil, as adjuvant or primary systemic therapy: European cooperative trial in operable breast cancer. J Clin Oncol. 2009;27:2474–81.
Smith IE, Dowsett M, Ebbs SR, Dixon JM, Skene A, Blohmer J-U, et al. Neoadjuvant treatment of postmenopausal breast cancer with anastrozole, tamoxifen, or both in combination: the immediate preoperative anastrozole, tamoxifen, or combined with tamoxifen (IMPACT) multicenter double-blind randomized trial. J Clin Oncol. 2005;23:5108–16.
Dowsett M, Ellis MJ, Dixon JM, Gluz O, Robertson J, Kates R, et al. Evidence-based guidelines for managing patients with primary ER+ HER2- breast cancer deferred from surgery due to the COVID-19 pandemic. NPJ Breast Cancer. 2020;6:21.
Masuda N, Sagara Y, Kinoshita T. Neoadjuvant anastrozole versus tamoxifen in patients receiving goserelin for premenopausal breast cancer (STAGE): a double-blind, randomised phase 3 trial. Lancet Oncol. 2012;13:345–52.
Alba E, Calvo L, Albanell J, De la Haba JR, Arcusa Lanza A, Chacon JI, et al. Chemotherapy (CT) and hormonotherapy (HT) as neoadjuvant treatment in luminal breast cancer patients: results from the GEICAM/2006–03, a multicenter, randomized, phase-II study. Ann Oncol. 2012;23:3069–74.
Ellis MJ, Suman VJ, Hoog J, Lin L, Snider J, Prat A, et al. Randomized phase II neoadjuvant comparison between letrozole, anastrozole, and exemestane for postmenopausal women with estrogen receptor-rich stage 2 to 3 breast cancer: clinical and biomarker outcomes and predictive value of the baseline PAM50-based intrinsic subtype–ACOSOG Z1031. J Clin Oncol. 2011;29:2342–9.
Prat A, Galvan P, Jimenez B, Buckingham W, Jeiranian HA, Schaper C, et al. Prediction of response to neoadjuvant chemotherapy using core needle biopsy samples with the prosigna assay. Clin Cancer Res. 2016;22:560–6.
Cortazar P, Zhang L, Untch M, Mehta K, Costantino JP, Wolmark N, et al. Pathological complete response and long-term clinical benefit in breast cancer: the CTNeoBC pooled analysis. Lancet. 2014;384:164–72.
Gianni L, Pienkowski T, Im Y-H, Roman L, Tseng L-M, Liu M-C, et al. Efficacy and safety of neoadjuvant pertuzumab and trastuzumab in women with locally advanced, inflammatory, or early HER2-positive breast cancer (NeoSphere): a randomised multicentre, open-label, phase 2 trial. Lancet Oncol. 2012;13:25–32.
Swain SM, Miles D, Kim SB, Im Y, Im S, Semiglazov V, et al. Pertuzumab, trastuzumab, and docetaxel for HER2-positive metastatic breast cancer (CLEOPATRA): end-of-study results from a double-blind, randomised, placebo-controlled, phase 3 study. Lancet Oncol 2020; 21: 519–30.
Voort A, Ramshorst M, Werkhoven E, Mandjes I, Kemper I, Vulink A, et al. Three-year follow-up of neoadjuvant chemotherapy with or without anthracyclines in the presence of dual HER2-blockade for HER2-positive breast cancer (TRAIN-2): a randomized phase 3 trial. JAMA Oncol. 2021;7:978–84.
Schneeweiss A, Chia S, Hickish T, Harvey V, Eniu A, Hegg R, et al. Pertuzumab plus trastuzumab in combination with standard neoadjuvant anthracycline-containing and anthracycline-free chemotherapy regimens in patients with HER2-positive early breast cancer: a randomized phase II cardiac safety study (TRYPHAENA). Ann Oncol. 2013;24:2278–84.
Slamon D, Eiermann W, Robert N, Pienkowski T, Martin M, Press M, et al. Adjuvant trastuzumab in HER2-positive breast cancer. N Engl J Med. 2011;365:1273–83.
Cameron D, Piccart-Gebhart MJ, Gelber RD, Procter M, Goldhirsch A, de Azambuja E, et al. 11 years’ follow-up of trastuzumab after adjuvant chemotherapy in HER2-positive early breast cancer: final analysis of the HERceptin Adjuvant (HERA) trial. Lancet. 2017;389:1195–205.
Perez EA, Romond EH, Suman VJ, Jeong J-H, Sledge G, Geyer CE, et al. Trastuzumab plus adjuvant chemotherapy for human epidermal growth factor receptor 2–positive breast cancer: planned joint analysis of overall survival from NSABP B-31 and NCCTG N9831. J Clin Oncol. 2014;32:3744–52.
Inno A, Barni S, Ghidini A. One year versus a shorter duration of adjuvant trastuzumab for HER2-positive early breast cancer: a systematic review and meta-analysis. Breast Cancer Res Treat. 2019;173:247–54.
Niraula S, Gyawali B. Optimal duration of adjuvant trastuzumab in treatment of early breast cancer: a meta-analysis of randomized controlled trials. Breast Cancer Res Treat. 2019;173:103–9.
Tolaney SM, Guo H, Pernas S. Seven-year follow-up analysis of adjuvant paclitaxel and trastuzumab trial for node-negative, human epidermal growth factor receptor 2-positive breast cancer. J Clin Oncol. 2019;37:1868–75.
Piccart M, Procter M, Fumagalli D, De Azambuja E, Clark E, Ewer MS, et al. Adjuvant pertuzumab and trastuzumab in early HER2-positive breast cancer in the APHINITY trial: 6 years’ follow-up. J Clin Oncol. 2021;39:1448–57.
Loibl S, Jassem J, Sonnenblick A, Parlier D, Winer E, Bergh J, et al. Adjuvant pertuzumab and trastuzumab in patients with early HER-2 positive breast cancer in APHINITY: 84 years’ follow-up. ESMO Virtual Plenary. 2022. https://doi.org/10.1016/j.annonc.2022.06.009.
Arlene MB, Mansi J. Final efficacy results of neratinib in HER2-positive hormone receptorpositive early-stage breast cancer from the phase III ExteNET trial. Clin Breast Cancer. 2021;21:80–91.
Minckwitz G, Huang CS, Mano MS, Loibl S, Mamounas EP, Untch M, et al. Trastuzumab emtansine for residual invasive HER2-positive breast cancer. N Engl J Med. 2019;380(7):617–28.
Perou CM, Sørlie T, Eisen MB, van de Rijn M, Jeffrey SS, Rees CA, et al. Molecular portraits of human breast tumours [Letter]. Nature. 2000;406:747–52.
Vagia E, Mahalingam D, Cristofanilli M. The landscape of targeted therapies in TNBC. Cancers. 2020. https://doi.org/10.3390/cancers12040916.
An X, Lei X, Huang R. Adjuvant chemotherapy for small, lymph node-negative, triple-negative breast cancer: a single-center study and a meta-analysis of the published literature. Cancer. 2020;126:3837–46.
Poggio F, Bruzzone M, Ceppi M, Pondé N, La Valle G, Del Mastro L, et al. Platinum-based neoadjuvant chemotherapy in triple-negative breast cancer: a systematic review and metaanalysis. Ann Oncol. 2018;29:1497–508.
Geyer C, Sikov W, Huober J, Rugo H, Wolmark N, O’Shaughnessy J, et al. Long-term efficacy and safety of addition of carboplatin with or without veliparib to standard neoadjuvant chemotherapy in triple-negative breast cancer: 4-year follow-up data from BrighTNess, a randomized phase III trial. Ann Oncol. 2022;33:384–94.
Schmid P, Cortes J, Dent R. Event-free survival with pembrolizumab in early triple-negative breast cancer. N Engl J Med. 2022;386:556–67.
Mittendorf EA, Zhang H, Barrios CH. Neoadjuvant atezolizumab in combination with sequential nab-paclitaxel and anthracycline-based chemotherapy versus placebo and chemotherapy in patients with early-stage triple-negative breast cancer (IMpassion031): a randomised, double- blind, phase 3 tri. Lancet. 2020;396:1090–100.
Mackelenbergh M, Seither F, Möbus V, O’Shaughnessy J, Martin M, Joensuu H, et al. Effects of capecitabine as part of neo-/adjuvant chemotherapy. A meta-analysis of individual patient data from 12 randomized trials including 15,457 patients. Eur J Cancer. 2022;166:185–201.
Tutt A, Garber J, Kaufman B. Adjuvant Olaparib for patients with BRCA1 or BRCA2 mutated breast cancer. N Engl J Med. 2021;384:2394–405.
Barnadas A, Algara M, Cordoba O, Casas A, Gonzalez M, Marzo M, et al. Recommendations for the follow-up care of female breast cancer survivors: a guideline of the Spanish Society of Medical Oncology (SEOM), Spanish Society of General Medicine (SEMERGEN), Spanish Society for Family and Community Medicine (SEMFYC), Spanish Society for General and Family Physicians (SEMG), Spanish Society of Obstetrics and Gynecology (SEGO), Spanish Society of Radiation Oncology (SEOR), Spanish Society of Senology and Breast Pathology (SESPM), and Spanish Society of Cardiology (SEC). Clin Transl Oncol. 2018;20:687–94.
Cardoso F, Kyriakides S, Ohno S, Penault-Llorca F, Poortmans P, Rubio IT, et al. Early breast cancer: ESMO Clinical Practice Guidelines for diagnosis, treatment and follow-up. Ann Oncol. 2019;30:1194–220.
NCCN Guidelines. Version 2.2021. Invasive Breast Cancer. 2021.
Acknowledgements
The authors thank César Rodriguez Sánchez and Juan de la Haba Rodríguez for their review and validation of the levels of evidence and grades of recommendation in this guideline.
Funding
Open Access funding provided thanks to the CRUE-CSIC agreement with Springer Nature.
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
Conflict of interest
FAP reports Speaker from Astra Zeneca, Novartis, Lilly, Sanofi and Daichii Sankyo; Speaker and Others from Celgene, Eisai and Pierre Fabre; Advisory Board—Speaker—Other from Pfizer and Roche; Advisory Board from Seagen; Other from MSD. JGG reports Advisory Board—Speaker—Non-financial Support from Daiichi Sankyo, AstraZeneca, Novartis, Roche and Pfizer; Speaker from lilly. FH reports Advisory from AstraZeneca, Daiichi-Sankyo, Novartis, Pfizer, Lilly and Roche. EC reports Advisory Board—Speaker from Roche, Lilly, Pfizer, AstraZeneca, Daichii Sankyo, Novartis, MSD and Gilead; Advisory Board from Reveal Genomics. MJVL, SAN, AS, LGC, CME, TMM have nothing to disclose.
Ethical approval
The current study has been performed in accordance with the ethical standards laid down in the 1964 Declaration of Helsinki and its later amendments.
Informed consent
No informed consent was required for this type of article.
Additional information
Publisher's Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
The original online version of this article was revised to correct Figure 3.
Rights and permissions
Open Access This article is licensed under a Creative Commons Attribution 4.0 International License, which permits use, sharing, adaptation, distribution and reproduction in any medium or format, as long as you give appropriate credit to the original author(s) and the source, provide a link to the Creative Commons licence, and indicate if changes were made. The images or other third party material in this article are included in the article's Creative Commons licence, unless indicated otherwise in a credit line to the material. If material is not included in the article's Creative Commons licence and your intended use is not permitted by statutory regulation or exceeds the permitted use, you will need to obtain permission directly from the copyright holder. To view a copy of this licence, visit http://creativecommons.org/licenses/by/4.0/.
About this article
Cite this article
Ayala de la Peña, F., Antolín Novoa, S., Gavilá Gregori, J. et al. SEOM-GEICAM-SOLTI clinical guidelines for early-stage breast cancer (2022). Clin Transl Oncol 25, 2647–2664 (2023). https://doi.org/10.1007/s12094-023-03215-4
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s12094-023-03215-4