Abstract
Background
Recommended treatment for patients with sentinel lymph node (SLN)-positive melanoma has recently changed. Randomized trials demonstrated equivalent survival with close observation versus completion lymph node dissection (CLND), but increased regional node recurrence. We evaluated factors related to in-basin nodal recurrence after lymphadenectomy (LND) for SLN-positive or macroscopic nodal metastases.
Methods
An institutional database and the first Multicenter Selective Lymphadenectomy Trial (MSLT-I) were analyzed independently. Exclusions were multiple primaries, multi-basin involvement, or in-transit metastases. Patient demographics, primary tumor thickness and ulceration, lymph nodes retrieved, and use of adjuvant radiotherapy were analyzed. Multivariate analyses were performed to determine factors predicting in-basin nodal recurrence (significance p ≤ 0.05).
Results
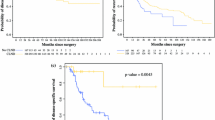
The retrospective cohort (577 patients) showed an in-basin failure rate of 6.6% after CLND for a positive SLN and 13.1% after LND for palpable disease (p = 0.001). This recurrence risk persisted after adjustment for patient, tumor, and LND factors [hazard ratio (HR) 2.32; p = 0.004]. In the MSLT-I cohort (326 patients), the failure rate after CLND following SLNB was 6.2%, but 10.1% after LND for palpable recurrence in observation patients. After adjustment for other factors, macroscopic disease was associated with an increased risk of recurrence after LND (HR 2.24; p = 0.05).
Conclusion
After LND for melanoma, in-basin recurrence is infrequent, but a clinically significant fraction will fail. Failure is less likely if dissection is performed for clinically occult disease. Further research is warranted to evaluate the long-term regional control and quality of life associated with nodal basin observation, which has now become standard practice.


Similar content being viewed by others
References
Morton DL, Thompson JF, Cochran AJ, et al. Final trial report of sentinel-node biopsy versus nodal observation in melanoma. N Engl J Med. 2014;370:599–609.
Faries MB, Thompson JF, Cochran AJ, et al. Completion dissection or observation for sentinel-node metastasis in melanoma. N Engl J Med. 2017;376:2211–22.
Pidhorecky I, Lee RJ, Proulx G, et al. Risk factors for nodal recurrence after lymphadenectomy for melanoma. Ann Surg Oncol. 2001;8:109–15.
Calabro A, Singletary E, Balch CM. Patterns of relapse in 1001 consecutive patients with melanoma nodal metastases. Arch Surg. 1989;124:1051–5.
Nathansohn N, Schachter J, Gutman H. Patterns of recurrence in patients with melanoma after radical lymph node dissection. Arch Surg. 2005;140(12):1172–7.
White RR, Stanley WE, Johnson JL, Tyler DS, Seigler HF. Long-term survival in 2,505 patients with melanoma with regional lymph node metastasis. Ann Surg. 2002;235:879–87.
Fisher SR. Cutaneous malignant melanoma of the head and neck. Laryngoscope. 1989;99:822–36.
Eggermont AMM, Blank CU, Mandala M, et al. Adjuvant pembrolizumab versus placebo in resected stage III melanoma. N Engl J Med. 2018;378:1789–801.
Hauschild A, Dummer R, Schadendorf D, et al. Longer follow-up confirms relapse-free survival benefit with adjuvant dabrafenib plus trametinib in patients with resected BRAF V600–mutant stage III melanoma. J Clin Oncol. 2018;36:3441–9.
Funding
This study was funded by the National Institutes of Health (R01CA189163).
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
Disclosures
Mark B. Faries has served on advisory boards for Array Bioscience, Bristol-Myers Squibb, Novartis, Castle Bioscience and Pulse Bioscience, and is a consultant for Delcath Systems. Vernon K. Sondak has served on advisory boards for Merck, Bristol-Meyers Squibb, Novartis and Regeneron, as well as data safety monitor boards for Bristol-Meyers Squibb, Array Bioscience, Novartis, Polynoma and Pfizer. Alistair J. Cochran has received National Institutes of Health grant funding related to this manuscript. Abhineet Uppal, Stacey Stern, John F. Thompson, Leland Foshag, Nicola Mizzollo, Omgo E. Nieweg, Harald J. Hoekstra, Daniel F. Roses, Mohammed Kashani-Sabet, Brendon J. Coventry, Manabu Fujita, Myung Sim-Shin, David Elashoff, and Robert M. Elashoff have no conflicts of interest to declare.
Additional information
Publisher's Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Rights and permissions
About this article
Cite this article
Uppal, A., Stern, S., Thompson, J.F. et al. Regional Node Basin Recurrence in Melanoma Patients: More Common After Node Dissection for Macroscopic Rather than Clinically Occult Nodal Disease. Ann Surg Oncol 27, 1970–1977 (2020). https://doi.org/10.1245/s10434-019-08086-0
Received:
Published:
Issue Date:
DOI: https://doi.org/10.1245/s10434-019-08086-0