Abstract
Background:The risk and outcome of regional failure after elective and therapeutic lymph node dissection (ELND/TLND) for microscopically and macroscopically involved lymph nodes without adjuvant radiotherapy were evaluated.
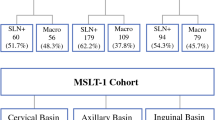
Methods:Retrospective melanoma database review of 338 patients (ELND 85, TLND 253) from 1970 to 1996 with pathologically involved lymph nodes.
Results:Regional recurrence occurred in 14% of patients treated with ELND (n = 12) and 28% of patients treated with TLND (n = 72; P = .009). Risk factors associated with nodal recurrence were advanced age, primary lesion in the head and neck region, depth of the primary lesion, number of involved lymph nodes, and extracapsular extension (ECE). For each nodal basin, the ELND group had a lower incidence of recurrence than the TLND group. The TLND group had larger lymph nodes, greater number of involved lymph nodes, and a higher incidence of ECE. The 10-year disease-specific survival was 51% vs. 30% for ELND and TLND, respectively (P = .0005). Nodal basin failure was predictive of distant metastasis, with 87% developing distant disease compared with 54% of patients without nodal recurrence (P < .0001). Of six patients who underwent a second dissection after isolated nodal recurrence, five patients have had a median disease-free interval of 79 months.
Conclusions:After ELND or TLND, patients who have a large tumor burden (thick primary melanoma, multiply involved lymph nodes, ECE), advanced age, and a primary lesion located in the head and neck have a significantly increased likelihood of relapse and a decreased survival. Few patients present with an isolated nodal recurrence, but the majority can be salvaged by a second dissection.
Similar content being viewed by others
REFERENCES
Fusi S, Ariyan S, Sternlicht A. Data on first recurrence after treatment for malignant melanoma in a large patient population Plast Reconstr Surg 1993; 91: 94–8.
Reintgen DS, Cox C, Slingluff CL, Seigler HF. Recurrent melanoma: The identification of prognostic factors to predict survival. Ann Plast Surg 1992; 28: 45–9.
McCarthy WH, Shaw HM, Thompson JF, Milton GW. Time and frequency of recurrence of cutaneous stage I malignant melanoma with guidelines for follow up study. Surg Gynecol Obstet 1988; 166: 497–502.
Milton GW, Shaw HM, Farago GA, McCarthy WH. Tumor thickness and the site and time of first recurrence in cutaneous malignant melanoma (stage I). Br J Surg 1980; 67: 543–6.
Balch CM, Soong SJ, Bartolucci AA, et al. Efficacy of an elective regional lymph node dissection of 1 to 4 mm thick melanomas for patients 60 years of age and younger. Ann Surg 1996; 224: 25–66.
Balch CM, Soong SJ, Ross MI, et al. Long term results of a multi-institutional randomized trial comparing prognostic factor and surgical results for intermediate thickness melanomas (1.0 to 4.0 mm). Ann Surg Oncol 2000; 7: 87–97.
Emilia J, Lawrence W. Sentinel lymph node biopsy in malignant melanoma: The standard of care? J Surg Oncol 1997; 65: 153–4.
Miller EJ, Daly JM, Synnestvedt M, Schultz D, Elder D, Guerry D. Loco-regional nodal relapse in melanoma. Surg Oncol 1992; 1: 333–40.
Warso MA, DasGupta TK. Melanoma recurrence in a previously dissected lymph node basin. Arch Surg 1994; 129: 252–5.
Calabro A, Singletary SE, Balch CM. Patterns of relapse in 1001 consecutive patients with melanoma nodal metastases. Arch Surg 1989; 124: 1051–5.
Monsour PD, Sause WT, Avent JM, Noyes RD. Local control following therapeutic nodal dissection for melanoma. J Surg Oncol 1993; 54: 18–22.
Ang KK, Peters LJ, Weber RS, et al. Post operative radiotherapy for cutaneous melanoma of the head and neck region. Int J Radiat Oncol Biol Phys 1994; 30: 795–8.
Karakousis CP, Driscoll DL, Rose B, Walsh DL. Groin dissection in malignant melanoma. Ann Surg Oncol 1994; 1: 271–7.
Karakousis CP. Therapeutic node dissections in malignant melanoma. Ann Surg Oncol 1998; 5: 473–82.
Cox D. Regression models and life tables. J Royal Stat Soc B 1972; 34: 187–220.
Kaplan EL, Meier P. Nonparametric estimation from incomplete observations. J Am Stat Assoc 1958; 53: 457–81.
Show JHF, Rumball EM. Complications and local recurrence following lymphadenectomy. Br J Surg 1990; 77: 760–4.
Gadd MA, Coit DG. Recurrence patterns and outcome in 1019 patients undergoing axillary or inguinal lymphadenectomy for melanoma. Arch Surg 1992; 127: 1412–6.
O’Brien CJ, Gianoutsos MP, Morgan MJ. Neck dissection for cutaneous malignant melanoma. World J Surg 1992; 16: 222–6.
Belli F, Nave M, Santinami M, Rovini D, Valgani M. Management of nodal metastases from head and neck melanoma. J Surg Oncol 1989; 42: 47–53.
Baas PC, Koops HS, Hoekstra HJ, van Bruggen JJ, van derWheele LT, Oldhoff J. Groin dissection in the treatment of lower-extremity melanoma. Arch Surg 1992; 127: 281–6.
Van deVrie W, Eggermont AMM, Was Putten WLJ, Wiggers T. Therapeutic lymphadenectomy in melanomas of the head and neck. Head Neck 1993; 15: 377–81.
Mann GB, Coit DC. Does the extent of operation influence the prognosis in patients with melanoma metastatic to inguinal nodes? Ann Surg Oncol 1999; 6: 263–71.
Strom EA, Ross MI. Adjuvant radiation therapy after axillary lymphadenectomy for metastatic melanoma: Toxicity and local control. Ann Surg Oncol 1995; 2: 445–9.
O’Brian CJ, Petersen-Schaefer K, Ruark D, Coates AS, Menzie SJ, Harrison RI. Radical, modified and selective neck dissection for cutaneous malignant melanoma. Head Neck 1995; 17: 232–41.
Johanson CR, Harwood AR, Cummings BJ, Ouirt I. 0-7-21 radiotherapy in nodular melanoma. Cancer 1983; 51: 226–32.
Houghton A, Coit D, Bloomer W, et al. NCCN melanoma practice guidelines. National Comprehensive Cancer Network. Oncology 1998; 12: 153–177.
Essner R, Conforti AC, Kelley MC, Wanek L, Stern A, Glass E, Morton DL. Efficacy of lymphatic mapping, sentinel lymphadenectomy, and selective complete lymph node dissection as a therapeutic procedure for early-stage melanoma. Ann Surg Oncol 1999; 6: 442–9.
Author information
Authors and Affiliations
Corresponding author
Rights and permissions
About this article
Cite this article
Pidhorecky, I., Lee, R.J., Proulx, G. et al. Risk Factors for Nodal Recurrence After Lymphadenectomy for Melanoma. Ann Surg Oncol 8, 109–115 (2001). https://doi.org/10.1007/s10434-001-0109-2
Received:
Accepted:
Issue Date:
DOI: https://doi.org/10.1007/s10434-001-0109-2