Abstract
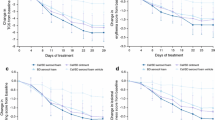
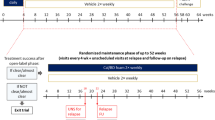
Background: Clobetasol propionate foam 0.05% (Connetics Corporation, Palo Alto, CA) is approved by the United States Food and Drug Administration for the treatment of corticosteroid-responsive scalp dermatoses, but there is only limited data available for its efficacy and tolerability in treating dermatoses which affect nonscalp sites. Objective: The efficacy and tolerability of clobetasol propionate foam (clobetasol foam) in treating psoriatic lesions at nonscalp sites was evaluated in a multicenter, randomized, double-blinded, placebo-controlled study of 279 patients with mild to moderate plaque-type psoriasis. Methods: The patients applied clobetasol foam or placebo to the psoriatic lesions twice daily for two weeks. In addition to receiving clinical evaluations, the study patients completed a questionnaire evaluating various characteristics of the foam formulation, including their preference for its use and their projected likelihood to comply with similar therapy in a nonstudy environment. Results: At Week 2 (or end of treatment), 68% (94/139) of patients who received clobetasol foam had a Physician’s Static Global Assessment score of 0 (clear, except for minor residual discoloration) or 1 (majority of lesions have individual scores for plaque thickness, erythema, and scaling that averages 1). This was significantly more than the 21% (30/140) observed in the placebo group (P < 0.0001). Similar results were obtained for the Patient’s Global Assessment score at Week 2 and in changes (from Baseline to Week 2) in the scores for the signs of psoriasis at a target lesion and for pruritus. Adverse effects were generally limited to mild and transient burning or other application site reactions in only a few patients in each treatment group. In the patient’s poststudy questionnaire (completed at Week 2, or end of treatment) a majority of patients rated the characteristics of the foam formulation very highly. The patients ranked the foam formulation as superior to other topical formulations based on factors impacting their quality of life and indicated they would be more likely to comply with a recommended course of therapy with the foam formulation than with other topical formulations. Conclusion: Clobetasol propionate foam 0.05% is safe and effective for the treatment of plaque-type psoriasis on scalp and nonscalp areas, when applied twice daily for two weeks. As it is understood that patient dissatisfaction with select topical formulations affects their compliance with therapy, which necessarily affects the effectiveness of the therapy, the results of the patient’s poststudy questionnaire suggest that there are multiple and integrated benefits for the use of clobetasol foam in the treatment of psoriasis of nonscalp sites.
Antécédents: La Food and Drug Administration, aux États-Unis, a approuvé l’usage de la mousse de propionate de clobétasol à 0,05% (Connetics Corporation, Palo Alto, California) dans le traitement des dermatoses du cuir chevelu qui sont sensibles aux corticostéroïdes. Cependant, les données sur son efficacité et le degré de tolérabilité dans le traitement d’autres dermatoses sont limitées. Objectifs: L’efficacité et la tolérabilité de la mousse de propionate de clobétasol (mosse clobétasol) dans le traitement des lésions de psoriasis qui ne sont pas localisées dans le cuir chevelu ont été évaluées dans une étude multicentrique, randomisée à double insu, contrôlée contre placebo, sur 279 patients souffrant de psoriasis doux à modéré. Méthodes: Pendant deux semaines, les patients appliquaient soit la mousse de clobétasol, soit le placebo, deux fois par jour sur les lésions de psoriasis. En plus de l’évaluation clinique, les patients ont rempli un questionnaire d’évaluation des différentes caractéristiques de la mousse, y compris leur préférence d’utilisation et jusqu’à quel point ils pensent pouvoir observer le traitement en-dehors de l’étude. Résultats: À la fin de la deuxiéme semaine (fin du traitement), 68% des patients (soit 94/139) qui ont reçu la mousse de clobétasol ont eu un score de 0 (guéri, sauf pour une décoloration résiduelle mineure) ou de 1 (la plupart des lésions présentent un score individuel moyen de 1 pour l’épaisseur, l’érythème et la desquamation). Ce pourcentage est bien supérieur aux 21% (30/140) du groupe placebo (P < 0,0001). Des résultats similaires ont été obtenus dans l’évaluation générale du patient à la deuxiéme semaine, ainsi que dans le changement du score (état de base/2 semaines) des signes du psoriasis et du prurit. Les effets indésirables se limitaient généralement à des brûlures faibles et passagères, ou à d’autres réactions sur le site de l’application chez seulement quelques patients dans chaque groupe. Dans le questionnaire que les patients ont rempli à la fin de l’etude, une majorité a donné une note élevée aux caractéristiques de la préparation en mousse. Les patients ont mieux classé cette préparation que les autres préparations topiques en ce qui concerne l’effet sur la qualité de vie et ont indiqué qu’ils seraient plus enclins à observer un traitement à la mousse qu’un traitement avec d’autres préparations topiques. Conclusion: L’efficacité et l’innocuité de la mousse de propionate de clobétasol à 0,05 % sont prouvées dans le traitement du psoriasis en plaques, touchant ou non le cuir chevelu, lorsque la préparation est appliquée deux fois par jour pendant deux semaines. Sachant que le mécontentement des patients envers une préparation topique donnée affecte l’observation du traitement, qui nuit par le fait même à l’efficacité du médicament, les résultats du questionnaire suggèrent que les avantages de l’utilisation de la mousse de clobétasol dans le traitement du psoriasis qui n’affecte pas le cuir chevelu sont multiples.




Similar content being viewed by others
References
G Krueger J Koo M Lebwohl et al. (2001) ArticleTitleThe impact of psoriasis on quality of life. Arch Dermatol 137 280–284 Occurrence Handle1:STN:280:DC%2BD3M7pvV2jsw%3D%3D Occurrence Handle11255325
JJ Miller D Roling D Margolis et al. (1999) ArticleTitleFailure to demonstrate therapeutic tachyphylaxis to topically applied steroids in patients with psoriasis. J Am Acad Dermatol 41 546–549 Occurrence Handle1:STN:280:DyaK1Mvis1yquw%3D%3D Occurrence Handle10495373
TJ Franz DA Parsell JA Myers et al. (2000) ArticleTitleClobetasol propionate foam 0.05%: a novel vehicle with enhanced delivery. Int J Dermatol 39 535–539 Occurrence Handle10.1046/j.1365-4362.2000.00986-4.x Occurrence Handle1:STN:280:DC%2BD3cvpsFOhsw%3D%3D Occurrence Handle10940121
AB Gottlieb (1998) ArticleTitlePsoriasis. Dis Manag Clin Outcomes 1 195–202 Occurrence Handle10.1016/S1088-3371(98)00025-4
InstitutionalAuthorNameConnectics Crop. (2000) Clobetasol propionate (foam) prescribing information. Connetics Corporation Palo Alto, CA
EO Gilbertson MC Spellman DJ Piacquadio et al. (1998) ArticleTitleSuper potent topical corticosteroid use associated with adrenal suppression: clinical considerations. J Am Acad Dermatol 38 318–321 Occurrence Handle1:STN:280:DyaK1c7ks1Wisw%3D%3D Occurrence Handle9486706
HI Katz JS Lindholm JS Weiss et al. (1995) ArticleTitleEfficacy and safety of twice-daily augmented betamethasone dipropionate lotion versus clobetasol propionate solution in patients with moderate to severe scalp psoriasis. Clin Ther 17 390–401 Occurrence Handle10.1016/0149-2918(95)80104-9 Occurrence Handle1:STN:280:BymD2s%2FjsVw%3D Occurrence Handle7585843
EA Olsen DL Cram CN Ellis et al. (1991) ArticleTitleA double-blind, vehicle-controlled study of clobetasol propionate, 0.05% (Temovate) scalp application in the treatment of moderate to severe scalp psoriasis. J Am Acad Dermatol 24 443–447 Occurrence Handle1:STN:280:By6B1cnks1Q%3D Occurrence Handle2061442
D Lubach J Rath M Kietzmann (1995) ArticleTitleSkin atrophy induced by initial continuous topical application of clobetasol followed by intermittent application. Dermatology 190 51–55 Occurrence Handle1:STN:280:ByqB3c7jsVE%3D Occurrence Handle7894098
InstitutionalAuthorNameGalxo Welcome (2000) Clobetasol propionate (ointment) prescribing information. Glaxo Wellcome Middlesex
InstitutionalAuthorNameGalxo Welcome (2000) Clobetasol propionate (scalp application) prescribing information. Glaxo Wellcome Middlesex
J Koo M Lebwohl (1999) ArticleTitleDuration of remission of psoriasis therapies. J Am Acad Dermatol 41 51–59 Occurrence Handle1:STN:280:DyaK1Mzjslaiug%3D%3D Occurrence Handle10411411
LF Stein A Sherr G Solodkina et al. (2001) ArticleTitleBetamethasone valerate foam for the treatment of nonscalp psoriasis. J Cut Med Surg 4 303–307
SL Gottlieb P Gilleaudeau R Johnson et al. (1995) ArticleTitleResponse of psoriasis to lymphocyte-selective toxin (DAB389IL-2) suggests a primary immune but not keratinocyte pathogenic basis. Nat Med 1 442–447 Occurrence Handle1:CAS:528:DyaK2MXls1SgtLw%3D Occurrence Handle7585092
HL Richards DG Fortune TM O’Sullivan et al. (1999) ArticleTitlePatients with psoriasis and their compliance with medication. J Am Acad Dermatol 41 581–583 Occurrence Handle1:STN:280:DyaK1Mvis12jtA%3D%3D Occurrence Handle10495380
CH Endzweig M Lebwohl (2001) ArticleTitleOlux foam as a cosmetically appearing delivery system for the treatment of psoriasis. Cosm Dermatol 14 13–15
Acknowledgements
Clinical investigators for this study were the following: Harold F. Farber, MD, Philadelphia, PA; Virginia C. Fiedler, MD, Chicago, IL; Michael H. Gold, MD, Nashville, TN; Alice B. Gottlieb, MD, PhD, New Brunswick, NJ; Gerald G. Krueger, MD, Salt Lake City, UT; Mark G. Lebwohl, MD, New York, NY; Alan Menter, MD, Dallas, TX; Bruce H. Miller, MD, Portland, OR; Toivo E. Rist, MD, Knoxville, TN; Thomas J. Russell, MD, Milwaukee, Wl; Ronald C. Savin, MD, New Haven, CT; Stacy R. Smith, MD, La Jolla, CA; Jeffrey M. Sobell, MD, North Andover, MA; Patricia N. Speelman, MD, Vista, CA; Linda F. Stein, MD, Detroit, MI; Kenneth J. Washenik, MD, PhD, New York, NY.
Author information
Authors and Affiliations
Corresponding author
About this article
Cite this article
Gottlieb, A.B., Ford, R. & Spellman, M.C. The Efficacy and Tolerability of Clobetasol Propionate Foam 0.05% in the Treatment of Mild to Moderate Plaque-type Psoriasis of Nonscalp Regions . JCMS 7, 185–192 (2003). https://doi.org/10.1007/s10227-002-0114-5
Published:
Issue Date:
DOI: https://doi.org/10.1007/s10227-002-0114-5