Abstract
Background
Volume overload is a known risk factor for cardiovascular complications in children on hemodialysis (HD), but a measurable index of volume overload is still lacking.
Methods
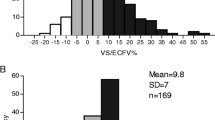
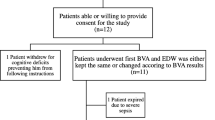
We propose a novel index of pre-HD volume overload based on blood volume (BV) monitoring, the first hour refill index (RI), calculated as the ratio between the ultrafiltration rate indexed for body weight during the first HD hour and the percent BV change at the first hour of the treatment. This parameter was retrospectively calculated in 121 sessions in 11 oligoanuric children and young adults on chronic HD, with median age 14.3 years (range 5.4–22.4), and its association with left-ventricular mass index, pre-HD blood pressure, and number of antihypertensive medications was evaluated.
Results
The median RI was 2.07 ml/kg/h/%. There was a significant correlation between RI and median LVMI (r 0.66, p = 0.028), which was 53.4 g/m2.7 (45.7–64) in patients with a median RI > 2, and 36.6 g/m2.7 (24.9–47) in those with a median RI < 2 ml/kg/h/% (p = 0.01). The number of antihypertensive drugs per patient was significantly higher in patients with a RI > 2 than in those with a RI < 2 ml/kg/h/% (three vs one per patient; p = 0.02) while blood pressure was not significantly different between the two groups.
Conclusions
The ratio between the ultrafiltration rate per body weight and the BV change during the first hour of a HD session could be a promising index of refill capacity and pre-HD volume overload in children and young adults on chronic HD.


Similar content being viewed by others
References
Groothoff JW, Gruppen MP, Offringa M, Hutten J, Lilien MR, Van De Kar NJ, Wolff ED, Davin JC, Heymans HS (2002) Mortality and causes of death of end-stage renal disease in children: a Dutch cohort study. Kidney Int 61:621–629
Chesnaye NC, Schaefer F, Groothoff JW, Bonthuis M, Reusz G, Heaf JG, Lewis M, Maurer E, Paripović D, Zagozdzon I, van Stralen KJ, Jager KJ (2016) Mortality risk in European children with end-stage renal disease on dialysis. Kidney Int 89:1355–1362
Paglialonga F, Consolo S, Galli MA, Testa S, Edefonti A (2015) Interdialytic weight gain in oligoanuric children and adolescents on chronic hemodialysis. Pediatr Nephrol 30:999–1005
Bakkaloglu SA, Borzych D, Soo Ha I, Serdaroglu E, Büscher R, Salas P, Patel H, Drozdz D, Vondrak K, Watanabe A, Villagra J, Yavascan O, Valenzuela M, Gipson D, Ng KH, Warady BA, Schaefer F, International Pediatric Peritoneal Dialysis Network (2011) Cardiac geometry in children receiving chronic peritoneal dialysis: findings from the International Pediatric Peritoneal Dialysis Network (IPPN) registry. Clin J Am Soc Nephrol 6:1926–1933
Mitsnefes MM, Daniels SR, Schwartz SM, Meyer RA, Khoury P, Strife CF (2000) Severe left ventricular hypertrophy in pediatric dialysis: prevalence and predictors. Pediatr Nephrol 14:898–902
Bakkaloglu SA, Saygily A, Sever L, Noyan A, Akman S, Ekim M, Aksu N, Doganay B, Yildiz N, Duzova A, Soylu A, Alpay H, Sonmez F, Civilibal M, Erdem S, Kardelen F (2009) Assessment of cardiovascular risk in paediatric peritoneal dialysis patients: a Turkish Pediatric Peritoneal Dialysis Study Group (TUPEPD) report. Nephrol Dial Transplant 24:3525–3532
Agarwal R, Bouldin JM, Light RP, Garg A (2011) Probing dry-weight improves left ventricular mass index. Am J Nephrol 33:373–380
Zaloszyc A, Schaefer B, Schaefer F, Krid S, Salomon R, Niaudet P, Schmitt CP, Fischbach M (2013) Hydration measurement by bioimpedance spectroscopy and blood pressure management in children on hemodialysis. Pediatr Nephrol 28:2169–2177
Milani GP, Groothoff JW, Vianello FA, Fossali EF, Paglialonga F, Edefonti A, Agostoni C, Consonni D, van Harskamp D, van Goudoever JB, Schierbeek H, Oosterveld MJ (2017) Bioimpedance and fluid status in children and adolescents treated with dialysis. Am J Kidney Dis 69:428–435
Allinovi M, Saleem M, Romagnani P, Nazerian P, Hayes W (2016) Lung ultrasound: a novel technique for detecting fluid overload in children on dialysis. Nephrol Dial Transplant 32:541–547
Allinovi M, Saleem MA, Burgess O, Armstrong C, Hayes W (2016) Finding covert fluid: methods for detecting volume overload in children on dialysis. Pediatr Nephrol 31:2327–2335
Dheu C, Terzic J, Menouer S, Fischbach M (2009) Importance of the curve shape for interpretation of blood volume monitor changes during haemodiafiltration. Pediatr Nephrol 24:1419–1423
Candan C, Sever L, Civilibal M, Caliskan S, Arisoy N (2009) Blood volume monitoring to adjust dry weight in hypertensive pediatric hemodialysis patients. Pediatr Nephrol 24:581–587
Patel HP, Goldstein SL, Mahan JD, Smith B, Fried CB, Currier H, Flynn JT (2007) A standard, noninvasive monitoring of hematocrit algorithm improves blood pressure control in pediatric hemodialysis patients. Clin J Am Soc Nephrol 2:252–257
Agarwal R, Kelley K, Light RP (2008) Diagnostic utility of blood volume monitoring in hemodialysis patients. Am J Kidney Dis 51:242–254
Maduell F, Arias M, Massó E, Fontseré N, Carrera M, Vera M, Cases A, Campistol JM (2013) Sensitivity of blood volume monitoring for fluid status assessment in hemodialysis patients. Blood Purif 35:202–208
Koomans HA, Geers AB, Mees EJ (1984) Plasma volume recovery after ultrafiltration in patients with chronic renal failure. Kidney Int 26:848–854
Wizemann V, Leibinger A, Mueller K, Nilson A (1995) Influence of hydration state on plasma volume changes during ultrafiltration. Artif Organs 19:416–419
Devereux RB, Alonso DR, Lutas EM, Gottlieb GJ, Campo E, Sachs I, Reichek N (1986) Echocardiographic assessment of left ventricular hypertrophy: comparison to necropsy findings. Am J Cardiol 57:450–458
Daniels SR, Kimball TR, Morrison JA, Khoury P, Meyers RA (1995) Indexing left ventricular mass to account for differences in body size in children and adolescents without cardiovascular disease. Am J Cardiol 76:699–701
Daugirdas JT (1993) Second generation logarithmic estimates of single-pool variable volume Kt/V: an analysis of error. J Am Soc Nephrol 4:1205–1213
Paglialonga F, Consolo S, Edefonti A, Montini G (2017) Blood pressure management in children on dialysis. Pediatr Nephrol. https://doi.org/10.1007/s00467-017-3666-8
Koc Y, Unsal A, Kayabasi H, Oztekin E, Sakaci T, Ahbap E, Yilmaz M, Akgun AO (2011) Impact of volume status on blood pressure and left ventricle structure in patients undergoing chronic hemodialysis. Ren Fail 33:377–381
Ozkahya M, Ok E, Toz H, Asci G, Duman S, Basci A, Kose T, Dorhout Mees EJ (2006) Long-term survival rates in haemodialysis patients treated with strict volume control. Nephrol Dial Transplant 21:3506–3513
VanDeVoorde RG, Barletta GM, Chand DH, Dresner IG, Lane J, Leiser J, Lin JJ, Pan CG, Patel H, Valentini RP, Mitsnefes MM (2007) Blood pressure control in pediatric hemodialysis: the Midwest Pediatric Nephrology Consortium tudy. Pediatr Nephrol 22:547–553
Haskin O, Wong CJ, McCabe L, Begin B, Sutherland SM, Chaudhuri A (2015) 44-h ambulatory blood pressure monitoring: revealing the true burden of hypertension in pediatric hemodialysis patients. Pediatr Nephrol 30:653–665
Kron S, Schneditz D, Leimbach T, Aign S, Kron J (2017) Vascular refilling is not reduced in dialysis sessions with morbid events. Blood Purif 43:309–314
Kron S, Schneditz D, Leimbach T, Aign S, Kron J (2016) Vascular refilling is independent of volume overload in hemodialysis with moderate ultrafiltration requirements. Hemodial Int 20:484–491
Pietribiasi M, Katzarski K, Galach M, Stachowska-Piętka J, Schneditz D, Lindholm B, Waniewski J (2015) Kinetics of plasma refilling during hemodialysis sessions with different initial fluid status. ASAIO J 61:350–356
Kron S, Wenkel R, Leimbach T, Aign S, Kron J (2016) Effects of osmotic changes on measuring relative blood volume: comparison of three hemodialysis devices. ASAIO J 62:214–215
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
The study was approved by the local Ethical Committee and conformed to the Declaration of Helsinki.
Conflict of interest
The authors declare that they have no conflict of interest.
Rights and permissions
About this article
Cite this article
Paglialonga, F., Consolo, S., Edefonti, A. et al. The first hour refill index: a promising marker of volume overload in children and young adults on chronic hemodialysis. Pediatr Nephrol 33, 1209–1214 (2018). https://doi.org/10.1007/s00467-018-3915-5
Received:
Revised:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s00467-018-3915-5