Abstract
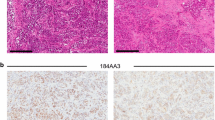
Bypassing estrogen receptor (ER) signaling during development of endocrine resistance remains the most common cause of disease progression and mortality in breast cancer patients. To date, the majority of molecular research on ER action in breast cancer has occurred in cell line models derived from late stage disease. Here we describe patient-derived ER+ luminal breast tumor models for the study of intratumoral hormone and receptor action. Human breast tumor samples obtained from patients post surgery were immediately transplanted into NOD/SCID or NOD/SCID/ILIIrg−/− mice under estrogen supplementation. Five transplantable patient-derived ER+ breast cancer xenografts were established, derived from both primary and metastatic cases. These were assessed for estrogen dependency, steroid receptor expression, cancer stem cell content, and endocrine therapy response. Gene expression patterns were determined in select tumors ±estrogen and ±endocrine therapy. Xenografts morphologically resembled the patient tumors of origin, and expressed similar levels of ER (5–99 %), and progesterone and androgen receptors, over multiple passages. Four of the tumor xenografts were estrogen dependent, and tamoxifen or estrogen withdrawal (EWD) treatment abrogated estrogen-dependent growth and/or tumor morphology. Analysis of the ER transcriptome in select tumors revealed notable differences in ER mechanism of action, and downstream activated signaling networks, in addition to identifying a small set of common estrogen-regulated genes. Treatment of a naïve tumor with tamoxifen or EWD showed similar phenotypic responses, but relatively few similarities in estrogen-dependent transcription, and affected signaling pathways. Several core estrogen centric genes were shared with traditional cell line models. However, novel tumor-specific estrogen-regulated potential target genes, such as cancer/testis antigen 45, were uncovered. These results evoke the importance of mapping both conserved and tumor-unique ER programs in breast cancers. Furthermore, they underscore the importance of primary xenografts for improved understanding of ER+ breast cancer heterogeneity and development of personalized therapies.







Similar content being viewed by others
Abbreviations
- AI:
-
Aromatase inhibitors
- ALDH:
-
Aldehyde dehydrogenase
- AR:
-
Androgen receptor
- AS:
-
Ascites
- CK5:
-
Cytokeratin 5
- CT45:
-
Cancer/testis antigen 45
- ER:
-
Estrogen receptor
- EWD:
-
Estrogen withdrawal
- GEO:
-
Gene expression omnibus
- IHC:
-
Immunohistochemisty
- MPA:
-
Medroxyprogesterone acetate
- PE:
-
Pleural effusion
- PR:
-
Progesterone receptor
- PT:
-
Primary tumor
- qPCR:
-
Quantitative PCR
- TN:
-
Triple negative
References
Obiorah I, Jordan VC (2011) Progress in endocrine approaches to the treatment and prevention of breast cancer. Maturitas 70(4):315–321. doi:10.1016/j.maturitas.2011.09.006
Bardou VJ, Arpino G, Elledge RM, Osborne CK, Clark GM (2003) Progesterone receptor status significantly improves outcome prediction over estrogen receptor status alone for adjuvant endocrine therapy in two large breast cancer databases. J Clin Oncol 21(10):1973–1979. doi:10.1200/JCO.2003.09.099
Axlund SD, Sartorius CA (2012) Progesterone regulation of stem and progenitor cells in normal and malignant breast. Mol Cell Endocrinol 357(1–2):71–79. doi:10.1016/j.mce.2011.09.021
Moinfar F, Okcu M, Tsybrovskyy O, Regitnig P, Lax SF, Weybora W, Ratschek M, Tavassoli FA, Denk H (2003) Androgen receptors frequently are expressed in breast carcinomas: potential relevance to new therapeutic strategies. Cancer 98(4):703–711. doi:10.1002/cncr.11532
Gonzalez LO, Corte MD, Vazquez J, Junquera S, Sanchez R, Alvarez AC, Rodriguez JC, Lamelas ML, Vizoso FJ (2008) Androgen receptor expression in breast cancer: relationship with clinicopathological characteristics of the tumors, prognosis, and expression of metalloproteases and their inhibitors. BMC Cancer 8:149. doi:10.1186/1471-2407-8-149
Peters AA, Buchanan G, Ricciardelli C, Bianco-Miotto T, Centenera MM, Harris JM, Jindal S, Segara D, Jia L, Moore NL, Henshall SM, Birrell SN, Coetzee GA, Sutherland RL, Butler LM, Tilley WD (2009) Androgen receptor inhibits estrogen receptor-alpha activity and is prognostic in breast cancer. Cancer Res 69(15):6131–6140. doi:10.1158/0008-5472.CAN-09-0452
Farmer P, Bonnefoi H, Becette V, Tubiana-Hulin M, Fumoleau P, Larsimont D, Macgrogan G, Bergh J, Cameron D, Goldstein D, Duss S, Nicoulaz AL, Brisken C, Fiche M, Delorenzi M, Iggo R (2005) Identification of molecular apocrine breast tumours by microarray analysis. Oncogene 24(29):4660–4671. doi:10.1038/sj.onc.1208561
Guedj M, Marisa L, de Reynies A, Orsetti B, Schiappa R, Bibeau F, Macgrogan G, Lerebours F, Finetti P, Longy M, Bertheau P, Bertrand F, Bonnet F, Martin AL, Feugeas JP, Bieche I, Lehmann-Che J, Lidereau R, Birnbaum D, Bertucci F, de The H, Theillet C (2011) A refined molecular taxonomy of breast cancer. Oncogene. doi:10.1038/onc.2011.301
Prat A, Perou CM (2011) Deconstructing the molecular portraits of breast cancer. Mol Oncol 5(1):5–23. doi:10.1016/j.molonc.2010.11.003
Osborne CK, Schiff R (2011) Mechanisms of endocrine resistance in breast cancer. Annu Rev Med 62:233–247. doi:10.1146/annurev-med-070909-182917
Abd El-Rehim DM, Pinder SE, Paish CE, Bell J, Blamey RW, Robertson JF, Nicholson RI, Ellis IO (2004) Expression of luminal and basal cytokeratins in human breast carcinoma. J Pathol 203(2):661–671. doi:10.1002/path.1559
Hammond ME, Hayes DF, Dowsett M, Allred DC, Hagerty KL, Badve S, Fitzgibbons PL, Francis G, Goldstein NS, Hayes M, Hicks DG, Lester S, Love R, Mangu PB, McShane L, Miller K, Osborne CK, Paik S, Perlmutter J, Rhodes A, Sasano H, Schwartz JN, Sweep FC, Taube S, Torlakovic EE, Valenstein P, Viale G, Visscher D, Wheeler T, Williams RB, Wittliff JL, Wolff AC (2010) American Society of Clinical Oncology/College of American Pathologists guideline recommendations for immunohistochemical testing of estrogen and progesterone receptors in breast cancer. J Clin Oncol 28(16):2784–2795. doi:10.1200/JCO.2009.25.6529
Creighton CJ, Fu X, Hennessy BT, Casa AJ, Zhang Y, Gonzalez-Angulo AM, Lluch A, Gray JW, Brown PH, Hilsenbeck SG, Osborne CK, Mills GB, Lee AV, Schiff R (2010) Proteomic and transcriptomic profiling reveals a link between the PI3K pathway and lower estrogen-receptor (ER) levels and activity in ER+ breast cancer. Breast Cancer Res 12(3):R40. doi:10.1186/bcr2594
De Amicis F, Thirugnansampanthan J, Cui Y, Selever J, Beyer A, Parra I, Weigel NL, Herynk MH, Tsimelzon A, Lewis MT, Chamness GC, Hilsenbeck SG, Ando S, Fuqua SA (2010) Androgen receptor overexpression induces tamoxifen resistance in human breast cancer cells. Breast Cancer Res Treat 121(1):1–11. doi:10.1007/s10549-009-0436-8
Lange CA, Yee D (2011) Killing the second messenger: targeting loss of cell cycle control in endocrine-resistant breast cancer. Endocr Relat Cancer 18(4):C19–C24. doi:10.1530/ERC-11-0112
O’Brien CS, Howell SJ, Farnie G, Clarke RB (2009) Resistance to endocrine therapy: are breast cancer stem cells the culprits? J Mammary Gland Biol Neoplasia 14(1):45–54. doi:10.1007/s10911-009-9115-y
Honeth G, Bendahl PO, Ringner M, Saal LH, Gruvberger-Saal SK, Lovgren K, Grabau D, Ferno M, Borg A, Hegardt C (2008) The CD44+/CD24− phenotype is enriched in basal-like breast tumors. Breast Cancer Res 10(3):R53. doi:10.1186/bcr2108
Charafe-Jauffret E, Ginestier C, Iovino F, Wicinski J, Cervera N, Finetti P, Hur MH, Diebel ME, Monville F, Dutcher J, Brown M, Viens P, Xerri L, Bertucci F, Stassi G, Dontu G, Birnbaum D, Wicha MS (2009) Breast cancer cell lines contain functional cancer stem cells with metastatic capacity and a distinct molecular signature. Cancer Res 69(4):1302–1313. doi:10.1158/0008-5472.CAN-08-2741
Fillmore CM, Kuperwasser C (2008) Human breast cancer cell lines contain stem-like cells that self-renew, give rise to phenotypically diverse progeny and survive chemotherapy. Breast Cancer Res 10(2):R25. doi:10.1186/bcr1982
Boecker W, Moll R, Poremba C, Holland R, Van Diest PJ, Dervan P, Burger H, Wai D, Ina Diallo R, Brandt B, Herbst H, Schmidt A, Lerch MM, Buchwallow IB (2002) Common adult stem cells in the human breast give rise to glandular and myoepithelial cell lineages: a new cell biological concept. Lab Invest 82(6):737–746. doi:10.1002/path.1241
Lim E, Vaillant F, Wu D, Forrest NC, Pal B, Hart AH, Asselin-Labat ML, Gyorki DE, Ward T, Partanen A, Feleppa F, Huschtscha LI, Thorne HJ, Fox SB, Yan M, French JD, Brown MA, Smyth GK, Visvader JE, Lindeman GJ (2009) Aberrant luminal progenitors as the candidate target population for basal tumor development in BRCA1 mutation carriers. Nat Med 15(8):907–913. doi:10.1038/nm.2000
Kabos P, Haughian JM, Wang X, Dye WW, Finlayson C, Elias A, Horwitz KB, Sartorius CA (2011) Cytokeratin 5 positive cells represent a steroid receptor negative and therapy resistant subpopulation in luminal breast cancers. Breast Cancer Res Treat 128(1):45–55. doi:10.1007/s10549-010-1078-6
Carroll JS, Meyer CA, Song J, Li W, Geistlinger TR, Eeckhoute J, Brodsky AS, Keeton EK, Fertuck KC, Hall GF, Wang Q, Bekiranov S, Sementchenko V, Fox EA, Silver PA, Gingeras TR, Liu XS, Brown M (2006) Genome-wide analysis of estrogen receptor binding sites. Nat Genet 38(11):1289–1297. doi:10.1038/ng1901
Creighton CJ, Cordero KE, Larios JM, Miller RS, Johnson MD, Chinnaiyan AM, Lippman ME, Rae JM (2006) Genes regulated by estrogen in breast tumor cells in vitro are similarly regulated in vivo in tumor xenografts and human breast tumors. Genome Biol 7(4):R28. doi:10.1186/gb-2006-7-4-r28
Frasor J, Danes JM, Komm B, Chang KC, Lyttle CR, Katzenellenbogen BS (2003) Profiling of estrogen up- and down-regulated gene expression in human breast cancer cells: insights into gene networks and pathways underlying estrogenic control of proliferation and cell phenotype. Endocrinology 144(10):4562–4574. doi:10.1210/en.2003-0567
Creighton CJ, Massarweh S, Huang S, Tsimelzon A, Hilsenbeck SG, Osborne CK, Shou J, Malorni L, Schiff R (2008) Development of resistance to targeted therapies transforms the clinically associated molecular profile subtype of breast tumor xenografts. Cancer Res 68(18):7493–7501. doi:10.1158/0008-5472.CAN-08-1404
Massarweh S, Osborne CK, Creighton CJ, Qin L, Tsimelzon A, Huang S, Weiss H, Rimawi M, Schiff R (2008) Tamoxifen resistance in breast tumors is driven by growth factor receptor signaling with repression of classic estrogen receptor genomic function. Cancer Res 68(3):826–833. doi:10.1158/0008-5472.CAN-07-2707
Creighton CJ, Li X, Landis M, Dixon JM, Neumeister VM, Sjolund A, Rimm DL, Wong H, Rodriguez A, Herschkowitz JI, Fan C, Zhang X, He X, Pavlick A, Gutierrez MC, Renshaw L, Larionov AA, Faratian D, Hilsenbeck SG, Perou CM, Lewis MT, Rosen JM, Chang JC (2009) Residual breast cancers after conventional therapy display mesenchymal as well as tumor-initiating features. Proc Natl Acad Sci USA 106(33):13820–13825. doi:10.1073/pnas.0905718106
Harvell DM, Spoelstra NS, Singh M, McManaman JL, Finlayson C, Phang T, Trapp S, Hunter L, Dye WW, Borges VF, Elias A, Horwitz KB, Richer JK (2008) Molecular signatures of neoadjuvant endocrine therapy for breast cancer: characteristics of response or intrinsic resistance. Breast Cancer Res Treat 112(3):475–488. doi:10.1007/s10549-008-9897-4
Ross-Innes CS, Stark R, Teschendorff AE, Holmes KA, Ali HR, Dunning MJ, Brown GD, Gojis O, Ellis IO, Green AR, Ali S, Chin SF, Palmieri C, Caldas C, Carroll JS (2012) Differential oestrogen receptor binding is associated with clinical outcome in breast cancer. Nature 481(7381):389–393. doi:10.1038/nature10730
Bergamaschi A, Hjortland GO, Triulzi T, Sorlie T, Johnsen H, Ree AH, Russnes HG, Tronnes S, Maelandsmo GM, Fodstad O, Borresen-Dale AL, Engebraaten O (2009) Molecular profiling and characterization of luminal-like and basal-like in vivo breast cancer xenograft models. Mol Oncol 3(5–6):469–482. doi:10.1016/j.molonc.2009.07.003
Marangoni E, Vincent-Salomon A, Auger N, Degeorges A, Assayag F, de Cremoux P, de Plater L, Guyader C, De Pinieux G, Judde JG, Rebucci M, Tran-Perennou C, Sastre-Garau X, Sigal-Zafrani B, Delattre O, Dieras V, Poupon MF (2007) A new model of patient tumor-derived breast cancer xenografts for preclinical assays. Clin Cancer Res 13(13):3989–3998. doi:10.1158/1078-0432.CCR-07-0078
DeRose YS, Wang G, Lin YC, Bernard PS, Buys SS, Ebbert MT, Factor R, Matsen C, Milash BA, Nelson E, Neumayer L, Randall RL, Stijleman IJ, Welm BE, Welm AL (2011) Tumor grafts derived from women with breast cancer authentically reflect tumor pathology, growth, metastasis and disease outcomes. Nat Med 17(11):1514–1520. doi:10.1038/nm.2454
Sartorius CA, Shen T, Horwitz KB (2003) Progesterone receptors A and B differentially affect the growth of estrogen-dependent human breast tumor xenografts. Breast Cancer Res Treat 79(3):287–299
Sartorius CA, Harvell DM, Shen T, Horwitz KB (2005) Progestins initiate a luminal to myoepithelial switch in estrogen-dependent human breast tumors without altering growth. Cancer Res 65(21):9779–9788. doi:10.1158/0008-5472.CAN-05-0505
Horwitz KB, Dye WW, Harrell JC, Kabos P, Sartorius CA (2008) Rare steroid receptor-negative basal-like tumorigenic cells in luminal subtype human breast cancer xenografts. Proc Natl Acad Sci USA 105(15):5774–5779. doi:10.1073/pnas.0706216105
Parker JS, Mullins M, Cheang MC, Leung S, Voduc D, Vickery T, Davies S, Fauron C, He X, Hu Z, Quackenbush JF, Stijleman IJ, Palazzo J, Marron JS, Nobel AB, Mardis E, Nielsen TO, Ellis MJ, Perou CM, Bernard PS (2009) Supervised risk predictor of breast cancer based on intrinsic subtypes. J Clin Oncol 27(8):1160–1167. doi:10.1200/JCO.2008.18.1370
Harrell JC, Prat A, Parker JS, Fan C, He X, Carey L, Anders C, Ewend M, Perou CM (2012) Genomic analysis identifies unique signatures predictive of brain, lung, and liver relapse. Breast Cancer Res Treat 132(2):523–535. doi:10.1007/s10549-011-1619-7
Pink JJ, Jordan VC (1996) Models of estrogen receptor regulation by estrogens and antiestrogens in breast cancer cell lines. Cancer Res 56(10):2321–2330
Frasor J, Stossi F, Danes JM, Komm B, Lyttle CR, Katzenellenbogen BS (2004) Selective estrogen receptor modulators: discrimination of agonistic versus antagonistic activities by gene expression profiling in breast cancer cells. Cancer Res 64(4):1522–1533
Santen RJ (1996) Long-term tamoxifen therapy: can an antagonist become an agonist? J Clin Endocrinol Metab 81(6):2027–2029
Ghosh MG, Thompson DA, Weigel RJ (2000) PDZK1 and GREB1 are estrogen-regulated genes expressed in hormone-responsive breast cancer. Cancer Res 60(22):6367–6375
Rae JM, Johnson MD, Scheys JO, Cordero KE, Larios JM, Lippman ME (2005) GREB 1 is a critical regulator of hormone dependent breast cancer growth. Breast Cancer Res Treat 92(2):141–149. doi:10.1007/s10549-005-1483-4
Fagan DH, Yee D (2008) Crosstalk between IGF1R and estrogen receptor signaling in breast cancer. J Mammary Gland Biol Neoplasia 13(4):423–429. doi:10.1007/s10911-008-9098-0
Chen YT, Ross DS, Chiu R, Zhou XK, Chen YY, Lee P, Hoda SA, Simpson AJ, Old LJ, Caballero O, Neville AM (2011) Multiple cancer/testis antigens are preferentially expressed in hormone-receptor negative and high-grade breast cancers. PLoS One 6(3):e17876. doi:10.1371/journal.pone.0017876
Simpson AJ, Caballero OL, Jungbluth A, Chen YT, Old LJ (2005) Cancer/testis antigens, gametogenesis and cancer. Nat Rev Cancer 5(8):615–625. doi:10.1038/nrc1669
Muss HB, Cruz JM (1992) High-dose progestin therapy for metastatic breast cancer. Ann Oncol 3(Suppl 3):15–20
Mahlke M, Grill HJ, Knapstein P, Wiegand U, Pollow K (1985) Oral high-dose medroxyprogesterone acetate (MPA) treatment: cortisol/MPA serum profiles in relation to breast cancer regression. Oncology 42(3):144–149
Tyson JJ, Baumann WT, Chen C, Verdugo A, Tavassoly I, Wang Y, Weiner LM, Clarke R (2011) Dynamic modelling of oestrogen signalling and cell fate in breast cancer cells. Nat Rev Cancer 11(7):523–532. doi:10.1038/nrc3081
Krop I, Winer EP (2012) Further progress in HER2-directed therapy. Lancet Oncol 13(1):2–3. doi:10.1016/S1470-2045(11)70388-6
Osborne CK, Neven P, Dirix LY, Mackey JR, Robert J, Underhill C, Schiff R, Gutierrez C, Migliaccio I, Anagnostou VK, Rimm DL, Magill P, Sellers M (2011) Gefitinib or placebo in combination with tamoxifen in patients with hormone receptor-positive metastatic breast cancer: a randomized phase II study. Clin Cancer Res 17(5):1147–1159. doi:10.1158/1078-0432.CCR-10-1869
Baselga J, Campone M, Piccart M, Burris HA III, Rugo HS, Sahmoud T, Noguchi S, Gnant M, Pritchard KI, Lebrun F, Beck JT, Ito Y, Yardley D, Deleu I, Perez A, Bachelot T, Vittori L, Xu Z, Mukhopadhyay P, Lebwohl D, Hortobagyi GN (2012) Everolimus in postmenopausal hormone-receptor-positive advanced breast cancer. N Engl J Med 366(6):520–529. doi:10.1056/NEJMoa1109653
Wolfer A, Wittner BS, Irimia D, Flavin RJ, Lupien M, Gunawardane RN, Meyer CA, Lightcap ES, Tamayo P, Mesirov JP, Liu XS, Shioda T, Toner M, Loda M, Brown M, Brugge JS, Ramaswamy S (2010) MYC regulation of a “poor-prognosis” metastatic cancer cell state. Proc Natl Acad Sci USA 107(8):3698–3703. doi:10.1073/pnas.0914203107
Tzivion G, Gupta VS, Kaplun L, Balan V (2006) 14–3-3 proteins as potential oncogenes. Semin Cancer Biol 16(3):203–213. doi:10.1016/j.semcancer.2006.03.004
Asselin-Labat ML, Shackleton M, Stingl J, Vaillant F, Forrest NC, Eaves CJ, Visvader JE, Lindeman GJ (2006) Steroid hormone receptor status of mouse mammary stem cells. J Natl Cancer Inst 98(14):1011–1014. doi:10.1093/jnci/djj267
Sleeman KE, Kendrick H, Robertson D, Isacke CM, Ashworth A, Smalley MJ (2007) Dissociation of estrogen receptor expression and in vivo stem cell activity in the mammary gland. J Cell Biol 176(1):19–26
Haughian JM, Pinto MP, Harrell JC, Bliesner BS, Joensuu KM, Dye WW, Sartorius CA, Tan AC, Heikkila P, Perou CM, Horwitz KB (2012) Maintenance of hormone responsiveness in luminal breast cancers by suppression of Notch. Proc Natl Acad Sci USA 109(8):2742–2747. doi:10.1073/pnas.1106509108
Fillmore CM, Gupta PB, Rudnick JA, Caballero S, Keller PJ, Lander ES, Kuperwasser C (2010) Estrogen expands breast cancer stem-like cells through paracrine FGF/Tbx3 signaling. Proc Natl Acad Sci USA 107(50):21737–21742. doi:10.1073/pnas.1007863107
Magee JA, Piskounova E, Morrison SJ (2012) Cancer stem cells: impact, heterogeneity, and uncertainty. Cancer Cell 21(3):283–296. doi:10.1016/j.ccr.2012.03.003
Farmer P, Bonnefoi H, Becette V, Tubiana-Hulin M, Fumoleau P, Larsimont D, MacGrogan G, Bergh J, Cameron D, Goldstein D, Duss S, Delorenzi M, Iggo R (2005) Identification of molecular apocrine breast tumours by microarray analysis. Cancer Treat Rev 31:S15
Chlebowski RT, Anderson GL, Gass M, Lane DS, Aragaki AK, Kuller LH, Manson JE, Stefanick ML, Ockene J, Sarto GE, Johnson KC, Wactawski-Wende J, Ravdin PM, Schenken R, Hendrix SL, Rajkovic A, Rohan TE, Yasmeen S, Prentice RL (2010) Estrogen plus progestin and breast cancer incidence and mortality in postmenopausal women. JAMA 304(15):1684–1692. doi:10.1001/jama.2010.1500
Jacobsen BM, Richer JK, Sartorius CA, Horwitz KB (2003) Expression profiling of human breast cancers and gene regulation by progesterone receptors. J Mammary Gland Biol Neoplasia 8(3):257–268
Graham JD, Mote PA, Salagame U, van Dijk JH, Balleine RL, Huschtscha LI, Reddel RR, Clarke CL (2009) DNA replication licensing and progenitor numbers are increased by progesterone in normal human breast. Endocrinology 150(7):3318–3326. doi:10.1210/en.2008-1630
Clarke CL, Graham JD (2012) Non-overlapping progesterone receptor cistromes contribute to cell-specific transcriptional outcomes. PLoS One 7(4):e35859. doi:10.1371/journal.pone.0035859
Acknowledgments
The authors thank Robert Tsay for providing tissue from pathological specimens, Lisa Litzenberger for graphics help, Audrie Van Bokhoven for the AR control slides, Britta Jacobsen and Elizabeth Wellberg for critical review of the manuscript, and the University of Colorado Cancer Center Breast Cancer Tissue Bank, Tissue Procurement, and Flow Cytometry Cores for their excellent services. This work was supported, in part, by grants from the Grohne Cancer Research Fund (P. Kabos), ASCO Young Investigator Award (P. Kabos), the National Institutes of Health R01 CA140985 (C. Sartorius), the Wendy Will Case Foundation (C. Sartorius), the University of Colorado Cancer Center (P. Kabos and C. Sartorius), and the Martha Cannon Dear Professorship (A. Elias).
Conflict of interest
The authors have no conflicts of interest to disclose.
Author information
Authors and Affiliations
Corresponding author
Electronic supplementary material
Below is the link to the electronic supplementary material.
Rights and permissions
About this article
Cite this article
Kabos, P., Finlay-Schultz, J., Li, C. et al. Patient-derived luminal breast cancer xenografts retain hormone receptor heterogeneity and help define unique estrogen-dependent gene signatures. Breast Cancer Res Treat 135, 415–432 (2012). https://doi.org/10.1007/s10549-012-2164-8
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s10549-012-2164-8