Abstract
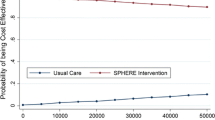
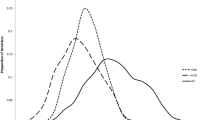
Heterogeneity exists within the patient population with coronary heart disease and the cost effectiveness of treatment may vary across subgroups within the overall population. This study compares the cost effectiveness of a secondary prevention intervention for a combined patient population relative to three selected subgroups: patients aged over 70 years; patients with a diagnosis other than angina only (that is, patients with a history of myocardial infarction, coronary artery bypass graft and/or percutaneous transluminal coronary angioplasty); and patients with diabetes. The results for the general population have been published elsewhere, but ongoing budget constraints require consideration of the appropriateness of targeting resources to patient subgroups. We adopt a probabilistic model to combine within trial and beyond trial impacts of treatment to estimate the lifetime health care costs and quality-adjusted life years of two primary care-based secondary prevention strategies: SPHERE Intervention—tailored practice and patient care plans and Control—standardised usual care. In all cases, the intervention was associated with mean cost savings and mean QALYs gains, when compared to the control, though statistical significance was never achieved. However, the probability of the intervention being cost effective was higher than 85% in all analyses across a range of potential cost-effectiveness threshold values. There is no compelling statistical evidence to support the targeting of specific subgroups across the general population. However, if affordability constraints are binding, the results do allow a tentative ranking of priorities based on the probabilistic subgroup analysis.


Similar content being viewed by others
References
Clark, A.M., Hartling, L., Vandermeer, B., McAlister, F.A.: Meta-analysis: secondary prevention programs for patients with coronary artery disease. Ann. Intern. Med. 143(9), 659–672 (2005)
Drummond, M.F., Sculpher, M.J., Torrance, G.W., O’Brien, J., Stoddart, G.L.: Methods for the Economic Evaluation of Health Care Programmes. Oxford University Press, Oxford (2005)
Sun, X., Faunce, T.: Decision-analytical modelling in health-care economic evaluations. Eur. J. Health Econ. 9, 313–323 (2008)
Taylor, D.C.A., Pandya, A., Thompson, D., Chu, P., Graff, J., Shepherd, J., Wenger, N., Greten, H., Carmena, R., Drummond, M.F., Weinstein, M.C.: Cost-effectiveness of intensive atorvastatin therapy in secondary cardiovascular prevention in the United Kingdom, Spain, and Germany, based on the treating to new targets study. Eur. J. Health Econ. 10, 255–265 (2009)
Gillespie, P., O’Shea, E., Murphy, A.W., Smith, S.M., Byrne, M.C., Byrne, M., Cupples, M.E.: The cost effectiveness of the SPHERE intervention for the secondary prevention of coronary heart disease. Int. J. Technol. Assess. Health Care. 26(3), 263–271 (2010)
Murphy, A.W., Cupples, M.E., Smith, S., Byrne, M., Byrne, M.C., Newell, J.: Secondary prevention of heart disease in general practice: a cluster randomised controlled trial of tailored practice and patient care plans. Br. Med. J. 339, b4220 (2009). doi:10.1136/bmj.b4220
Murphy, A.W., Cupples, M.E., Smith, S., Byrne, M., Leathem, C., Byrne, M.C.: The SPHERE Study. Secondary prevention of heart disease in general practice: protocol of a randomised controlled trial of tailored practice and patient care plans with parallel qualitative, economic and policy analyses. [ISRCTN24081411]. Curr. Control Trials Cardiovasc. Med. 6, 11 (2005)
Fenwick, E., Byford, S.: A guide to cost effectiveness acceptability curves. Br. J. Psychiatr. 187, 106–108 (2005)
D’Agostino, R.B., Russell, M., Huse, D.M., Ellison, R.C., Silbershatz, H., Wilson, P.W., Hartz, S.C.: Primary and subsequent coronary risk appraisal: new results from The Framingham Study. Am. Heart J. 139, 272–281 (2000)
Barry, M., Tilson, L.: Recent developments in pricing and reimbursement of medicines in Ireland. Expert Rev. Pharmacoeconomics Outcomes Res. 7, 605–611 (2007)
National Institute for Clinical Excellence: Guide to the methods of technology appraisal. London: NICE, Apr 2004. www.nice.org.uk/page.aspx?o=201974 (reference 0515)
Ware, J.E., Kosinski, M., Keller, S.D.: A 12-item short-form health survey: construction of scales and preliminary tests of reliability and validity. Med. Care 34(3), 220–233 (1996)
Brazier, J.E., Roberts, J.: Estimating a preference-based index from the SF-12. Med. Care 42(9), 851–859 (2004)
Campbell, M.K., Elbourne, D.R., Altman, D.G.: CONSORT statement: extension to cluster randomised trials. BMJ 328, 702–708 (2004)
Central Statistics Office: Dublin (www.cso.ie)
Department of Health and Children: The National Heartwatch Programme: Clinical Report—March 2003 to December 2005. Dublin. (2006)
Robinson, M., Palmer, S., Sculpher, M., Philips, Z., Ginnelly, L., Bowens, A., Golder, S., Alfakih, K., Bakhai, A., Packham, C., Cooper, N., Abrams, K., Eastwood, A., Pearman, A., Flather, M., Gray, D., Hall, A.: Cost effectiveness of alternative strategies for the initial medical management of non-ST elevation acute coronary syndrome: systematic review and decision-analytical modelling. Health Technol. Assess. 9(27), 1–172 (2005)
Hardin, J.W., Hilbe, J.M.: Generalised estimating equations. Chapman and Hall/CRC Press, London (2003)
Glick, H.A., Doshi, J.A., Sonnad, S.S., Polsky, D.: Economic evaluation in clinical trials. Oxford University Press, Oxford (2007)
Thompson, S.G., Nixon, R.M., Grieve, R.: Addressing the issues that arise in analysing multicentre cost data with application to a multinational study. J Health Econ. 25, 1015–1028 (2006)
Netten, A., Curtis, J.: Unit costs of health and social care. Personal Social Services Research Unit, University of Kent, Canterbury (2006)
Central Bank of Ireland: Dublin (www.centralbank.ie)
Manca, A., Hawkins, N., Sculpher, M.: Estimating mean QALYs in trial based cost effectiveness analysis: the importance of controlling for baseline utility. Health Econ. 14, 487–496 (2005)
Lacey, E.A., Walters, S.J.: Continuing inequality: gender and social class influences on self perceived health after a heart attack. J. Epidemiol. Commun. Health 57, 622–627 (2003)
Davies, A., Hutton, J., o’Donnell, J., Kingslake, S.: Cost effectiveness of rosuvastatin, atorvastatin, simvastatin, pravastatin and fluvastatin for the primary prevention of CHD in the UK. Br. J. Cardiol. 13, 196–202 (2006)
Briggs, A., Claxton, K., Sculpher, M.: Decision modelling for health economic evaluation. Oxford University Press, Oxford (2005)
Black, W.C.: The cost effectiveness plane: a graphic representation of cost effectiveness. Med. Decis. Making 10, 212–215 (1990)
Johnston, K., Gray, A., Moher, M., Yudkin, P., Wright, L., Mant, D.: Reporting the cost-effectiveness of interventions with nonsignificant effect differences: example from a trial of secondary prevention of heart disease. Int. J. Technol. Assess. Health Care 19(3), 476–489 (2003)
Buckley, B.S., Simpson, C.R., McLernon, D.J., Murphy, A.W., Hannaford, P.C.: Five year prognosis in patients with angina identified in primary care: incident cohort study. BMJ 339, b3058 (2009)
Briggs, A.: A Bayesian approach to stochastic cost effectiveness analysis: an illustration and application to blood pressure control in type 2 diabetes. Int. J. Technol. Assess. Health Care 17(1), 69–82 (2001)
O’Neill, C., Normand, C., Cupples, M., McKnight, A.: Cost effectiveness of personal health education in primary care for people with angina in the Greater Belfast area of Northern Ireland. J. Epidemiol. Commun. Health 50, 538–540 (1996)
Raftery, J.P., Yao, G.L., Murchie, P., Campbell, N.C., Ritchie, L.D.: Cost effectiveness of nurse led secondary prevention clinics for coronary heart disease in primary care: follow up of a randomised controlled trial. BMJ 330(7493), 707 (2005)
Turner, D.A., Paul, S.K., Stone, M., Juarez-Garcia, A., Squire, I., Khunti, K.: Cost-effectiveness of a disease management programme for secondary prevention of coronary heart disease and heart failure in primary care. Heart 94, 1601–1606 (2008)
Acknowledgments
We would like to thank the other members of the SPHERE study team including C. Leathem, A. Houlihan, M. O.’Malley, V. Spillane, H. Grealish and P. Ryan (research nurses); M. Corrigan, M. D’Eath and J. Wilson (qualitative researchers); and A. Kelly, J. Newell and M. Donnelly (statistical and policy advisers). We would also like to thank the patients and practitioners who participated in the study. This study was funded by the Health Research Board and Irish Heart Foundation. The funders had no part in the design of the study; the collection, analysis and interpretation of the data; the writing of the report; and the decision to submit the article for publication.
Author information
Authors and Affiliations
Consortia
Corresponding author
Appendix: model input parameter data
Rights and permissions
About this article
Cite this article
Gillespie, P., O’Shea, E., Murphy, A.W. et al. Relative cost effectiveness of the SPHERE intervention in selected patient subgroups with existing coronary heart disease. Eur J Health Econ 13, 429–443 (2012). https://doi.org/10.1007/s10198-011-0314-2
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s10198-011-0314-2
Keywords
- Coronary heart disease
- Secondary prevention
- General practice
- Cost effectiveness analysis: subgroup analysis