Abstract
Purpose
The purpose of the study was to assess the utility of tumor biomarkers, ultrasound (US) and US-guided diffuse optical tomography (DOT) in early prediction of breast cancer response to neoadjuvant therapy (NAT).
Methods
This prospective HIPAA compliant study was approved by the institutional review board. Forty one patients were imaged with US and US-guided DOT prior to NAT, at completion of the first three treatment cycles, and prior to definitive surgery from February 2017 to January 2020. Miller-Payne grading was used to assess pathologic response. Receiver operating characteristic curves (ROCs) were derived from logistic regression using independent variables, including: tumor biomarkers, US maximum diameter, percentage reduction of the diameter (%US), pretreatment maximum total hemoglobin concentration (HbT) and percentage reduction in HbT (%HbT) at different treatment time points. Resulting ROCs were compared using area under the curve (AUC). Statistical significance was tested using two-sided two-sample student t-test with P < 0.05 considered statistically significant. Logistic regression was used for ROC analysis.
Results
Thirty-eight patients (mean age = 47, range 24–71 years) successfully completed the study, including 15 HER2 + of which 11 were ER + ; 12 ER + or PR + /HER2−, and 11 triple negative. The combination of HER2 and ER biomarkers, %HbT at the end of cycle 1 (EOC1) and %US (EOC1) provided the best early prediction, AUC = 0.941 (95% CI 0.869–1.0). Similarly an AUC of 0.910 (95% CI 0.810–1.0) with %US (EOC1) and %HbT (EOC1) can be achieved independent of HER2 and ER status. The most accurate prediction, AUC = 0.974 (95% CI 0.933–1.0), was achieved with %US at EOC1 and %HbT (EOC3) independent of biomarker status.
Conclusion
The combined use of tumor HER2 and ER status, US, and US-guided DOT may provide accurate prediction of NAT response as early as the completion of the first treatment cycle.
Clinical Trial Registration number: NCT02891681. https://clinicaltrials.gov/ct2/show/NCT02891681, Registration time: September 7, 2016


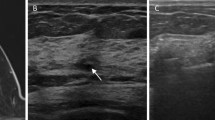
source laser diodes of 730 nm, 785 nm, 808 nm and 830 nm optical wavelengths were sequentially switched to nine source positions (pointed by an arrow) on the probe, while the reflected light was coupled by the 14 light guides (pointed by an arrow) to 14 parallel detectors




Similar content being viewed by others
Data availability
The patients’ clinicopathologic characteristics are given in Table 1. The datasets generated during and/or analyzed during the current study are available from the corresponding author on reasonable request.
Code availability
The code is available from the corresponding author on reasonable request.
Abbreviations
- NIR:
-
Near infrared
- pCR:
-
Pathological complete response
- ROI:
-
Region of interest
- ER:
-
Estrogen receptor
- PR:
-
Progesterone receptor
- HER2:
-
Human epidermal growth factor receptor 2
- TNBC:
-
Triple-negative breast cancer
- MP:
-
Miller-Payne grade
- RCB:
-
Residual cancer burden
- NAT:
-
Neoadjuvant therapy
- HbT:
-
Total hemoglobin
- ROC:
-
Receiver operating characteristic curve
- AUC:
-
Area under receiving operating characteristic curve
References
Cortazar P, Zhang L, Untch M, Mehta K, Costantino JP, Wolmark N, Bonnefoi H, Cameron D, Gianni L, Valagussa P, Swain SM, Prowell T, Loibl S, Wickerham DL, Bogaerts J, Baselga J, Perou C, Blumenthal G, Blohmer J, Mamounas EP, Bergh J, Semiglazov V, Justice R, Eidtmann H, Paik S, Piccart M, Sridhara R, Fasching PA, Slaets L, Tang S, Gerber B, Geyer CE Jr, Pazdur R, Ditsch N, Rastogi P, Eiermann W, von Minckwitz G (2014) Pathological complete response and long-term clinical benefit in breast cancer: the CTNeoBC pooled analysis. Lancet 384(9938):164–172. https://doi.org/10.1016/S0140-6736(13)62422-8
Gianni L, Pienkowski T, Im YH et al (2012) Efficacy and safety of neoadjuvant pertuzumab and trastuzumab in women with locally advanced, inflammatory, or early HER2-positive breast cancer (NeoSphere): a randomised multicentre, open-label, phase 2 trial. Lancet Oncol 13:25–32
Hurvitz SA, Martin M, Symmans WF, Jung KH, Huang CS, Thompson AM, Harbeck N, Valero V, Stroyakovskiy D, Wildiers H, Campone M, Boileau JF, Beckmann MW, Afenjar K, Fresco R, Helms HJ, Xu J, Lin YG, Sparano J, Slamon D (2018) Neoadjuvant trastuzumab, pertuzumab, and chemotherapy versus trastuzumab emtansine plus pertuzumab in patients with HER2-positive breast cancer (KRISTINE): a randomised, open-label, multicentre, phase 3 trial. Lancet Oncol 19(1):115–126. https://doi.org/10.1016/S1470-2045(17)30716-7
Schneeweiss A, Chia S, Hickish T et al (2013) Pertuzumab plus trastuzumab in combination with standard neoadjuvant anthracycline-containing and anthracycline-free chemotherapy regimens in patients with HER2-positive early breast cancer: a randomized phase II cardiac safety study (TRYPHAENA). Ann Oncol 24:2278–2284
Krystel-Whittemore M, Xu J, Brogi E, Ventura K, Patil S, Ross DS, Dang C, Robson M, Norton L, Morrow M, Wen HY (2019) Pathologic complete response rate according to HER2 detection methods in HER2-positive breast cancer treated with neoadjuvant systemic therapy. Breast Cancer Res Treat. https://doi.org/10.1007/s10549-019-05295-9
von Minckwitz G, Huang CS, Mano MS, Loibl S, Mamounas EP, Untch M, Wolmark N, Rastogi P, Schneeweiss A, Redondo A, Fischer HH, Jacot W, Conlin AK, Arce-Salinas C, Wapnir IL, Jackisch C, DiGiovanna MP, Fasching PA, Crown JP, Wülfing P, Shao Z, Rota Caremoli E, Wu H, Lam LH, Tesarowski D, Smitt M, Douthwaite H, Singel SM, Geyer CE Jr, KATHERINE Investigators (2019) Trastuzumab Emtansine for Residual Invasive HER2-Positive Breast Cancer. N Engl J Med 380(7):617–628. https://doi.org/10.1056/NEJMoa1814017
Lehmann BD, Jovanović B, Chen X, Estrada MV, Johnson KN, Shyr Y, Moses HL, Sanders ME, Pietenpol JA (2016) Refinement of triple-negative breast cancer molecular subtypes: implications for neoadjuvant chemotherapy selection. PLoS ONE 11(6):e0157368. https://doi.org/10.1371/journal.pone.0157368
Keune JD, Jeffe DB, Schootman M, Hoffman A, Gillanders WE, Aft RL (2010) Accuracy of ultrasonography and mammography in predicting pathologic response after neoadjuvant chemotherapy for breast cancer. Am J Surg 199(4):477–484. https://doi.org/10.1016/j.amjsurg.2009.03.012
Marinovich ML, Houssami N, Macaskill P, von Minckwitz G, Blohmer JU, Irwig L (2015) Accuracy of ultrasound for predicting pathologic response during neoadjuvant therapy for breast cancer. Int J Cancer 136(11):2730–2737. https://doi.org/10.1002/ijc.29323
Candelaria RP, Bassett RL, Symmans WF, Ramineni M, Moulder SL, Kuerer HM, Thompson AM, Yang WT (2017) Performance of mid-treatment breast ultrasound and axillary ultrasound in predicting response to neoadjuvant chemotherapy by breast cancer subtype. Oncologist 22:394–401
von Minckwitz G, Kümmel S, Vogel P, Hanusch C, Eidtmann H, Hilfrich J, Gerber B, Huober J, Costa SD, Jackisch C, Loibl S, Mehta K, Kaufmann M, German Breast Group (2008) Intensified neoadjuvant chemotherapy in early-responding breast cancer: phase III randomized GeparTrio study. J Natl Cancer Inst. 100:552–562
Baumgartner A, Tausch C, Hosch S, Papassotiropoulos B, Varga Z, Rageth C, Baege A (2018) Ultrasound-based prediction of pathologic response to neoadjuvant chemotherapy in breast cancer patients. Breast 39:19–23. https://doi.org/10.1016/j.breast.2018.02.028
Hayashi N, Tsunoda H, Namura M, Ochi T, Suzuki K, Yamauchi H, Nakamura S (2019) Magnetic resonance imaging combined with second-look ultrasonography in predicting pathologic complete response after neoadjuvant chemotherapy in primary breast cancer patients. Clin Breast Cancer 19(1):71–77. https://doi.org/10.1016/j.clbc.2018.08.004
Paydary K, Seraj SM, Zadeh MZ, Emamzadehfard S, Shamchi SP, Gholami S, Werner TJ, Alavi A (2019) The evolving role of FDG-PET/CT in the diagnosis, staging, and treatment of breast cancer. Mol Imaging Biol 21(1):1–10. https://doi.org/10.1007/s11307-018-1181-3
Sheikhbahaei S, Trahan TJ, Xiao J, Taghipour M, Mena E, Connolly RM (2016) Subramaniam RM FDG-PET/CT and MRI for evaluation of pathologic response to neoadjuvant chemotherapy in patients with breast cancer: a meta-analysis of diagnostic accuracy studies. Oncologist 21(8):931–939. https://doi.org/10.1634/theoncologist.2015-0353
Tromberg BJ, Zhang Z, Leproux A, O’Sullivan TD, Cerussi AE, Carpenter PM, Mehta RS, Roblyer D, Yang W, Paulsen KD, Pogue BW, Jiang S, Kaufman PA, Yodh AG, Chung SH, Schnall M, Snyder BS, Hylton N, Boas DA, Carp SA, Isakoff SJ, Mankoff D, ACRIN 6691 investigators (2016) Predicting responses to neoadjuvant chemotherapy in breast cancer: ACRIN 6691 trial of diffuse optical spectroscopic imaging. Cancer Res 76(20):5933–5944
Gunther JE, Lim EA, Kim HK, Flexman M, Altoé M, Campbell JA, Hibshoosh H, Crew KD, Kalinsky K, Hershman DL, Hielscher AH (2018) Dynamic diffuse optical tomography for monitoring neoadjuvant chemotherapy in patient. Radiology 287:778
Tank A, Peterson HM, Pera V, Tabassum S, Leproux A, O’Sullivan T, Jones E, Cabral H, Ko N, Mehta RS, Tromberg BJ, Roblyer D (2020) Diffuse optical spectroscopic imaging reveals distinct early breast tumor hemodynamic responses to metronomic and maximum tolerated dose regimens. Breast Cancer Res 22(1):29. https://doi.org/10.1186/s13058-020-01262-1
Zhu Q, Tannenbaum S, Kurtzman SH, DeFusco P, Ricci A Jr, Vavadi H, Zhou F, Xu C, Merkulov A, Hegde P, Kane M, Wang L, Sabbath K (2018) Identifying an early treatment window for predicting breast cancer response to neoadjuvant chemotherapy using immunohistopathology and hemoglobin parameters. Breast Cancer Res 20(1):56. https://doi.org/10.1186/s13058-018-0975-1
Cochran JM et al (2018) Tissue oxygen saturation predicts response to breast cancer neoadjuvant chemotherapy within 10 days of treatment. J Biomed Opt 24:1
Zhu Q, Wang L, Tannenbaum S, Ricci A Jr, DeFusco P, Hegde P (2014) Pathologic response prediction to neoadjuvant chemotherapy utilizing pretreatment near-infrared imaging parameters and tumor pathologic criteria. Breast Cancer Res 16(5):456. https://doi.org/10.1186/s13058-014-0456-0
Zhu Q, DeFusco PA, Ricci A Jr, Cronin EB, Hegde PU, Kane M, Tavakoli B, Xu Y, Hart J, Tannenbaum SH (2013) Breast cancer: assessing response to neoadjuvant chemotherapy by using US-guided near-infrared tomography. Radiology 266(2):433–442. https://doi.org/10.1148/radiol.12112415
Zhi W, Liu G, Chang C, Miao A, Zhu X, Xie L, Zhou J (2018) Predicting treatment response of breast cancer to neoadjuvant chemotherapy using ultrasound-guided diffuse optical tomography. Transl Oncol 11(1):56–64. https://doi.org/10.1016/j.tranon.2017.10.011
Jiang S, Pogue BW, Kaufman PA, Gui J, Jermyn M, Frazee TE, Poplack S, DiFlorio-Alexander R, Wells WA, Paulsen KD (2014) Predicting breast tumor response to neoadjuvant chemotherapy with diffuse optical spectroscopic tomography prior to treatment. Clin Cancer Res 20(23):6006–6015
Jiang S, Pogue BW (2016) A comparison of near-infrared diffuse optical imaging and 18F-FDG PET/CT for the early prediction of breast cancer response to neoadjuvant chemotherapy. J Nucl Med 57:1166
Tran WT, Gangeh MJ, Sannachi L, Chin L, Watkins E, Bruni SG, Rastegar RF, Curpen B, Trudeau M, Gandhi S, Yaffe M, Slodkowska E, Childs C, Sadeghi-Naini A, Czarnota GJ (2017) Predicting breast cancer response to neoadjuvant chemotherapy using pretreatment diffuse optical spectroscopic texture analysis. Br J Cancer 116(10):1329–1339. https://doi.org/10.1038/bjc.2017.97
Vavadi H, Mostafa A, Zhou F, Uddin KMS, Althobaiti M, Xu C, Bansal R, Ademuyiwa F, Poplack S, Zhu Q (2018) Compact ultrasound-guided diffuse optical tomography system for breast cancer imaging. J Biomed Opt 24(2):1–9. https://doi.org/10.1117/1.JBO.24.2.021203
Uddin KMS, Mostafa A, Anastasio M, Zhu Q (2017) Two step imaging reconstruction using truncated pseudoinverse as a preliminary estimate in ultrasound guided diffuse optical tomography. Biomed Opt Express 8(12):5437–5449. https://doi.org/10.1364/BOE.8.005437
Ogston KN, Miller ID, Payne S et al (2003) A new histologic grading system to assess response of breast cancers to primary chemotherapy; prognostic significance and survival. Breast 12:320–327
Symmans WF, Peintinger F, Hatzis C et al (2007) Measurement of residual breast cancer burden to predict survival after neoadjuvant chemotherapy. J Clin Oncol 25:4414–4422
Harvey JM, Clark GM, Osborne CK, Allred DC (1999) Estrogen receptor status by immunohistochemistry is superior to the ligand-binding assay for predicting response to adjuvant endocrine therapy in breast cancer. J Clin Oncol 17(5):1474–1481
Nonparametric Statistics: a step-by-step approach, Gregory W. Corder and Dole I. Foreman (2009).
Heller G, Seshan VE, Moskowitz CS, Gonen M (2016) Inference for the difference in the area under the ROC curve derived from nested binary regression models. Biostatistics 18:260–274
Kruppa J, Liu Y, Biau G, Kohler M, König IR, Malley JD, Ziegler A (2014) Probability estimation with machine learning methods for dichotomous and multicategory outcome: theory. Biom J 56(4):534–563. https://doi.org/10.1002/bimj.201300068
Dobruch-Sobczak K, Piotrzkowska-Wróblewska H, Klimonda Z, Roszkowska-Purska K (2019) Litniewski ultrasound echogenicity reveals the response of breast cancer to chemotherapy. J Clin Imaging 55:41–46. https://doi.org/10.1016/j.clinimag.2019.01.021
Matsuda N, Kida K, Ohde S, Suzuki K, Yamauchi H, Nakamura S, Tsunoda H (2018) Change in sonographic brightness can predict pathological response of triple-negative breast cancer to neoadjuvant chemotherapy. Breast Cancer 25(1):43–49. https://doi.org/10.1007/s12282-017-0782-z
Zhao Y, Dong X, Li R, Ma X, Song J, Li Y, Zhan D (2015) Evaluation of the pathological response and prognosis following neoadjuvant chemotherapy in molecular subtypes of breast cancer. Onco Targets Ther 8:1511–1521
Sejben A, Kószó R, Kahán Z, Cserni G, Zombori T (2020) Examination of tumor regression grading systems in breast cancer patients who received neoadjuvant therapy. Pathol Oncol Res 26(4):2747–2754. https://doi.org/10.1007/s12253-020-00867-3
Masuda N, Lee SJ, Ohtani S, Im YH, Lee ES, Yokota I, Kuroi K, Im SA, Park BW, Kim SB, Yanagita Y, Ohno S, Takao S, Aogi K, Iwata H, Jeong J, Kim A, Park KH, Sasano H, Ohashi Y, Toi M (2017) Adjuvant capecitabine for breast cancer after preoperative chemotherapy. N Engl J Med 376(22):2147–2159. https://doi.org/10.1056/NEJMoa1612645
Acknowledgements
The authors appreciate the help of Clinical Trial Office of the Oncology Department of Washington University School of Medicine for patient consenting and scheduling. Drs. Catherine Young, Catherine Appleton, Matthew F. Covington, were faculty members of Radiology Department of Washington University in St Louis from the beginning of the study to July 2019. Dr. Steven Poplack was a faculty member of Radiology Department of Washington University in St Louis from the beginning of the study to June 2020.
Funding
This study was funded by National Institutes of Health (R01EB002136, R01 CA228047). SPP acknowledges funding support from the Foundation for Barnes Jewish Hospital Ronald and Hanna Evens Endowed Chair in Women’s Health.
Author information
Authors and Affiliations
Contributions
QZ: designed and conducted all aspects of the ultrasound-guided optical tomography data acquisition, image reconstruction and data analysis and contributed to the manuscript preparation and literature review. SPP: designed and conducted patient imaging studies, data analysis, and contributed to the manuscript preparation and literature review. FOA and CM: coordinated and recruited patients to the study, and contributed to the manuscript review and literature review. CY, CA, MFC: contributed to the imaging studies, imaging interpretations, and manuscript review. SS and ISH: contributed to the pathological data evaluations, interpretations, manuscript review. AM and K.M.S.U: contributed to the development of optical tomography system hardware and software as well as imaging algorithm. IG: coordinated, consented all study patients, and data analysis. AEF and LFH: contributed to patient recruitments. All authors read and approved the final manuscript.
Corresponding author
Ethics declarations
Conflict of interest
QZ is the inventor of the patents related to ultrasound-guided near-infrared tomography technologies and patents owned by the University of Connecticut and/or Washington University in St Louis. She has no conflicts of interest. All authors declare that they have no conflicts of interests.
Ethical approval
All procedures performed in studies involving human participants were in accordance with the ethical standards of the institutional and/or national research committee and with the 1964 Helsinki declaration and its later amendments or comparable ethical standards.
Informed consent
Informed consent was obtained from all individual participants included in the study.
Research involving human and animal rights
This article does not contain any studies with animals performed by any of the authors.
Consent for publication
All authors have read the manuscript and agreed with the submission.
Additional information
Publisher's Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Supplementary Information
Below is the link to the electronic supplementary material.
10549_2021_6239_MOESM1_ESM.docx
We developed treatment prediction models using data of 38 patients from this manuscript and data of 22 patients from an earlier study. Results are similar to the regression analysis reported in the manuscript. Please see the supplement materials for details. (DOCX 174 kb)
Rights and permissions
About this article
Cite this article
Zhu, Q., Ademuyiwa, F.O., Young, C. et al. Early Assessment Window for Predicting Breast Cancer Neoadjuvant Therapy using Biomarkers, Ultrasound, and Diffuse Optical Tomography. Breast Cancer Res Treat 188, 615–630 (2021). https://doi.org/10.1007/s10549-021-06239-y
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s10549-021-06239-y