Abstract
High-intensity focused ultrasound (HIFU) was experimentally used for focal therapy for anti-cancer effects in prostate cancer (PC). Focal therapy is a diagnosis-based investigational treatment option for localized PC that cures clinically significant PC (csPC) while preserving the anatomical structures related to urinary and sexual function based on its spread observed using multi-parametric magnetic resonance imaging (mpMRI). The European Association of Urology indicated that the current status of focal therapy for localized PC was an investigational modality and encouraged prospective recording of outcomes and recruitment of suitable patients in 2018. During the last few years, large-population multi- and single-center prospective studies have investigated focal therapy as a treatment strategy for localized PC. In a multicenter prospective study with 5-year follow-up, failure-free survival, which was defined as avoidance of local salvage therapy (surgery or radiotherapy), systemic therapy, metastases, and prostate cancer-specific death, was 88%. In the previous studies, there was no significant influence on urinary function before and at 3 months after the treatment, although transient impairment was reported 1 month after the treatment. Pad- and leak-free continence was preserved in 80–100% of the patients after treatment. Erectile function was significantly impaired in the initial 3 months after treatment compared to the pretreatment values, but it improved 6 months after the focal therapy in the previous reports. Paired comparison studies and cohort studies with long-term follow-up will contribute to verifying this treatment's clinical outcomes for patients with localized PC.



Similar content being viewed by others
References
Barret E, Turkbey B, Puech P, et al. Update on the ICUD-SIU consultation on multi-parametric magnetic resonance imaging in localised prostate cancer. World J Urol. 2019;37:429–36.
Onik G, Miessau M, Bostwick DG. Three-dimensional prostate mapping biopsy has a potentially significant impact on prostate cancer management. J Clin Oncol. 2009;27:4321–6.
Stamey TA, Freiha FS, McNeal JE, Redwine EA, Whittemore AS, Schmid HP. Localized prostate cancer. Relationship of tumor volume to clinical significance for treatment of prostate cancer. Cancer. 1993;71:933–8.
Shoji S, Hiraiwa S, Hanada I, et al. Current status and future prospective of focal therapy for localized prostate cancer: development of multiparametric MRI, MRI-TRUS fusion image-guided biopsy, and treatment modalities. Int J Clin Oncol. 2020;25:509–20.
Shoji S, Ukimura O, de Castro Abreu AL, et al. Image-based monitoring of targeted biopsy-proven prostate cancer on active surveillance: 11-year experience. World J Urol. 2016;34:221–7.
Schoots IG, Roobol MJ, Nieboer D, Bangma CH, Steyerberg EW, Hunink MG. Magnetic resonance imaging-targeted biopsy may enhance the diagnostic accuracy of significant prostate cancer detection compared to standard transrectal ultrasound-guided biopsy: a systematic review and meta-analysis. Eur Urol. 2015;68:438–50.
Rud E, Klotz D, Rennesund K, et al. Detection of the index tumour and tumour volume in prostate cancer using T2-weighted and diffusion-weighted magnetic resonance imaging (MRI) alone. BJU Int. 2014;114:E32–42.
Baco E, Ukimura O, Rud E, et al. Magnetic resonance imaging-transectal ultrasound image-fusion biopsies accurately characterize the index tumor: correlation with step-sectioned radical prostatectomy specimens in 135 patients. Eur Urol. 2015;67:787–94.
Rajwa P, Pradere B, Quhal F, et al. Reliability of serial prostate magnetic resonance imaging to detect prostate cancer progression during active surveillance: a systematic review and meta-analysis. Eur Urol. 2021 (in press).
Hettiarachchi D, Geraghty R, Rice P, et al. Can the use of serial multiparametric magnetic resonance imaging during active surveillance of prostate cancer avoid the need for prostate biopsies? A systematic diagnostic test accuracy review. Eur Urol Oncol. 2021;4:426–36.
Hung AJ, Abreu AL, Shoji S, et al. Robotic transrectal ultrasonography during robot-assisted radical prostatectomy. Eur Urol. 2012;62:341–8.
Shoji S, Aron M, de Castro Abreu AL, et al. Intraoperative ultrasonography with a surgeon-manipulated microtransducer during robotic radical prostatectomy. Int J Urol. 2014;21:736–9.
Onik G, Narayan P, Vaughan D, Dineen M, Brunelle R. Focal, “nerve-sparing” cryosurgery for treatment of primary prostate cancer: a new approach to preserving potency. Urology. 2002;60:109–14.
Crouzet S, Chapelon JY, Rouviere O, et al. Whole-gland ablation of localized prostate cancer with high-intensity focused ultrasound: oncologic outcomes and morbidity in 1002 patients. Eur Urol. 2014;65:907–14.
Uchida T, Tomonaga T, Kim H, et al. Improved outcomes with advancements in high intensity focused ultrasound devices for the treatment of localized prostate cancer. J Urol. 2015;193:103–10.
Madersbacher S, Pedevilla M, Vingers L, Susani M, Marberger M. Effect of high-intensity focused ultrasound on human prostate cancer in vivo. Cancer Res. 1995;55:3346–51.
Shoji S, Nakano M, Nagata Y, Usui Y, Terachi T, Uchida T. Quality of life following high-intensity focused ultrasound for the treatment of localized prostate cancer: a prospective study. Int J Urol. 2010;17:715–9.
Shoji S, Uchida T, Hanada I, et al. Analysis of oncological outcomes of whole-gland therapy with high-intensity focused ultrasound for localized prostate cancer in clinical and technical aspects: a retrospective consecutive case-series analysis with a median 5-year follow-up. Int J Hyperthermia. 2021;38:1205–16.
Chapelon JY, Margonari J, Vernier F, Gorry F, Ecochard R, Gelet A. In vivo effects of high-intensity ultrasound on prostatic adenocarcinoma Dunning R3327. Cancer Res. 1992;52:6353–7.
Oosterhof GO, Cornel EB, Smits GA, Debruyne FM, Schalken JA. Influence of high-intensity focused ultrasound on the development of metastases. Eur Urol. 1997;32:91–5.
Gelet A, Chapelon JY, Margonari J, et al. Prostatic tissue destruction by high-intensity focused ultrasound: experimentation on canine prostate. J Endourol. 1993;7:249–53.
Foster RS, Bihrle R, Sanghvi N, et al. Production of prostatic lesions in canines using transrectally administered high-intensity focused ultrasound. Eur Urol. 1993;23:330–6.
Kincaide LF, Sanghvi NT, Cummings O, et al. Noninvasive ultrasonic subtotal ablation of the prostate in dogs. Am J Vet Res. 1996;57:1225–7.
Beerlage HP, van Leenders GJ, Oosterhof GO, et al. High-intensity focused ultrasound (HIFU) followed after one to two weeks by radical retropubic prostatectomy: results of a prospective study. Prostate. 1999;39:41–6.
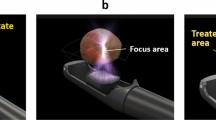
Shoji S, Mouraviev V, Scionti S. High intensity focused ultrasound (HIFU) treatment of prostate cancer. Handbook of Focal Therapy for Prostate and Renal Cancer; 2016. p. 241–54.
Silverman RH, Muratore R, Ketterling JA, Mamou J, Coleman DJ, Feleppa EJ. Improved visualization of high-intensity focused ultrasound lesions. Ultrasound Med Biol. 2006;32:1743–51.
Shoji S, Hiraiwa S, Uemura K, et al. Focal therapy with high-intensity focused ultrasound for the localized prostate cancer for Asian based on the localization with MRI-TRUS fusion image-guided transperineal biopsy and 12-cores transperineal systematic biopsy: prospective analysis of oncological and functional outcomes. Int J Clin Oncol. 2020;25:1844–53.
Shoji S, Uchida T, Nakamoto M, et al. Prostate swelling and shift during high intensity focused ultrasound: implication for targeted focal therapy. J Urol. 2013;190:1224–32.
Shoji S, Tonooka A, Hashimoto A, et al. Time-dependent change of blood flow in the prostate treated with high-intensity focused ultrasound. Int J Urol. 2014;21:942–5.
Ahmed HU, Hindley RG, Dickinson L, et al. Focal therapy for localised unifocal and multifocal prostate cancer: a prospective development study. Lancet Oncol. 2012;13:622–32.
Ahmed HU, Freeman A, Kirkham A, et al. Focal therapy for localized prostate cancer: a phase I/II trial. J Urol. 2011;185:1246–54.
Curiel L, Chavrier F, Gignoux B, Pichardo S, Chesnais S, Chapelon JY. Experimental evaluation of lesion prediction modelling in the presence of cavitation bubbles: intended for high-intensity focused ultrasound prostate treatment. Med Biol Eng Comput. 2004;42:44–54.
Shoji S, Hashimoto A, Nakamoto M, et al. Morphological analysis of the effects of intraoperative transrectal compression of the prostate during high-intensity focused ultrasound for localized prostate cancer. Int J Urol. 2015;22:563–71.
Shoji S, Hiraiwa S, Endo J, et al. Manually controlled targeted prostate biopsy with real-time fusion imaging of multiparametric magnetic resonance imaging and transrectal ultrasound: an early experience. Int J Urol. 2015;22:173–8.
Shoji S, Hiraiwa S, Ogawa T, et al. Accuracy of real-time magnetic resonance imaging-transrectal ultrasound fusion image-guided transperineal target biopsy with needle tracking with a mechanical position-encoded stepper in detecting significant prostate cancer in biopsy-naive men. Int J Urol. 2017;24:288–94.
Kasivisvanathan V, Rannikko AS, Borghi M, et al. MRI-targeted or standard biopsy for prostate-cancer diagnosis. N Engl J Med. 2018;378:1767–77.
Shoji S. Magnetic resonance imaging-transrectal ultrasound fusion image-guided prostate biopsy: current status of the cancer detection and the prospects of tailor-made medicine of the prostate cancer. Investig Clin Urol. 2019;60:4–13.
Bahn DK, Silverman P, Lee F Sr, Badalament R, Bahn ED, Rewcastle JC. Focal prostate cryoablation: initial results show cancer control and potency preservation. J Endourol. 2006;20:688–92.
Consensus statement: guidelines for PSA following radiation therapy. American Society for Therapeutic Radiology and Oncology Consensus Panel. Int J Radiat Oncol Biol Phys. 1997;37:1035–41.
Muto S, Yoshii T, Saito K, Kamiyama Y, Ide H, Horie S. Focal therapy with high-intensity-focused ultrasound in the treatment of localized prostate cancer. Jpn J Clin Oncol. 2008;38:192–9.
Shoji S, Nakano M, Fujikawa H, et al. Urethra-sparing high-intensity focused ultrasound for localized prostate cancer: functional and oncological outcomes. Int J Urol. 2015;22:1043–9.
Roach M 3rd, Hanks G, Thames H Jr, et al. Defining biochemical failure following radiotherapy with or without hormonal therapy in men with clinically localized prostate cancer: recommendations of the RTOG-ASTRO Phoenix Consensus Conference. Int J Radiat Oncol Biol Phys. 2006;65:965–74.
Ahmed HU, Dickinson L, Charman S, et al. Focal ablation targeted to the index lesion in multifocal localised prostate cancer: a prospective development study. Eur Urol. 2015;68:927–36.
Feijoo ER, Sivaraman A, Barret E, et al. Focal high-intensity focused ultrasound targeted hemiablation for unilateral prostate cancer: a prospective evaluation of oncologic and functional outcomes. Eur Urol. 2016;69:214–20.
van Velthoven R, Aoun F, Marcelis Q, et al. A prospective clinical trial of HIFU hemiablation for clinically localized prostate cancer. Prostate Cancer Prostatic Dis. 2016;19:79–83.
Rischmann P, Gelet A, Riche B, et al. Focal high intensity focused ultrasound of unilateral localized prostate cancer: a prospective multicentric hemiablation study of 111 patients. Eur Urol. 2017;71:267–73.
Guillaumier S, Peters M, Arya M, et al. A multicentre study of 5-year outcomes following focal therapy in treating clinically significant nonmetastatic prostate cancer. Eur Urol. 2018;74:422–9.
Ganzer R, Hadaschik B, Pahernik S, et al. Prospective multicenter phase ii study on focal therapy (hemiablation) of the prostate with high intensity focused ultrasound. J Urol. 2018;199:983–9.
Johnston MJ, Emara A, Noureldin M, Bott S, Hindley RG. Focal High-intensity focussed ultrasound partial gland ablation for the treatment of localised prostate cancer: a report of medium-term outcomes from a single-center in the United Kingdom. Urology. 2019;133:175–81.
Stabile A, Orczyk C, Hosking-Jervis F, et al. Medium-term oncological outcomes in a large cohort of men treated with either focal or hemi-ablation using high-intensity focused ultrasonography for primary localized prostate cancer. BJU Int. 2019;124:431–40.
Abreu AL, Peretsman S, Iwata A, et al. High intensity focused ultrasound hemigland ablation for prostate cancer: initial outcomes of a United States series. J Urol. 2020;204:741–7.
Eggener SE, Scardino PT, Carroll PR, et al. Focal therapy for localized prostate cancer: a critical appraisal of rationale and modalities. J Urol. 2007;178:2260–7.
Hanada I, Shoji S, Takeda K, et al. Significant impact of the anterior transition zone portion treatment on urinary function after focal therapy with high-intensity focused ultrasound for prostate cancer. J Endourol. 2021;35:951–60.
He Y, Tan P, He M, et al. The primary treatment of prostate cancer with high-intensity focused ultrasound: a systematic review and meta-analysis. Medicine (Baltimore). 2020;99: e22610.
Faure Walker NA, Norris JM, Shah TT, et al. A comparison of time taken to return to baseline erectile function following focal and whole gland ablative therapies for localized prostate cancer: a systematic review. Urol Oncol. 2018;36:67–76.
Hofman MS, Violet J, Hicks RJ, et al. [(177)Lu]-PSMA-617 radionuclide treatment in patients with metastatic castration-resistant prostate cancer (LuPSMA trial): a single-centre, single-arm, phase 2 study. Lancet Oncol. 2018;19:825–33.
Kirkham AP, Emberton M, Hoh IM, Illing RO, Freeman AA, Allen C. MR imaging of prostate after treatment with high-intensity focused ultrasound. Radiology. 2008;246:833–44.
Scheltema MJ, Tay KJ, Postema AW, et al. Utilization of multiparametric prostate magnetic resonance imaging in clinical practice and focal therapy: report from a Delphi consensus project. World J Urol. 2017;35:695–701.
Donaldson IA, Alonzi R, Barratt D, et al. Focal therapy: patients, interventions, and outcomes—a report from a consensus meeting. Eur Urol. 2015;67:771–7.
Huber PM, Afzal N, Arya M, et al. Prostate specific antigen criteria to diagnose failure of cancer control following focal therapy of nonmetastatic prostate cancer using high intensity focused ultrasound. J Urol. 2020;203:734–42.
Weinreb JC, Barentsz JO, Choyke PL, et al. PI-RADS prostate imaging—reporting and data system: 2015, version 2. Eur Urol. 2016;69:16–40.
Shoji S, Hashimoto A, Nakamura T, et al. Novel application of three-dimensional shear wave elastography in the detection of clinically significant prostate cancer. Biomed Rep. 2018;8:373–7.
SonaCare Medical homepage; 2021. https://sonacaremedical.com/surgeons/our-products/sonablate.
Igarasihi R, Koizumi N, Nishiyama Y, Tomita K, Shigenari Y, Shoji S. Sagittal alignment in an MR-TRUS fusion biopsy using only the prostate contour in the axial image. ROBOMECH J. 2020;7:4.
Scheltema MJ, Chang JI, Bohm M, et al. Pair-matched patient-reported quality of life and early oncological control following focal irreversible electroporation versus robot-assisted radical prostatectomy. World J Urol. 2018;36:1383–9.
Zheng X, Jin K, Qiu S, et al. Focal laser ablation versus radical prostatectomy for localized prostate cancer: survival outcomes from a matched cohort. Clin Genitourin Cancer. 2019;17:464–9.
van der Poel HG, van den Bergh RCN, Briers E, et al. Focal therapy in primary localised prostate cancer: the European Association of Urology position in 2018. Eur Urol. 2018;74:84–91.
Funding
This research received no external funding.
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
Conflict of interest
The authors declare no conflicts of interest.
Informed consent
Not applicable.
Institutional Review Board statement
Not applicable.
Informed consent
Not applicable.
Additional information
Publisher's Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
About this article
Cite this article
Shoji, S., Koizumi, N., Yuzuriha, S. et al. Development and future prospective of treatment for localized prostate cancer with high-intensity focused ultrasound. J Med Ultrasonics (2022). https://doi.org/10.1007/s10396-021-01183-2
Received:
Accepted:
Published:
DOI: https://doi.org/10.1007/s10396-021-01183-2