Abstract
Objective
This study aimed at assessing the evolution of cardiovascular characteristics during hemodialysis and ultrafiltration by a perturbation accurately defined in its magnitude and directly relevant to the problem of volume adjustment in stable hemodialysis patients.
Methods
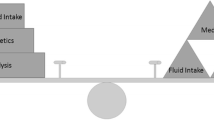
Excess fluid volume was removed by constant ultrafiltration-rate as prescribed. Hemodynamic variables were continuously measured throughout treatments using non-invasive finger plethysmography. In addition to ongoing volume reduction by ultrafiltration (long-term perturbation), well-defined magnitudes of intravascular volume were transiently and reversibly sequestered (short-term perturbation) into the extracorporeal circulation at hourly intervals. Sensitivities of hemodynamic variables and of the baroreflex to the acute change in intravascular volume (volume sensitivities) were analyzed.
Results
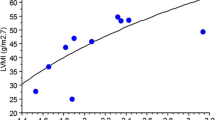
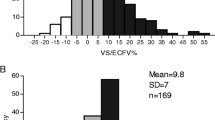
Eight stable patients were assessed during two subsequent treatments. Treatments were accompanied by a decrease in cardiac output (p < 0.05) and stroke volume (p < 0.01), and by an increase in peripheral resistance (p < 0.05) and diastolic pressure (p < 0.05). Mean arterial pressure remained unchanged for the whole group but correlated with the change in total peripheral resistance in individual treatments (p < 0.01). The average volume sensitivity of mean arterial pressure was 11.9 ± 9.9 mmHg/L and increased (p < 0.01) during treatments, while the average volume sensitivity of heart rate remained unchanged at −7.9 ± 8.58 1/(min L). The corresponding volume sensitivity of the baroreflex was −0.81 ± 1.5 1/(min mmHg) and remained unchanged for the whole group, but the change correlated with the change in mean arterial pressure in individual treatments (p < 0.05).
Interpretation
The changes in arterial pressures during hemodialysis appear to relate to an unbalanced response of barocontrol mechanisms characterized by a compromised chronotropy and vascular over-reactivity.




Similar content being viewed by others
References
Brummelhuis WJ, van Geest RJ, van Schelven LJ, Boer WH (2009) Sodium profiling, but not cool dialysate, increases the absolute plasma refill rate during hemodialysis. ASAIO J 55:575–580
Daugirdas JT (2001) Pathophysiology of dialysis hypotension: an update. Am J Kidney Dis 38:S11–S17
Shoji T, Tsubakihara Y, Fujii M, Imai E (2004) Hemodialysis-associated hypotension as an independent risk factor for two-year mortality in hemodialysis patients. Kidney Int 66:1212–1220
Locatelli F, Cavalli A, Tucci B (2010) The growing problem of intradialytic hypertension. Nat Rev Nephrol 6:41–48
Dorhout Mees EJ (2000) Cardiovascular aspects of dialysis treatment the importance of volume control. Kluwer, Dordrecht
Sagawa K (1983) Baroreflex control of systemic arterial pressure and vascular bed. In: Shepherd JT, Abboud FM (eds) The Cardiovascular System. American Physiological Society, Bethesda, pp 453–496
Karemaker JM (2002) Why do we measure baroreflex sensitivity the way we do? Clin Auton Res 12:427–428
Laude D, Elghozi J-L, Girard A, Bellard E, Bouhaddi M, Castiglioni P, Cerutti C, Cividjian A, Di Rienzo M, Fortrat J-O, Janssen B, Karemaker JM, Leftheriotis G, Parati G, Persson PB, Porta A, Quintin L, Regnard J, Rudiger H, Stauss HM (2004) Comparison of various techniques used to estimate spontaneous baroreflex sensitivity (the EuroBaVar study). Am J Physiol Regul Integr Comp Physiol 286:R226–R231
Chesterton LJ, Selby NM, Burton JO, Fialova J, Chan C, McIntyre CW (2010) Categorization of the hemodynamic response to hemodialysis: The importance of baroreflex sensitivity. Hemodial Int 14:18–28
Schneditz D, Kenner T, Heimel H, Stabinger H (1989) A sound speed sensor for the measurement of total protein concentration in disposable, blood perfused tubes. J Acoust Soc Am 86:2073–2080
Wimmer J, Bachler I, Haditsch B, Stadlbauer V, Holzer H, Schneditz D (2006) Device and technique for extracorporeal blood volume sequestration during hemodialysis. ASAIO J 52:662–669
Nadler SB, Hidalgo JU, Bloch T (1962) Predicition of blood volume in normal human adults. Surgery 51:224–232
Riley AA, Arakawa Y, Worley S, Duncan BW, Fukamachi K (2010) Circulating blood volumes: a review of measurement techniques and a meta-analysis in children. ASAIO J 56:260–264
Chen C-H, Lin Y-P, Yu W-C, Yang W-C, Ding Y-A (2003) Volume status and blood pressure during long-term hemodialysis: role of ventricular stiffness. Hypertension 42:257–262
Parati G, Di Rienzo M, Mancia G (2001) Dynamic modulation of baroreflex sensitivity in health and disease. Ann NY Acad Sci 940:469–487
Zhang R, Behbehani K, Crandall CG, Zuckerman JH, Levine BD (2001) Dynamic regulation of heart rate during acute hypotension: new insight into baroreflex function. Am J Physiol 280:H407–H419
Nette RW, Krepel HP, van den Dorpel MA, van den Meiracker AH, Poldermans D, Boomsma F, Weimar W, Zietse R (2003) Hemodynamic response to lower body negative pressure in hemodialysis patients. Am J Kidney Dis 41:807–813
Goswami N, Roessler A, Lackner H, Schneditz D, Grasser E, Hinghofer-Szalkay H (2009) Heart rate and stroke volume response patterns to augmented orthostatic stress. Clin Auton Res 19:157–165
Milnor WR (1990) Cardiovascular physiology. Oxford University Press, New York
Chesterton LJ, Sigrist MK, Bennett T, Taal MW, McIntyre CW (2005) Reduced baroreflex sensitivity is associated with increased vascular calcification and arterial stiffness. Nephrol Dial Transplant 20:1140–1147
Guerin AP, Pannier B, Marchais SJ, London GM (2008) Arterial structure and function in end-stage renal disease. Curr Hypertens Rep 10:107–111
McIntyre CW (2007) The functional cardiovascular consequences of vascular calcification. Semin Dial 20:122–128
James MA, Robinson TG, Potter JF (2001) The effect of systemic blood pressure on cardio-vascular reflexes in elderly subjects. Clin Physiol 21:67–76
Landry DW, Oliver JA (2006) Blood pressure instability during hemodialysis. Kidney Int 69:1710–1711
Seagard J, Gallenberg L, Hopp F, Dean C (1992) Acute resetting in two functionally different types of carotid baroreceptors. Circ Res 70:559–565
Smith SM, Potter JF, Samani NJ, Sammons EL, Rathbone WE, Bentley S, Panerai RB (2008) Are baroreflex events detected by invasive and non-invasive techniques coincident? Clin Physiol Funct I 28:262–269
Acknowledgments
This work was supported by a grant from Fresenius Medical Care Deutschland GmbH. The funds for the Finometer were provided by the infrastructure grant UGP4 of the Austrian Ministry of Science, Education, and Art. We thank Prof. H. Holzer and the dialysis staff for the opportunity and support to conduct this study at the Division of Nephrology and Hemodialysis, Department of Internal Medicine, at the Medical University of Graz. We also thank G. Vogrinec from our institute for final processing of the video resource accompanying this paper.
Conflict of interest
The authors declare that they have no conflict of interest.
Author information
Authors and Affiliations
Corresponding author
Electronic supplementary material
Below is the link to the electronic supplementary material.
Supplementary material 1 (MPG 49,716 kb)
Rights and permissions
About this article
Cite this article
Wimmer, J., Batzel, J.J., Haditsch, B. et al. Evolution of volume sensitivity during hemodialysis and ultrafiltration. Clin Auton Res 21, 353–360 (2011). https://doi.org/10.1007/s10286-011-0122-x
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s10286-011-0122-x