Abstract
Purpose
Focal therapy (FT) for localized prostate cancer (PCa) is only recommended within the context of clinical trials by international guidelines. We aimed to investigate oncological follow-up and safety data of focal high-intensity focused ultrasound (HIFU) treatment.
Methods
We conducted a single-center prospective study of 29 patients with PCa treated with (focal) HIFU between 2016 and 2021. Inclusion criteria were unilateral PCa detected by mpMRI-US-fusion prostate biopsy and maximum prostate specific antigen (PSA) of 15 ng/ml. Follow-up included mpMRI-US fusion-re-biopsies 12 and 24 months after HIFU. No re-treatment of HIFU was allowed. The primary endpoint was failure-free survival (FFS), defined as freedom from intervention due to cancer progression.
Results
Median follow-up of all patients was 23 months, median age was 67 years and median preoperative PSA was 6.8 ng/ml. One year after HIFU treatment PCa was still detected in 13/ 29 patients histologically (44.8%). Two years after HIFU another 7/29 patients (24.1%) were diagnosed with PCa. Until now, PCa recurrence was detected in 11/29 patients (37.93%) which represents an FFS rate of 62%.One patient developed local metastatic disease 2 years after focal HIFU. Adverse events (AE) were low with 70% of patients remaining with sufficient erectile function for intercourse and 97% reporting full maintenance of urinary continence.
Conclusion
HIFU treatment in carefully selected patients is feasible. However, HIFU was oncologically not as safe as expected because of progression rates of 37.93% and risk of progression towards metastatic disease. Thus, we stopped usage of HIFU in our department.
Similar content being viewed by others
Avoid common mistakes on your manuscript.
Introduction
Focal therapy (FT) for prostate cancer (PCa) gained large interest by urologists and patients in treatment of low and intermediate-risk disease with the aim to provide equivalent oncological safety while reducing adverse events (AE) due to radical treatment [1]. The increased interest for FT can be explained by the growing number of younger patients who are identified at an earlier stage with localized PCa and small-volume prostate lesions due to the successful screening programs [2].
Most FT are based on ablative technologies, in particular high-intensity focused ultrasound (HIFU), cryotherapy, photodynamic therapy, electroporation, and focal radiation therapy RT by brachytherapy, for example [3]. In brief, HIFU is the most widely used technology with highest number of clinical retrospective data available. HIFU technology uses a transducer that ablates prostate tissue up to 65 degrees Celsius (149 degrees Fahrenheit), destroying malignant tumor cells through shear forces [4].
Currently, FTs are still defined in oncological guidelines as experimental treatment options that should only be performed in the context of clinical trials due to the significant lack of robust prospective clinical trials [5]. Nevertheless, large surveys in western urological communities’ report that every second urologist in Europe and one of four urologists in the United States recommend and perform FT, even outside clinical trials [6].
The main argument for HIFU is based on the index lesion theory which states that there is a pre-dominant focus of PCa causing local and systemic progression of the disease [7]. Consequently, FT is selectively treating this primary tumor focus while protecting presumably non-affected prostate tissue and leaving insignificant foci under surveillance. Pretherapeutic multiparametric MRI (mpMRI) and mpMRI-targeted biopsy represents the fundamental diagnostic technique pre-selecting patients and monitoring treatment outcomes. Multiple studies have reported high sensitivity (up to 90%) for mpMRI-targeted in combination with systematic biopsies in detecting significant PCa lesions [8]. Consequently, there is a remaining diagnostic uncertainty of mpMRI between 9 and 11% to miss significant PCa (ISUP grade ≥ 2) [9, 10]. Even though PCa is considered a multifocal disease, various studies reported a limited involvement to a singular lesion in 13–38%, and unilateral involvement in 19–63% [11, 12].
We aimed to assess the clinical outcome of patients treated by FT using HIFU in a prospective trial using rigorous inclusion and follow-up criteria. Based on previous HIFU data, we expected to reduce the risk of disease progression using HIFU only in carefully selected patients while reducing AE compared to standard recommended therapies like RP and RT.
Patients and methods
This controlled, prospective, non-randomized, phase 2 clinical study was carried out in a single European institution between December 2016 and October 2021. Follow-up is still ongoing. All patients gave written informed consent and were extensively informed about established treatment recommendations of RP or RT. The local ethical board approved the study (2019-14595). All patients received mpMRI of the prostate, followed by mpMRI-ultrasound (US)-fusion prostate biopsy of suspicious lesions with a score of ≥ 3 on the Prostate Imaging-Reporting and Data System (PI-RADS). Additional 12 cores were taken for a systematic examination. Only patients who had been diagnosed with unilateral PCa of ISUP grade 1 to 3 were included in the study and treated with focal HIFU. Further inclusion criteria involved prostate specific antigen (PSA) ≤ 15 ng/ml, clinical tumor classification ≤ T2 and prostate volume of ≤ 90 ml due to the technical limitation in insufficiently reaching ventral gland areas with the rectal HIFU transducer. Afterwards all patients received HIFU Focal One ® (EDAP TMS SA) therapy.
Follow-up protocol included PSA blood tests every three months during the first 2 years after HIFU treatment. At first and second year after HIFU treatment mpMRI and MRI-US fusion biopsies were conducted. AE after treatment were documented, using standard Clavien-Dindo classification. Pre-therapeutic diagnostic procedures, HIFU treatment and follow-up protocols were conducted at the same center. As part of the study protocol, we set up a goal of maximum 20% progression to more aggressive treatments, as this is a reasonable goal to achieve benefits compared to progression risk of Active Surveillance (AS) and based on recommendations by expert consensus statements to define a good focal therapy center [13]. The study protocol was based on the international recommendation valid at that time. Thus, the following PSA levels after HIFU treatment were individually evaluated in our multidisciplinary tumor board before performing re-biopsy to define treatment failure, as there was no established threshold for the PSA level defining treatment failure: rise of PSA above patient baseline PSA value and significant increase of PSA as compared to PSA nadir [13, 14]. If the PSA level increased suspiciously, mpMRI-targeted biopsy was recommended. Finally, metastatic progression during follow-up was defined as criteria to stop the trial.
As a unique exception from other centers, we strictly excluded focal HIFU retreatments in our protocol [15]. We also excluded patients with any previous therapy for PCa (AS, RT, hormone therapy), patients without prostate-limited disease preoperatively (in terms of extracapsular extension, seminal vesicle invasion or lymph nodes metastases), as well as patients diagnosed with PCa after transurethral resection of the prostate.
First, pre-interventional patient characteristics such as age at intervention, PSA level, prostate volume, HIFU therapy (hemi-ablation vs. focal ablation), PI-RADS classification, Gleason grading, number of positive cores in the targeted biopsy cores and number of positive cores in the systematic biopsy cores were described and stratified according to cancer recurrence at follow-up. Failure free survival (FFS), defined as freedom from any further intervention (e.g., RP or RT) due to cancer progression, was the primary outcome of the study. Secondary outcomes included total PSA levels, PSA nadir, area of recurrence diagnosed in mpMRI as part of follow-up and AE.
Statistical analysis was performed using IBM SPSS Statistics Version 27 (Armonk, NY: IBM Corp.). Descriptive statistics were reported as frequencies and proportions, continuous variables were presented as medians ± interquartile range (IQR, 25–75). Continuous variables were compared using the Mann–Whitney U test. FFS was demonstrated by Kaplan–Meier curves.
Results
Baseline characteristics of the study population are summarized in Table 1. Overall, a total of 29 men were enrolled in this study. Follow-up and AS are still ongoing. Median follow-up was 23 months and median age at time of focal HIFU treatment was 67 years. Median time to reach PSA nadir was six months.
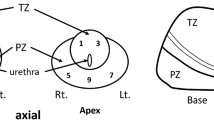
At first-year follow-up, out of 24 patients who underwent first re-biopsy 14 patients (44.8%) were diagnosed with PCa. Five of these patients (17.2% related to overall study population) were recommended RP or RT because of progression and unsuitability for continuing AS strategy (Table 1) [16]. At 2-year follow-up 12 patients received targeted prostate biopsy with 12-fold systematic biopsy in case of mpMRI lesions. Seven patients out of 12 (24.1%) were diagnosed with PCa. Six of these 12 patients (20.7% of overall population) were recommended RP or RT because of progression. Among all patients with PCa recurrence 2 years after HIFU treatment, six patients (40%) were detected with outfield recurrence regarding initially treated PCa lesions, while five patients (33.33%) showed infield and outfield lesions. Thus, 11 patients (73.33%) developed outfield PCa lesions in our study cohort (Fig. 1 of the Supplementary Material shows a workflow of patients’ follow-up).
In summary, 2 years after HIFU, we recommended RT or RP treatment in 11 cases which represents a drop-out rate of 37.93% and an FFS rate of 62%, respectively (Fig. 1). Median time until study drop-out was 22 months (standard deviation of 8.77, min. 4 months, max. 27 months).
Notably, we report about one patient who developed lymphatic metastases after focal HIFU treatment. Baseline characteristics of this patient were the following: iPSA of 9.3 ng/ml, prostate volume of 42 ml and ISUP grade 2 unilateral PCa. Initial mpMRI revealed inconspicuous lymph nodes. He underwent HIFU hemi-ablation in March 2020. After initial mpMRI-US fusion biopsy, we performed follow-up biopsy in March 2021 according to study protocol. Here, we detected only one positive biopsy with ISUP grade 1 (< 5% volume of biopsy), thus continued with AS according to guidelines. After reaching low PSA 0.84 ng/ ml nadir, PSA level eventually rose to 6 ng/ml 18 months after HIFU. Two-year follow-up mpMRI demonstrated conspicuous pelvic lymph nodes. Thus, he underwent immediate DaVinci-assisted RP with pelvic lymph node dissection in April 2022. Final pathology revealed pT3 pN1 (6 positive lymph nodes) status. Additional PSMA-PET CT-scan confirmed even more cancerous pelvic nodes. Consequently, multimodal adjuvant treatment was recommended with RT plus androgen deprivation therapy.
As a result of the high clinical failure rate of HIFU treatment despite current standard diagnostic methods, with one patient even progressing to metastatic palliative disease, we stopped this clinical study for HIFU treatment in our department because of oncologic safety concerns.
Finally, the most frequent AE, namely gross haematuria, erectile dysfunction, acute urinary retention, urinary tract infection, and urge incontinence are reported in Table 1. Grade 3 Clavien–Dindo complications occurred in 14% of patients. Four patients (14%) had no AE at all. Notably, after 4 years 69% of patients still had full erectile function and 97% reported no effects on their continence.
Discussion
In our prospective, single-center clinical study of HIFU treatment in unilateral localized PCa we demonstrate high progression rates with overall FFS of only 62%. Despite lower AE compared to RP and RT we had to stop HIFU treatment in localized unilateral PCa because of oncologic safety concerns.
HIFU treatment is based on index lesion theory which has not been properly confirmed, yet. As long as several large pathological analyses of patients undergoing RP reveal multifocal disease in up to 80%, we have to address this knowledge to our patients treated by FT [17]. In our study, 73.33% of patients treated with HIFU revealed outfield PCa lesions in first- or second-year re-biopsies. These findings contradict the index lesion theory and are consistent with larger pathological analyses which support the existing consensus of PCa as multifocal disease [11, 12].
Moreover, high accuracy in optimal patient selection is extremely important for any FT to detect focal disease based on index lesion theory, which is primarily based on mpMRI-US fusion biopsy. However, the accuracy of mpMRI in defining clinically significant PCa depends on several variables, as well as interobserver and interoperator variability, which may result in substantial reduction in negative predictive value [8].
Despite our efforts in maximal accurate patient selection to address the underlying index theory of FT, we report an unexpected high number of tumor regression with median FFS rate of approximately 62% of total study cohort (median time until study drop-out of 22 months). Most importantly, one patient developed metastatic disease leading to palliative care. Comparing our results with those of other centers, only few midterm follow-up results are published reporting significant treatment failure and need for re-treatment. One of the largest cohorts has been published in 2019 with a total of 1032 men treated with HIFU between 2005 and 2017 with median follow-up of 36 months [18]. In this study, only 46% of men were free from any need for re-treatment during median follow-up. Approximately 70% of patients receiving any kind of re-treatment underwent a second FT. When regarding men undergoing at least one follow-up biopsy, only 35% were free from clinically significant PCa at 96 months. Another evaluation from 13 centers with 1379 patients and overall median follow-up of 32 months reported 7-years failure-free survival of 69% (64–74%) [19].
Notably, we did not include second HIFU treatment in our study protocol because it prevents causal relationships of cause and effect. Second, we regard high rates of re-treatment by 70% as a critical issue that needs to be discussed, especially when 5-year progression-free survival rates for RP above 80% are documented in large prospective trials [20, 21]. In our study population 37.93% of patients were recommended RP or RT due to tumor progression. Also, progression occurred in initial HIFU treatment areas as well as new areas of the prostate gland which we regard as significant risk to patients’ safety. Moreover, there is no clear consensus on PSA thresholds for acceptable rates of progression under FT [22].
Regarding further smaller study cohorts, PCa recurrence and progression rates after FT treatment also varied from 20 to 30% [23]. These numbers may also reflect the heterogenous and partially unclear inclusion and treatment criteria [24].
Ultimately, our results strengthen the need to increase diagnostic accuracy to detect localized PCa. This could be achieved by further narrowing the inclusion criteria in terms of more localized, small-volume PCa. We propose to establish HIFU study protocols including PSMA PET-CT. Based on the phase III “proPSMA” trial, there is strong evidence for significant improvement in identifying pelvic nodal and distant metastatic PCa compared to conventional CT and bone scanning [25]. When combined with mpMRI-US-fusion prostate biopsy, PSMA PET-CT may lead to improved diagnostic accuracy, thereby reducing outfield recurrences when FT is used.
Nevertheless, we can confirm overall low rates of AE as compared RP or RT [18, 26]. Approximately 70% of our patients maintained full erectile function and 97% reported maintenance of urinary continence while 14% reported no AE at all.
Additionally, we need to address AS treatment for patients with low-risk PCa. Compared to definitive treatment or focal HIFU, AS does not have Clavien ≥ 3 AEs and provides high evidence-based long-term follow-up data showing comparable overall survival in appropriately selected patients. Disease progression rates of AS leading to definitive treatment might also be high, up to approximately 60% in long-term follow-up of 10 years and median FFS up to 8.5 years [27, 28].
Finally, we encourage technical improvements of FT to further increase the effectiveness of ablative technologies to achieve even better local destruction of PCa cells, while better protecting the surrounding tissue, including prostate nerve bundle preservation. Moreover, the usage of HIFU is limited in treatment of prostates larger than 40 ccm or to lesions within 4 cm from the treatment site [29].
We are aware of the limitations of our study, in particular the limited sample size. However, we had to stop the trial after treating 29 patients based on our trial protocol. Thus, we are not able to perform an in-depth multiple logistic regression analysis to identify, for example, risk factors for failure after HIFU treatment. To further evaluate these factors, we would need at least 40–50 patients per parameter. Furthermore, mpMRI-US-fused prostate biopsies were conducted by several urologists and MRI was analyzed by different radiologists, thereby interobserver bias is of specific relevance. Nevertheless, our results resemble real world experience which we believe is very important for colleagues in urology and their daily treatment recommendations.
Conclusion
In conclusion, FT in PCa using HIFU demonstrated good functional results in patients. However, HIFU was not as safe oncologically as expected, with recurrence and progression rates of 37.93% and risk of disease progression to metastatic disease. We strongly support the further scientific evaluation of FT, but until oncological risks cannot be safely reduced, we no longer recommend HIFU treatment in our department at this time.
References
Beerlage HP, Thüroff S, Madersbacher S et al (2000) Current status of minimally invasive treatment options for localized prostate carcinoma. Eur Urol 37:2–13
Mouraviev V, Mayes JM, Polascik TJ (2009) Pathologic basis of focal therapy for early-stage prostate cancer. Nat Rev Urol 6:205–215
Valerio M, Cerantola Y, Eggener SE et al (2017) New and established technology in focal ablation of the prostate: a systematic review. Eur Urol 71:17–34
Madersbacher S, Marberger M (2003) High-energy shockwaves and extracorporeal high-intensity focused ultrasound. J Endourol 17:667–672
MacLennan S, Williamson PR, Bekema H et al (2017) A core outcome set for localised prostate cancer effectiveness trials. BJU Int 120:E64–E79
Marra G, Ploussard G, Ost P et al (2018) Focal therapy in localised prostate cancer: real-world urological perspective explored in a cross-sectional European survey. Urol Oncol 36:529.e511-529.e522
Ahmed HU (2009) The index lesion and the origin of prostate cancer. N Engl J Med 361:1704–1706
Moldovan PC, Van den Broeck T, Sylvester R et al (2017) What is the negative predictive value of multiparametric magnetic resonance imaging in excluding prostate cancer at biopsy? A systematic review and meta-analysis from the European Association of Urology Prostate Cancer Guidelines Panel. Eur Urol 72:250–266
Fütterer JJ, Briganti A, De Visschere P et al (2015) Can clinically significant prostate cancer be detected with multiparametric magnetic resonance imaging? A systematic review of the literature. Eur Urol 68:1045–1053
Simmons LAM, Kanthabalan A, Arya M et al (2017) The PICTURE study: diagnostic accuracy of multiparametric MRI in men requiring a repeat prostate biopsy. Br J Cancer 116:1159–1165
Cheng L, Jones TD, Pan CX et al (2005) Anatomic distribution and pathologic characterization of small-volume prostate cancer (< 0.5 ml) in whole-mount prostatectomy specimens. Mod Pathol 18:1022–1026
Polascik TJ, Mouraviev V (2008) Focal therapy for prostate cancer. Curr Opin Urol 18:269–274
van den Bos W, Muller BG, Ahmed H et al (2014) Focal therapy in prostate cancer: international multidisciplinary consensus on trial design. Eur Urol 65:1078–1083
Ganzer R, Rogenhofer S, Walter B et al (2008) PSA nadir is a significant predictor of treatment failure after high-intensity focussed ultrasound (HIFU) treatment of localised prostate cancer. Eur Urol 53:547–553
Resnik DB, Shamoo AE (2017) Reproducibility and Research Integrity. Account Res 24:116–123
Willemse PM, Davis NF, Grivas N et al (2022) Systematic review of active surveillance for clinically localised prostate cancer to develop recommendations regarding inclusion of intermediate-risk disease, biopsy characteristics at inclusion and monitoring, and surveillance repeat biopsy strategy. Eur Urol 81:337–346
Mouraviev V, Mayes JM, Sun L et al (2007) Prostate cancer laterality as a rationale of focal ablative therapy for the treatment of clinically localized prostate cancer. Cancer 110:906–910
Stabile A, Orczyk C, Hosking-Jervis F et al (2019) Medium-term oncological outcomes in a large cohort of men treated with either focal or hemi-ablation using high-intensity focused ultrasonography for primary localized prostate cancer. BJU Int 124:431–440
Reddy D, Peters M, Shah TT et al (2022) Cancer control outcomes following focal therapy using high-intensity focused ultrasound in 1379 men with nonmetastatic prostate cancer: a multi-institute 15-year experience. Eur Urol 81:407–413
Vernooij RW, Lancee M, Cleves A et al (2020) Radical prostatectomy versus deferred treatment for localised prostate cancer. Cochrane Database Syst Rev 6:CD006590
Wilt TJ, Jones KM, Barry MJ et al (2017) Follow-up of prostatectomy versus observation for early prostate cancer. N Engl J Med 377:132–142
Tay KJ, Scheltema MJ, Ahmed HU et al (2017) Patient selection for prostate focal therapy in the era of active surveillance: an International Delphi Consensus Project. Prostate Cancer Prostatic Dis 20:294–299
Shah TT, Peters M, Eldred-Evans D et al (2019) Early-medium-term outcomes of primary focal cryotherapy to treat nonmetastatic clinically significant prostate cancer from a prospective multicentre registry. Eur Urol 76:98–105
Sivaraman A, Barret E (2016) Focal therapy for prostate cancer: an “À la Carte” approach. Eur Urol 69:973–975
Hofman MS, Lawrentschuk N, Francis RJ et al (2020) Prostate-specific membrane antigen PET-CT in patients with high-risk prostate cancer before curative-intent surgery or radiotherapy (proPSMA): a prospective, randomised, multicentre study. Lancet 395:1208–1216
Valerio M, Ahmed HU, Emberton M et al (2014) The role of focal therapy in the management of localised prostate cancer: a systematic review. Eur Urol 66:732–751
Hamdy FC, Donovan JL, Lane JA et al (2016) 10-year outcomes after monitoring, surgery, or radiotherapy for localized prostate cancer. N Engl J Med 375:1415–1424
Wilt TJ, Vo TN, Langsetmo L et al (2020) Radical prostatectomy or observation for clinically localized prostate cancer: extended follow-up of the prostate cancer intervention versus observation trial (PIVOT). Eur Urol 77:713–724
Lodeizen O, de Bruin M, Eggener S et al (2019) Ablation energies for focal treatment of prostate cancer. World J Urol 37:409–418
Acknowledgements
The authors wish to thank all patients for their contribution.
Funding
Open Access funding enabled and organized by Projekt DEAL. This research received no specific grant from any funding agency in the public, commercial, or not-for-profit sectors. The authors declare no conflicts of interest in preparing this article.
Author information
Authors and Affiliations
Contributions
GD: Manuscript writing, Manuscript editing, Data management, Data analysis (corresponding author). KB: Protocol/ Project development, Manuscript editing. MH: Manuscript editing. PS: Manuscript editing. MPB: Manuscript editing. RM: Manuscript editing. IT: Manuscript editing. H: Manuscript editing. TH: Protocol/ Project development, Manuscript editing, Data collection, Data management.
Corresponding author
Ethics declarations
Conflict of interest
All authors certify that they have no affiliations with, or involvement in any organization, or entity with any financial interest, or non-financial interest in the subject matter or materials discussed in this manuscript. Furthermore, the authors have no competing interests to declare that are relevant to the content of this article.
Ethical approval
The study was approved by the Ethics Committee of the Rhineland-Palatinate State Medical Association (application number: 2019-14595). Our research was conducted ethically in accordance with the World Medical Association Declaration of Helsinki. All procedures performed in this study involving human participants were in accordance with the ethical standards of the institutional and national research committee and with the 1964 Declaration of Helsinki and its later amendments or comparable ethical standards.
Consent to participate
Informed consent was obtained from all individual participants included in the study.
Consent to publish
Informed consent was obtained from all participants, regarding publishing their data.
Additional information
Publisher's Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Supplementary Information
Below is the link to the electronic supplementary material.
345_2023_4352_MOESM1_ESM.docx
Supplementary file1 Figure 1: Workflow of 29 patients who received HIFU therapy in our institution. All of them harboured prostate cancer; 20 patients were diagnosed with ISUP 1, eight patients with ISUP 2 and one patient with ISUP 3 prostate cancer. (DOCX 102 kb)
Rights and permissions
Open Access This article is licensed under a Creative Commons Attribution 4.0 International License, which permits use, sharing, adaptation, distribution and reproduction in any medium or format, as long as you give appropriate credit to the original author(s) and the source, provide a link to the Creative Commons licence, and indicate if changes were made. The images or other third party material in this article are included in the article's Creative Commons licence, unless indicated otherwise in a credit line to the material. If material is not included in the article's Creative Commons licence and your intended use is not permitted by statutory regulation or exceeds the permitted use, you will need to obtain permission directly from the copyright holder. To view a copy of this licence, visit http://creativecommons.org/licenses/by/4.0/.
About this article
Cite this article
Duwe, G., Boehm, K., Haack, M. et al. Single-center, prospective phase 2 trial of high-intensity focused ultrasound (HIFU) in patients with unilateral localized prostate cancer: good functional results but oncologically not as safe as expected. World J Urol 41, 1293–1299 (2023). https://doi.org/10.1007/s00345-023-04352-9
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s00345-023-04352-9