Abstract
Objectives
To compare Dixon water-fat suppression with spectral pre-saturation with inversion recovery (SPIR) at 3T for coronary magnetic resonance angiography (MRA) and to demonstrate the feasibility of fat suppressed coronary MRA at 3T without administration of a contrast agent.
Materials and methods
Coronary MRA with Dixon water-fat separation or with SPIR fat suppression was compared on a 3T scanner equipped with a 32-channel cardiac receiver coil. Eight healthy volunteers were examined. Contrast-to-noise ratio (CNR), signal-to-noise ratio (SNR), right coronary artery (RCA), and left anterior descending (LAD) coronary artery sharpness and length were measured and statistically compared. Two experienced cardiologists graded the visual image quality of reformatted Dixon and SPIR images (1: poor quality to 5: excellent quality).
Results
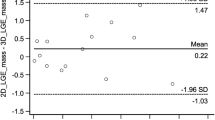
Coronary MRA images in healthy volunteers showed improved contrast with the Dixon technique compared to SPIR (CNR blood-fat: Dixon = 14.9 ± 2.9 and SPIR = 13.9 ± 2.1; p = 0.08, CNR blood-myocardium: Dixon = 10.2 ± 2.7 and SPIR = 9.11 ± 2.6; p = 0.1). The Dixon method led to similar fat suppression (fat SNR with Dixon: 2.1 ± 0.5 vs. SPIR: 2.4 ± 1.2, p = 0.3), but resulted in significantly increased SNR of blood (blood SNR with Dixon: 19.9 ± 4.5 vs. SPIR: 15.5 ± 3.1, p < 0.05). This means the residual fat signal is slightly lower with the Dixon compared to the SIPR technique (although not significant), while the SNR of blood is significantly higher with the Dixon technique. Vessel sharpness of the RCA was similar for Dixon and SPIR (57 ± 7 % vs. 56 ± 9 %, p = 0.2), while the RCA visualized vessel length was increased compared to SPIR fat suppression (107 ± 21 vs. 101 ± 21 mm, p < 0.001). For the LAD, vessel sharpness (50 ± 13 % vs. 50 ± 7 %, p = 0.4) and vessel length (92 ± 46 vs. 90 ± 47 mm, p = 0.4) were similar with both techniques. Consequently, the Dixon technique resulted in an improved visual score of the coronary arteries in the water fat separated images of healthy subjects (RCA: 4.6 ± 0.5 vs. 4.1 ± 0.7, p = 0.01, LAD: 4.1 ± 0.7 vs. 3.5 ± 0.8, p = 0.007).
Conclusions
Dixon water-fat separation can significantly improve coronary artery image quality without the use of a contrast agent at 3T.
Similar content being viewed by others
Introduction
Coronary artery magnetic resonance angiography (CMRA) requires effective fat suppression as coronary arteries are embedded in epicardial fat. Unwanted signal arising from fat can compromise vessel delineation and decrease the diagnostic value of CMRA [1].
Various fat suppression techniques have been proposed for CMRA such as short tau inversion recovery (STIR) and spectral presaturation with inversion recovery (SPIR) [2]. These methods are based on the relaxation time (T1) as well as chemical shift differences between fat and water. The frequency selective RF pulse of the SPIR technique only saturates the magnetization of fat while maintaining the magnetization of water and data acquisition begins immediately after the fat saturation pulse. In contrast, the STIR prepulse inverts both water and fat magnetization and imaging commences when the magnetization of fat is zero. However, each of these methods has specific drawbacks that may cause spatial misregisteration artifacts or sensitivity to B 0 or B 1 field inhomogeneities. Thus, it is important to develop and evaluate methods that may circumvent these drawbacks. STIR fat suppression suppresses the magnetization of fat and tissues which have similar short T 1. As a result STIR is not recommended to be used in concert with a contrast agent. SPIR images have higher SNR compared to STIR images because the STIR prepulse inverts both the water and fat magnetization. For these reasons the SPIR technique has become the preferable fat suppression method for coronary artery imaging.
MRI chemical shift based water fat separation methods such as the Dixon method (first described by Dixon in 1984 [3]) provide excellent water and fat separation by acquiring images at carefully chosen echo times and using pixel by pixel image algebra. It provides additional diagnostic benefits (fat image) compared to conventional fat-saturation techniques [3–6]. The Dixon method has been shown to increase the image quality of whole heart CMRA at 1.5T [7]. Unlike other methods of water-fat separation that selectively excite water or suppress fat signal, the Dixon technique takes advantage of the phase shifts due to the water-fat resonance frequency difference in order to separate water from fat. In addition, the key advantage of the Dixon method is its tolerance to the main field inhomogeneity. This is achieved by including the underlying B0 distribution into the signal model avoiding adverse effects on the signal separation process this way. Furthermore, the separation of water and fat by generating water and fat only images may reduce the sensitivity to motion artifacts in the water images as those artifacts often arise from residual fat signal in the chest wall that subsequently may lead to ghosting artifacts if chest wall motion is not adequately corrected for.
The purpose of this study was to compare CMRA with Dixon water fat separation with SPIR fat suppression at 3T and to investigate the sensitivity of both methods to the larger field inhomogeneity at 3T without administration of a contrast agent.
Materials and methods
This work was performed using a 3T MR scanner (Achieva, Philips Healthcare, Best, the Netherlands) equipped with a 32-element cardiac coil for signal detection. Data were acquired in eight healthy adult subjects (six male, two female, mean age 36 ± 11 years). All subjects provided written informed consent and study was approved by the institutional review board. Imaging parameters of the SPIR and Dixon CMRA sequence were identical in healthy subjects. Every subject received two different scans: (1) conventional whole heart CMRA with SPIR fat suppression and (2) whole heart CMRA with two-point Dixon water fat separation in the same imaging session.
CMRA pulse sequences
In this study, a segmented Turbo Field (TFE) gradient echo sequence was used both for the Dixon and SPIR CMRA. TFE was chosen because T1-weighted gradient echo imaging has been found to be superior to balanced gradient echo imaging at high field strength [8]. A schematic of the imaging sequence is shown in Fig. 1. The 3D CMRA sequence with isotropic spatial resolution was preceded by a pencil beam navigator for prospective respiratory motion correction [9, 10] and by a T2prep prepulse (TET2prep = 50 ms) for suppression of signal from myocardium and venous blood (with short T 2 relaxation time) to improve contrast between arterial blood (T 2 = 250 ms) and myocardium (T 2 = 50 ms). Imaging was performed during the quiescent phase in mid-diastole and the gating window was 5 mm. Standard cardiac volume shim was used. Imaging parameters of the CMRA pulse sequence included: TR/TE = 4.1/1.7 ms for SPIR, TR/TE1/TE2 = 4.1/1.7/3.1 ms for Dixon, flip angle = 20°, acquisition window = 120 ms, slab thickness = 80–120 mm, FOV = 300 × 300 mm, matrix size = 448 × 448, in-plane resolution = 1.2 × 1.2 mm2, slice thickness = 1.2 mm, pixel bandwidth for SPIR = 1296 Hz/pixel and SENSE factor 2. Depending on the size of the heart, scans were performed either with 133 or 167 reconstructed slices. Images were acquired in the coronal plane with read-out in foot-head direction.
Imaging parameters were almost identical for the two-point Dixon and SPIR fat saturation. The readout gradient of the Dixon sequence consisted of two rephasing lobes with different polarity and echo times TE1 and TE2. In Dixon method the additional echo (TE1/TE2 = 1.7/3.1 ms) acquired did not alter the total scan time because the same repetition time (TR = 4.1 ms) was used for both methods to minimize parameter variations and to have comparable contrast and image quality. Bandwidth for the Dixon sequence was slightly higher to accommodate the two echoes and was 1568 Hz/pixel. Because of the two echoes and their actual timing, the SNR of the Dixon images is slightly higher (factor 1.2) than that of the SPIR images [11, 12]. Inline image reconstruction was performed to separate water and fat signal. Before separation of water and fat an appropriate phase correction is performed to eliminate phase errors induced by eddy currents [11].
Image analysis
Two expert readers (15 and 3 years of cardiac MRI experience), blinded to the methods used, scored the image quality for each dataset using a five-point scale system: 1, poor quality; 2, structured visible but markedly blurred; 3, anatomy visible, but with moderate blurring; 4, minimal blurring; 5, well defined borders of vessel sharpness. All images were reformatted using dedicated software [13] to compare coronary artery delineation. Vessel sharpness and visualized vessel length of the RCA and LAD were quantified with Soapbubble software [13]. SNR was determined in fat \(\left( {{\text{SNR}}_{\text{fat}} = \frac{{I_{\text{fat}} }}{{{\text{SDEV}}_{\text{fat}} }}} \right)\), blood and myocardium. Furthermore, CNR between blood, fat, \(\left( {{\text{CNR}}_{\text{blood, fat}} = \frac{{I_{\text{blood}} { - }I_{\text{fat}} }}{{ 0. 5 ( {\text{SDEV}}_{\text{blood}} {\text{ + SDEV}}_{\text{fat}} )}}} \right)\) and myocardium were calculated.
Statistical analysis
For statistical comparison a Wilcoxon Signed-Rank was used for the calculation of the image quality, whereas a t test was used for vessel sharpness and length. All measurements are presented as mean ± standard deviation and p ≤ 0.05 considered statistically significant.
Results
All scans were successfully performed and produced good quality images in all volunteers. The total scan time for 133 reconstructed slices was Dixon: 365 ± 58 s and SPIR: 368 ± 58 s) and for 167 reconstructed slices (Dixon: 434.5 ± 15 s and SPIR: 445 ± 1 s). The average navigator efficiency was 54 ± 11 % (range 37–73 %). Figure 2 shows representative CMRA images from four healthy volunteers for both Dixon water-fat separation and SPIR fat suppression. Figure 2 demonstrates that excellent coronary artery image quality can be obtained at 3T without the use of a contrast agent. Fat suppression and vessel delineation with Dixon was visually superior to the SPIR technique (Fig. 2). Furthermore, images acquired in healthy subjects with the two-point Dixon method scored higher image quality than those acquired with SPIR (RCA: 4.6 ± 0.5 vs. 4.1 ± 0.7, p = 0.01, LAD: 4.1 ± 0.7 vs. 3.5 ± 0.8, p = 0.007).
Reformatted whole heart CMRA using SPIR (first column) fat suppression and Dixon water (second column), fat (third column) separation in four representative volunteers. Arrows point to locations in the images where fat suppression was improved with the Dixon compared to the SPIR fat suppression method. Reformatted images demonstrate that fat suppression is good with both techniques at 3T without the use of a contrast agent. In addition, the Dixon technique provides a fat image which can be used for diagnostic purposes or to improve vessel tracking as distal segments are often displayed better in the fat images
Measured vessel length and sharpness of the RCA in healthy subjects acquired with both fat suppression methods are shown in Table 1. Vessel sharpness of the RCA acquired with the Dixon method was similar to SPIR fat suppression (57 ± 7 vs. 56 ± 9 %, p = 0.2). However, there were statistically significant differences found in the visualized vessel length for the Dixon compared to the SPIR fat suppression method (107 ± 21 vs. 101 ± 21 mm, p < 0.001). For LAD vessel sharpness (50 ± 13 vs. 50 ± 7 %, p = 0.4) and vessel length (92 ± 46 vs. 90 ± 47 mm, p = 0.4) both techniques performed equally well.
The Dixon method was found to lead to similar fat suppression but increased SNR of blood and myocardium compared to SPIR fat suppression (Table 1). There was a trend towards higher CNR between blood and fat using the Dixon method (p = 0.08).
Discussion
In this study, the two-point Dixon water-fat separation technique was compared with the SPIR fat suppression technique at 3T for non-contrast enhanced whole heart CMRA. The main findings of this study were that (1) there was improved image quality in terms of visual score, (2) there was a tendency for higher blood and myocardium SNR and blood/fat CNR, (3) longer visual vessel length and. Our findings are in agreement with a previous study at 1.5T where the Dixon water-fat separation technique helped to improve image quality of segmented TFE coronary MRA compared with SPIR fat suppressed balanced fast field echo (BTFE) CMRA [7].
Another advantage of the dual echo Dixon water fat separation technique compared to magnetization-prepared fat separation methods is that ghosting artifacts from not suppressed, moving, high intensity, chest wall fat only appears in the fat image and does not leak into the water image thereby minimizing sensitivity to breathing artifacts in the water image [7]. Because of the insensitivity of the chemical shift encoding to B 0 and B 1 inhomogeneities the robustness of Dixon fat suppression is better than that of SPIR at 3T. It has been shown that changing the direction of phase encoding in dual echo Dixon scans can reduce the ghosting level, increase the quality of the fat image and also reduce the motion sensitivity of the scan. Changing the phase encoding direction can increase scan time but if one is only interested in water images, image quality should be less dependent on the phase encoding direction [7]. Another advantage of Dixon-type fat-suppression strategy is its compatibility with steady-state acquisition, e.g. in cine-type acquisitions or recently proposed 4D coronary MRA [14, 15].
In the presence of B1 inhomogeneities (RF inhomogeneity), as typically encountered at 3T and higher field strengths, Dixon water fat separation should be superior to SPIR fat suppression because it is based on chemical shift difference and does not depend on the performance of saturation or inversion prepulses, which can be compromised by the transmit field inhomogeneity (B +1 ). In line with this, the overall performance of fat suppression was better for Dixon water-fat separation than for SPIR fat suppression in the current study.
We chose a wider receiver bandwidth for the Dixon compared to the SPIR to reduce chemical shifts artifacts and to allow faster data acquisition within the given sequence TR. Larger receiver bandwidth usually reduces SNR because more noise is included (SNR = 1/√rBW and chemical shift = 1/rBW), but this is compensated for by the dual echo acquisition and the noise averaging effect taking place in the Dixon reconstruction [11]. Moreover, due to its excitation bandwidth, the SPIR pulse may also saturate parts of the water peak, thereby reducing the SNR from the free water pool.
Although our data show no statistically significant differences between Dixon and SPIR in terms of coronary vessel sharpness, the two-point Dixon method improved the visual score and the visualized RCA length significantly.
Recent studies have demonstrated that cardiac fat may carry significant diagnostic value with a potential predictive value [7], such as better characterization of cardiac masses for identification of tumors, lipoma, and edema [16]. Visceral fat and obesity can cause different cardiovascular diseases such as cerebral vascular disease, coronary artery disease, and stroke [17–21]. Fibrofatty infiltrations of the myocardium have been found to be associated with a higher likelihood of sudden cardiac death [22] and arrythmogenic right ventricular cardiomyopathy (ARVC) is characterized pathologically by fibrofatty infiltration [23–26]. In addition, adipose tissue has been observed within the area of healed myocardial infarcts, with greater degree of fat volume in patients with coronary artery bypass graft surgery [27]. Moreover, pericardial fat volume is highly associated with atrial fibrillation (AF). For the above reasons, assessment of fatty infiltration by magnetic resonance imaging (MRI) may provide important diagnostic information for the detection and characterization of cardiovascular disease.
The additional fat data that is available with Dixon protocols may represent an important, until now clinically underused biomarker, and can be used to quantify the ratio of peri- to paracardial fat, and thus may enhance the diagnostic value of coronary MRA. In addition, as it is sometimes easier to find the tissue boundaries and the location of small epicardial vessels in the fat image rather than water image, the fat image also could be used to guide coronary artery segmentation. As a result the fat information can potentially be used for vessel tracking and characterization [7].
Contrast enhanced MR angiography (CE-MRA) techniques are widely used due to improved contrast-to-noise ratio (CNR) between blood and surrounding tissues, shorter examination times due to the ability to apply more imaging pulses because of shorter T1, better anatomical coverage and less flow artifacts compared to non-contrast MR angiography (NC-MRA). However, in high risk patients like patients with renal dysfunction or failure, NC-MRA is widely used. Moreover, NC-MRA does not require the perfect timing of the first pass of the contrast agent which can be challenging in the presence of cardiac or vascular disease. Furthermore contrast enhanced techniques are “single shot”, i.e., cannot be easily repeated, whereas NC-MRA allows multiple acquisitions if needed.
Limitations
We only investigated a small number of healthy subjects in this proof-of-concept study. Further evaluation is needed to assess the diagnostic accuracy of the Dixon technique in patient population undergoing invasive clinical coronary angiography. In addition, the Dixon technique can be combined with an inversion recovery pulse for using in contrast enhanced coronary. However, further study is needed to compare Dixon and SPIR fat suppression in the presence of a contrast agent as fat and blood signal may have similar T1 , and thus fat suppression becomes important to delineate efficiently epicardial fat from coronary blood.
Conclusions
We have demonstrated that the Dixon water-fat separation method provides improved CMRA image quality at 3T compared to the SPIR technique without the need of a contrast agent and may provide additional diagnostic information due to pericardial fat signal visualization without increasing the overall scan time.
References
Simon JH, Szumowski J (1992) Proton (fat/water) chemical shift imaging in medical magnetic resonance imaging. Current status. Invest Radiol 27:865–874
Kaldoudi E, Williams SC, Barker GJ et al (1993) A chemical shift selective inversion recovery sequence for fat-suppressed MRI: theory and experimental validation. Magn Reson Imaging 11:341–355
Dixon WT (1984) Simple proton spectroscopic imaging. Radiology 153:189–194
Glover GH, Schneider E (1991) Three-point Dixon technique for true water/fat decomposition with B 0 inhomogeneity correction. Magn Reson Med 18:371–383
Ma J (2008) Dixon techniques for water and fat imaging. J Magn Reson Imaging 28:543–558
Xiang QS, An L (1997) Water-fat imaging with direct phase encoding. J Magn Reson Imaging 7:1002–1015
Bornert P, Koken P, Nehrke K et al (2014) Water/fat-resolved whole-heart Dixon coronary MRA: an initial comparison. Magn Reson Med 71:156–163
Kaul MG, Stork A, Bansmann PM et al (2004) Evaluation of balanced steady-state free precession (TrueFISP) and K-space segmented gradient echo sequences for 3D coronary MR angiography with navigator gating at 3 Tesla. Rofo 176:1560–1565
Danias PG, Stuber M, Botnar RM et al (1999) Relationship between motion of coronary arteries and diaphragm during free breathing: lessons from real-time MR imaging. AJR Am J Roentgenol 172:1061–1065
Wang Y, Riederer SJ, Ehman RL (1995) Respiratory motion of the heart: kinematics and the implications for the spatial resolution in coronary imaging. Magn Reson Med 33:713–719
Eggers H, Brendel B, Duijndam A et al (2011) Dual-echo Dixon imaging with flexible choice of echo times. Magn Reson Med 65:96–107
Reeder SB, McKenzie CA, Pineda AR et al (2007) Water-fat separation with IDEAL gradient-echo imaging. J Magn Reson Imaging 25:644–652
Etienne A, Botnar RM, Van Muiswinkel AM et al (2002) “Soap-Bubble” visualization and quantitative analysis of 3D coronary magnetic resonance angiograms. Magn Reson Med 48:658–666
Pang J, Sharif B, Fan Z et al (2014) ECG and navigator-free four-dimensional whole-heart coronary MRA for simultaneous visualization of cardiac anatomy and function. Magn Reson Med 72:1208–1217
Coppo S, Piccini D, Bonanno G et al (2015) Free-running 4D whole-heart self-navigated golden angle MRI: initial results. Magn Reson Med 74:1306–1316
Kellman P, Hernando D, Shah S et al (2009) Multiecho dixon fat and water separation method for detecting fibrofatty infiltration in the myocardium. Magn Reson Med 61:215–221
de Vos AM, Prokop M, Roos CJ et al (2008) Peri-coronary epicardial adipose tissue is related to cardiovascular risk factors and coronary artery calcification in post-menopausal women. Eur Heart J 29:777–783
Ding J, Kritchevsky SB, Harris TB et al (2008) The association of pericardial fat with calcified coronary plaque. Obesity (Silver Spring) 16:1914–1919
Greif M, Becker A, von Ziegler F et al (2009) Pericardial adipose tissue determined by dual source CT is a risk factor for coronary atherosclerosis. Arterioscler Thromb Vasc Biol 29:781–786
Hubert HB, Feinleib M, McNamara PM et al (1983) Obesity as an independent risk factor for cardiovascular disease: a 26-year follow-up of participants in the Framingham Heart Study. Circulation 67:968–977
Walker SP, Rimm EB, Ascherio A et al (1996) Body size and fat distribution as predictors of stroke among US men. Am J Epidemiol 144:1143–1150
Burke AP, Farb A, Tashko G et al (1998) Arrhythmogenic right ventricular cardiomyopathy and fatty replacement of the right ventricular myocardium: are they different diseases? Circulation 97:1571–1580
Castillo E, Tandri H, Rodriguez ER et al (2004) Arrhythmogenic right ventricular dysplasia: ex vivo and in vivo fat detection with black-blood MR imaging. Radiology 232:38–48
Tandri H, Castillo E, Ferrari VA et al (2006) Magnetic resonance imaging of arrhythmogenic right ventricular dysplasia: sensitivity, specificity, and observer variability of fat detection versus functional analysis of the right ventricle. J Am Coll Cardiol 48:2277–2284
Tandri H, Macedo R, Calkins H et al (2008) Role of magnetic resonance imaging in arrhythmogenic right ventricular dysplasia: insights from the North American arrhythmogenic right ventricular dysplasia (ARVD/C) study. Am Heart J 155:147–153
Vermes E, Strohm O, Otmani A et al (2011) Impact of the revision of arrhythmogenic right ventricular cardiomyopathy/dysplasia task force criteria on its prevalence by CMR criteria. JACC Cardiovasc Imaging 4:282–287
Su L, Siegel JE, Fishbein MC (2004) Adipose tissue in myocardial infarction. Cardiovasc Pathol 13:98–102
Acknowledgments
The authors acknowledge financial support from: (1) the British Heart Foundation (RG/12/1/29262), (2) the Centre of Excellence in Medical Engineering funded by the Wellcome Trust and EPSRC (WT 088641/Z/09/Z), (3) the Department of Health via the National Institute for Health Research (NIHR) comprehensive Biomedical Research Centre award to Guy’s & St Thomas’ NHS Foundation Trust in partnership with King’s College London and King’s College Hospital NHS Foundation Trust, and (4) the National Institute for Health Research Leeds Clinical Research Facility. The views expressed are those of the authors and not necessarily those of the NHS, the NIHR, or the Department of Health.
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
Conflict of interest
There is no conflict of interest of any of the authors.
Ethical approval
All procedures performed in studies involving human participants were in accordance with the ethical standards of the institutional and/or national research committee and with the 1964 Helsinki declaration and its later amendments or comparable ethical standards.
Informed consent
Informed consent was obtained from all individual participants included in the study.
Rights and permissions
Open Access This article is distributed under the terms of the Creative Commons Attribution 4.0 International License (http://creativecommons.org/licenses/by/4.0/), which permits unrestricted use, distribution, and reproduction in any medium, provided you give appropriate credit to the original author(s) and the source, provide a link to the Creative Commons license, and indicate if changes were made.
About this article
Cite this article
Nezafat, M., Henningsson, M., Ripley, D.P. et al. Coronary MR angiography at 3T: fat suppression versus water-fat separation. Magn Reson Mater Phy 29, 733–738 (2016). https://doi.org/10.1007/s10334-016-0550-7
Received:
Revised:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s10334-016-0550-7