Abstract
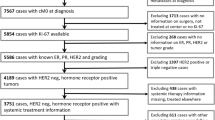
The aim of this analysis was to investigate the usefulness of Ki-67 labeling index (LI) for the identification of different prognostic subgroups in primary node-negative, triple negative breast cancer (TNBC) patients. From January 1997 to December 2005, 1,053 patients operated for TNBC were identified through the institutional clinical database. The study was performed in accordance with REMARK criteria. The relationship between Ki-67LI and the risk of breast-related deaths was evaluated with a multivariable Cox regression model. Cubic splines were used to model Ki-67LI as a continuous variable. We selected 496 consecutive patients with node-negative TNBC. Median age was 52 years, median Ki-67LI 48 % (range 4–95), and median follow up 6 years (range 0.5–13). Total deaths and deaths from BC were 52 (10.5 %) and 38 (7.7 %), respectively. Ki-67LI increased with decreasing age (P < 0.01), increasing tumor size (P < 0.01), and grade (P < 0.01). When analyzing Ki-67LI as a continuous variable, the risk of death from BC increased steeply with increasing Ki-67LI up to about 35 % and remained flat for higher values (adjusted effect of Ki-67 P = 0.049; adjusted nonlinear effect P = 0.021). Accordingly, when dividing patients into lower (≤35 %) and higher (>35 %) Ki-67LI subgroups, the 5-year cumulative incidence of breast-related deaths were 2.3 and 9.0 %, respectively, with an adjusted HR>35 vs ≤35 of 2.3 (95 % CI 1.0–5.8, P = 0.046). Within the group of patients with node-negative TNBC, Ki-67LI was associated with different prognoses subgroups. Ki-67LI might be useful in the design of trials of risk-adapted adjuvant therapies.


Similar content being viewed by others
References
Gluz O, Liedtke C, Gottschalk N et al (2009) Triple negative breast cancer—current status and future directions. Ann Oncol 20:1913–1927
Hudis C, Gianni L (2011) Triple-negative breast cancer: an unmet medical need. Oncologist 16(suppl 1):1–11
Adamo B, Anders CK (2011) Stratifying triple-negative breast cancer: which definition(s) to use? Breast Cancer Res 13:105
Cheang MC, Voduc D, Bajdik C et al (2008) Basal-like breast cancer defined by five biomarkers has superior prognostic value than triple-negative phenotype. Clin Cancer Res 14:1368–1376
Prat A, Parker J, Karginova O et al (2010) Phenotypic and molecular characterization of the claudin-low intrinsic subtype of breast cancer. Breast Cancer Res 12:R68
Urruticoechea A, Smith IE, Dowsett M (2005) Proliferation marker Ki-67 in early breast cancer. J Clin Oncol 23(28):7212–7220
Petit T, Wilt M, Velten M et al (2004) Comparative value of tumour grade, hormonal receptors, Ki-67, HER-2 and topoisomerase II alpha status as predictive markers in breast cancer patients treated with neoadjuvant anthracycline-based chemotherapy. Eur J Cancer 40:205–211
Pohl G, Rudas M, Taucher S et al (2003) Expression of cell cycle regulatory proteins in breast carcinomas before and after preoperative chemotherapy. Breast Cancer Res Treat 78:97–103
Brown RW, Allred CD, Clark GM et al (1996) Prognostic value of Ki-67 compared to S-phase fraction in axillary node-negative breast cancer. Clin Cancer Res 2:585–592
Weikel W, Brumm C, Wilkens C, Beck T, Knapstein PG (1995) Growth fractions (Ki-67) in primary breast cancers, with particular reference to node-negative tumors. Cancer Detect Prev 19:446–450
Rhee J, Han SW, Oh DY et al (2008) The clinicopathologic characteristics and prognostic significance of triple-negativity in node-negative breast cancer. BMC Cancer 8:307
Dowsett M, Nielsen TO, A’hern R et al (2011) Assessment of Ki67 in breast cancer: recommendations from the International Ki67 in Breast Cancer Working Group. J Natl Cancer Inst 103:1656–1664
Hernandez-Aya LF, Chavez-MacGregor M, Lei X et al (2011) Nodal status and clinical outcomes in a large cohort of patients with triple-negative breast cancer. J Clin Oncol 29:2628–2634
McShane LM, Altman DG, Sauerbrei W et al (2006) Reporting recommendations for tumor MARKer prognostic studies (REMARK). Breast Cancer Res Treat 100:229–235
Rosen PP, Oberman H (1993) Tumors of the mammary gland. Armed Forces Institute of Pathology, Washington, DC
Elston CW, Ellis IO (2002) Pathological prognostic factors in breast cancer, I: the value of histological grade in breast cancer: experience from a large study with long-term follow-up. Histopathology 41:151
Gray RJ (1988) A class of K-sample tests for comparing the cumulative incidence of a competing risk. Ann Stat 16:1141–1154
Durrleman S, Simon R (1989) Flexible regression models with cubic splines. Stat Med 8:551–561
Dent R, Trudeau M, Pritchard KI et al (2007) Triple-negative breast cancer: clinical features and patterns of recurrence. Clin Cancer Res 13:4429–4434
Keam B, Im SA, Lee KH et al (2011) Ki-67 can be used for further classification of triple negative breast cancer into two subtypes with different response and prognosis. Breast Cancer Res 13:R22
Rakha EA, El-Rehim DA, Paish C et al (2006) Basal phenotype identifies a poor prognostic subgroup of breast cancer of clinical importance. Eur J Cancer 42:3149–3156
Yamamoto Y, Ibusuki M, Nakano M et al (2009) Clinical significance of basal-like subtype in triple-negative breast cancer. Breast Cancer 16:260–267
Munzone E, Curigliano G, Burstein HJ et al (2012) CMF revisited in the 21st century. Ann Oncol 23(2):305–311
Paik S (2011) Is gene array testing to be considered routine now? Breast 20:S87–S91
Wirapati P, Sotiriou C, Kunkel S et al (2008) Meta-analysis of gene expression profiles in breast cancer: toward a unified understanding of breast cancer subtyping and prognosis signatures. Breast Cancer Res 10(4):R65
Conflict of interest
The authors declare that they have no conflict of interest.
Author information
Authors and Affiliations
Corresponding author
Rights and permissions
About this article
Cite this article
Munzone, E., Botteri, E., Sciandivasci, A. et al. Prognostic value of Ki-67 labeling index in patients with node-negative, triple-negative breast cancer. Breast Cancer Res Treat 134, 277–282 (2012). https://doi.org/10.1007/s10549-012-2040-6
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s10549-012-2040-6