Abstract
Background
This study aims to describe the regional variance in prescriptions for chronic kidney disease (CKD) medications and to analyze regional characteristics to identify the sources of these differences by utilizing the National Database of Health Insurance Claims, which provides more than 95% of nationwide claim information for Japan.
Methods
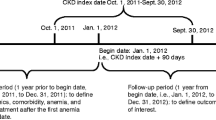
Data regarding the total claimed amount for phosphate binders (PBs), erythropoiesis-stimulating agents (ESAs), carbonaceous adsorbents, and potassium-lowering agents in fiscal year 2015 were obtained. Correlation coefficients were calculated for the claimed amount of these drugs per CKD patient and social and medical variables, including the percentage of the population aged ≥ 65 years and the numbers of hospital beds and certified nephrologists. Subsequent multiple regression analysis was performed using explanatory factors affecting the amount of PB or ESA prescriptions per CKD patient.
Results
The total claimed amounts were 585,485,115 for PBs and 2,373,777 for ESAs. Variations in the claimed amount per CKD patient among 47 prefectures were 4.9-, 6.1-, 6.6-, and 6.0-fold for PBs, ESAs, carbonaceous adsorbents and potassium-lowering agents, respectively. The number of nephrologists per CKD patient was positively correlated with the prescribed amount for PBs and ESAs per CKD patient, and independently associated with the prescribed amount also in regression analysis.
Conclusion
Substantial regional variation in CKD-related drug prescriptions exists even within a uniform health care system. The number of certified nephrologists was associated with the prescribed amount for PBs and ESAs. Further studies are needed to clarify whether geographic distribution of certified nephrologist may affect clinical practice pattern.


Similar content being viewed by others
References
Ikegami N, Yoo BK, Hashimoto H, Matsumoto M, Ogata H, Babazono A, et al. Japanese universal health coverage: evolution, achievements, and challenges. Lancet. 2011;378:1106–15.
Ishikawa KB. Medical big data for research use: current status and related issues. Japan Med Assoc J. 2016;59:110–24.
Mues KE, Liede A, Liu J, Wetmore JB, Zaha R, Bradbury BD, et al. Use of the Medicare database in epidemiologic and health services research: a valuable source of real-world evidence on the older and disabled populations in the US. Clin Epidemiol. 2017;9:267–77.
Yamasaki D, Tanabe M, Muraki Y, Kato G, Ohmagari N, Yagi T. The first report of Japanese antimicrobial use measured by national database based on health insurance claims data (2011–2013): comparison with sales data, and trend analysis stratified by antimicrobial category and age group. Infection. 2018;46:207–14.
Okumura Y, Sugiyama N, Noda T, Tachimori H. Psychiatric admissions and length of stay during fiscal years 2014 and 2015 in Japan: a retrospective cohort study using a nationwide claims database. J Epidemiol. 2018. https://doi.org/10.2188/jea.JE20180096.
Kamata Y, Minota S. Wide difference in biologics usage and expenditure for the treatment of patients with rheumatoid arthritis in each prefecture in Japan analyzed using “National Database of Health Insurance Claims and Specific Health Checkups of Japan”. Rheumatol Int. 2018;38:663–68.
Jardine MJ, Kasiske B, Adu D, Alrukhaimi M, Ashuntantang GE, Basnet S. Closing the gap between evidence and practice in chronic kidney disease. Kidney Int Suppl. 2017;7:114–21.
Masakane I, Taniguchi M, Nakai S, Tsuchida K, Goto S, Wada A, et al. Annual dialysis data report 2015, JSDT renal data registry. Ren Replace Ther. 2018; 4:19.
Chihara D, Ito H, Katanoda K, Shibata A, Matsuda T, Sobue T, et al. Incidence of myelodysplastic syndrome in Japan. J Epidemiol. 2014;24:469–73.
Naito T, Ohtani H, Kobayashi K, Miyazaki M, Yamada K, Sugawara M. Current status of and regional differences in CKD management and medical cooperation in Japan: from the results of a nationwide questionnaire survey for primary care physicians [in Japanese]. Nihon Jinzo Gakkai Shi. 2013;55:1391–400.
Nakamura S, Nakata H, Yoshihara F, Kamide K, Horio T, Nakahama H, et al. Effect of early nephrology referral on the initiation of hemodialysis and survival in patients with chronic kidney disease and cardiovascular diseases. Circ J. 2007;71:511–6.
Winkelmayer WC, Owen WF Jr, Levin R, Avorn J. A propensity analysis of late versus early nephrologist referral and mortality on dialysis. J Am Soc Nephrol. 2003;14:486–92.
Kim DH, Kim M, Kim H, Kim YL, Kang SW, Yang CW, et al. Early referral to a nephrologist improved patient survival: prospective cohort study for end-stage renal disease in Korea. PLoS One. 2013;8:e55323.
Fischer MJ, Stroupe KT, Kaufman JS, O’Hare AM, Browning MM, Sohn MW, et al. Predialysis nephrology care and dialysis-related health outcomes among older adults initiating dialysis. BMC Nephrol. 2016;17:103.
Baek SH, Ahn S, Lee SW, Park YS, Kim S, Na KY, et al. Outcomes of predialysis nephrology care in elderly patients beginning to undergo dialysis. PLoS One. 2015;10:e0128715.
Japanese Society of Nephrology. Essential points from evidence-based Clinical Practice Guidelines for Chronic Kidney Disease 2018. Clin Exp Nephrol. 2019;23:1–15.
Furumatsu Y, Nagasawa Y, Hamano T, Iwatani H, Iio K, Shoji T, et al. Integrated therapies including erythropoietin decrease the incidence of dialysis: lessons from mapping the incidence of end-stage renal disease in Japan. Nephrol Dial Transplant. 2008;23:984–90.
Imasawa T, Nakazato T. Status of board-certified nephrologists of the Japanese Society of Nephrology among 47 prefectures [in Japanese]. Nihon Jinzo Gakkai Shi. 2010;52:1015–21.
White H, Gillgrass L, Wood A, Peckham DG. Requirements and access needs of patients with chronic disease to their hospital electronic health record: results of a cross-sectional questionnaire survey. BMJ Open. 2016;6:e012257.
Tsutsumi M, Shaku F, Ozone S, Sakamoto N, Maeno T. Reasons for the preference of clinic visits to self-medication by common cold patients in Japan. J Gen Fam Med. 2017;18:336–40.
Acknowledgements
This work was supported by the Kidney Foundation Grant for Pathophysiological Research Conferences in Chronic Kidney Disease (JKFB17-9, to HN).
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
Conflict of interest
All the authors have declared no competing interest.
Human and animal rights
The study was approved by the University of Tokyo Graduate School of Medicine Research Ethics Committee (#11621).
Additional information
Publisher’s Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
About this article
Cite this article
Inoue, R., Nishi, H., Tanaka, T. et al. Regional variance in patterns of prescriptions for chronic kidney disease in Japan. Clin Exp Nephrol 23, 859–864 (2019). https://doi.org/10.1007/s10157-019-01720-x
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s10157-019-01720-x