Abstract
Background
Patients with chronic kidney disease (CKD) are at high risk of drug-related problems (DRPs) because of extensive comorbidities and pharmacokinetic changes. This study aimed to identify DRPs and possible contributing factors in hospitalized patients with CKD, and evaluate the efficacy of the clinical pharmacist services in detection and intervention of DRPs in a large general hospital in Zhejiang Province, eastern China.
Methods
With the approval of the Ethics Committee, patients with CKD admitted to the nephrology ward from January to December 2020 were enrolled in this prospective study. The clinical pharmacist identified and intervened the DRPs during hospitalization. The DRPs were classified using the Pharmaceutical Care Network Europe (PCNE) DRP classification system, and all data were statistically analyzed using Statistical Package for Social Science (SPSS) version 26.0.
Results
A total of 914 patients with CKD were included, with 463 DRPs observed among 420 (45.95%) participants; the average DRP per patient was 0.51 (standard deviation [SD], 0.60) before pharmacist intervention. Treatment safety accounted for the highest proportion of problems (43.84%), followed by treatment efficacy, accounting for 43.20%. Drug selection was the most common cause of DRPs (60.26%), and antibiotics and cardiovascular agents were the most common drugs associated with DRPs (32.84% and 28.66%, respectively). A total of 85.53% of pharmaceutical intervention recommendations were followed, and 84.23% of DRPs were completely resolved after intervention by the clinical pharmacist. The proportion of patients who experienced DRPs decreased to 7.77%, with an average of 0.08 (SD 0.28) DRPs during hospitalization after pharmacist’s intervention. Significant contributing factors for DRPs were CKD stage 4, number of comorbid diseases, number of prescribed medications, and hospitalization days in both the univariate and multivariate logistic regression models.
Conclusion
DRPs are common among hospitalized patients with CKD in China. CKD stage 4, the number of comorbidities, use of multiple prescription drugs, and extended length of hospital stay are contributing factors for DRPs. Even only one clinical nephrology pharmacist in the nephrology ward, clinical pharmacist can play an important role in facilitating the identification of DRPs in patients with CKD and assisting physicians resolve DRPs in this single center study in China.
Similar content being viewed by others
Background
In 2017, the global prevalence of chronic kidney disease (CKD) was estimated to be 9.1%, with 697.5 million cases of all-stage CKD recorded [1]. China accounted for 132.3 million among these cases with the incidence was 9.57% [1]. A 2014 cross-sectional study estimated the prevalence of CKD at 9.88% (approximately 5.67 million patients) in Zhejiang Province, eastern China [2]. According to the 2015 Annual Data Report of the China Kidney Disease Network (CK-NET), more than half of patients with CKD in China were aged ≥ 60 years, and the most common causes of CKD include diabetic kidney disease, hypertensive nephropathy, obstructive nephropathy and glomerulonephritis [3].
According to the Pharmaceutical Care Network Europe (PCNE), drug-related problems (DRPs), including unnecessary drug therapy, ineffective drugs, need for additional drug therapy, and inappropriate drug dose or frequency, can certainly or potentially affect the desired therapeutic outcomes [4,5,6]. A systematic review in 2020 based on 16 studies reported that the average number of DRPs per patient ranged from 0.58 to 7.2 [7]. A large population-based retrospective study found 25% of patients with CKD had three or more comorbidities, with hypertension, diabetes, heart failure, chronic pulmonary disease and atrial fibrillation being the five most common comorbidities [8]. The use of multiple drugs is necessary in CKD population with comorbidities, but also obviously increase the risk of DRPs [5, 9,10,11]. Besides, CKD seriously alters the pharmacokinetic parameters of drugs mainly metabolized and excreted by kidney [10, 12]. Some antibiotics, such as vancomycin, need to adjust the dose or frequency according to kidney function in CKD population. The dose-adjustment regimens might be more complex, especially in the CKD cases with renal replacement therapy [12, 13]. Briefly, due to extensive comorbidities and pharmacokinetic changes, the patients with CKD are at high risk of DRPs [5, 14]. A systematic review based on 20 studies showed that the prevalence of DRPs in cases of CKD ranged from 12–87% [14].
Since DRPs are highly prevalent in patients with CKD, it is necessary to discover and address DRPs in time. The valuable contribution of pharmacists to drug therapy in patients with CKD, including drug dosage adjustment, adverse reaction detection, blood concentration monitoring, and medication-related education, has been documented in two systematic reviews [15, 16]. It can be predicted that with pharmacist identification and intervention of DRPs, the drug use in patients with CKD will be more reasonable and clinical outcomes will be greatly improved [16,17,18,19,20,21]. In a 2-year randomized, controlled study, compared with patients receiving the standard of care, those receiving pharmaceutical care had significantly fewer all-cause hospitalizations and shorter lengths of stay; 530 DRPs were simultaneously identified and resolved [22]. In a randomized controlled trial including 100 patients with CKD, the number of DRPs per patient at discharge was significantly affected by clinical pharmacists, and was 0.94 ± 1.03 and 1.96 ± 1.25 in the intervention and control groups respectively (p < 0.001) [20].In the Zhejiang Province, there are approximately 5.67 million CKD patients and only approximately 15 nephrology pharmacists [2]. It is common for many public hospitals in Zhejiang Province, even in China, to have only one clinical nephrology pharmacist, under the background of relatively insufficient number of clinical nephrology pharmacists. So far, the characteristics of DRP in Chinese patients with CKD has not been described in the literature. The aim of the present study was to identify DRPs and possible determinants in hospitalized patients with CKD, and evaluate the efficacy of the clinical pharmacist services in detection and intervention of DRPs in a nephrology ward of a large general hospital in Zhejiang Province, eastern China.
Methods
Study design and setting
This prospective study was approved by Ethics Committee of Zhejiang Provincial People’s Hospital. Hospitalized patients admitted in the nephrology department (60 beds) with diagnoses including CKD from January to December 2020, were included in this study after providing informed consent. A professional clinical nephrology pharmacist, who had 10 years of experience in the management of nephropathy medication, identified DRPs and provided pharmaceutical recommendations to the doctors, nurses and patients. DRPs were identified by this pharmacist by evaluating the appropriateness of drug therapy in terms of indication, dosage, safety, efficacy and cost. Standard guidelines published by authoritative nephrology organization, such as Kidney Disease: Improving Global Outcomes (KDIGO) association, and drug instructions were the main references for determining DRPs. The clinical pharmacist evaluated and addressed DRPs by attending clinical ward rounds with doctors from Monday to Friday, reviewing doctors’ orders daily in the hospital information system (HIS), and providing medication-related education (MRE) for discharged patients from Monday to Friday. At each clinical round, the pharmacist preformed three main tasks: ① Medication reconciliation (MR) aiming to reduce medication discrepancies in the dose or frequency of all medications given within 24 h after admission to the nephrology ward compared with those before admission, in addition to adjustment of anticoagulant or antiplatelet medication for patients requiring renal biopsy. ② Medication evaluation and management (MEM) mainly involving reviews of the route of administration, dosage and incompatibility for new orders by the pharmacist. ③ MRE for discharged patients aiming to improve patient compliance and medical knowledge using educational materials. MRE included best usage of drugs, special drug storage conditions, common adverse effects of drugs, and food and drugs contraindications. When necessary, pharmacist interviewed patients to determine the occurrence of a DRP. The identified DRPs were categorized using PCNE classification tool, version 9.00, and briefly classified by problem (P), cause (C), intervention (I), acceptance (A), and outcome (O) [6].
When a DRP occurred, the clinical pharmacist recorded it, consulted relevant guidelines/drug instructions, and communicated with the clinicians or patients. There were many ways to consult with doctors, including face-to-face discussions, telephone communication, and the use of communication software (WeChat or Ding Talk software). Communication with patients with CKD about DRPs was generally confined to bedside communication. A DRP was considered completely resolved when the clinician followed the pharmacist’s recommendation and made changes to the prescribed medication accordingly before a consequence caused by this DRP during hospitalization. A DRP was considered unresolved if the physician did not follow or implement the pharmacist’s recommendations for prescription modification during hospitalization. If the pharmacist’s recommendation regarding a DRP was not accepted or implemented, the clinical pharmacist recorded any related effects, and carefully monitored changes in laboratory indicators and consequences induced by this DRP during the remainder of the hospital stay. Due to the inclusion of only one clinical pharmacist in this study, all pharmacist interventions and follow-ups were limited to the hospitalization during which the DRP occurred.
Data collection
All patient data, including sociodemographic characteristics (age, sex, smoking status, and alcohol consumption status), and clinical information (number of complications, number of drugs prescribed, and length of stay), were collected and recorded. All the abovementioned data were queried and extracted from the HIS. The sociodemographic data of all new inpatients with CKD were collected by a graduate student at 9:00 a.m. daily, whereas the clinical data were collected by the pharmacist every week. If certain information was missing in the HIS, the clinical pharmacist inquired about the information.
Statistical analysis
Categorical variables were expressed as frequencies and percentages, and continuous variables were expressed as means and standard deviations (SDs). The Wilcoxon signed ranks test was used to analyze the changes in DRP quantity before and after the clinical pharmacist’s intervention in CKD patients as the distribution of DRPs in the sample did not conform to a Gaussian distribution. Logistic regression analysis was performed to determine potential determinants of DRPs. The results were reported as odds ratios (ORs) with 95% confidence intervals (CIs). Crude ORs were obtained using logistic regression for a single independent variable. Accordingly, only significant independent variables were analyzed using logistic regression to adjust the OR. The Statistical Package for Social Science (SPSS) (version 26.0) was used for data analysis, and a p value < 0.05 was considered statistically significant.
Results
Patient characteristics
A total of 914 patients were included, with a mean age of 60.23 ± 17.83 years. 38.29% were men, and 64.44% of patients were diagnosed with stage 5 CKD in this study. The median numbers of comorbid diseases were 3.12 ± 1.31, with hypertension (74.84%) and diabetes mellitus (34.79%) being the most common kinds. The average hospital stay of each patient was nearly 1 week (8.76 ± 4.54 days), and 14.74 ± 8.60 drugs were prescribed (Table 1).
Prevalence of DRPs
During the study period, 463 DRPs were recorded in 420 (45.95%) study participants, and the number of DRPs per patient was 0.51 (SD 0.60). Further analysis showed that 385 patients experienced 1 DRP, 27 patients experienced 2 DRPs, and 8 patients experienced 3 DRPs before the clinical pharmacist’s intervention during hospitalization.
Classification of DRPs
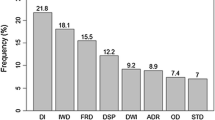
According to the PCNE classification tool version 9.00, treatment safety accounted for the highest proportion of problems (43.84%), followed by treatment efficacy (43.20%). Drug selection was the most common cause of DRPs (60.26%), followed by dose (29.59%) (Table 2). Unreasonable use of antibiotics and cardiovascular agents were the most common cause of DRPs (32.84% and 28.66%, respectively) (Fig. 1).
Clinical pharmacist interventions
Approximately half of the clinical pharmacist interventions were provided at the prescriber level, and 49.46% of the interventions were offered at the drug level, and mainly included adjustments of the type and dosage of drugs, as well as stopping or starting some drugs (Table 3). According to the results, 396 (85.53%) pharmaceutical interventions recommendations were accepted, and 67 (14.47%) recommendations were rejected for various reasons (Table 3).
DRP outcomes of pharmacist interventions
In total, 390 DRPs (84.23%) were resolved after implementation of interventions by a clinical pharmacist (Table 4). The proportion of patients who experienced DRPs decreased to 7.77%, with an average of 0.08 (SD 0.28) DRPs during hospitalization after pharmacist intervention. Wilcoxon signed ranks test result showed a significant reduction in the mean number of DRPs after the pharmacist’s intervention in this single center study (p = 0.000).
Seventy-three DRPs (15.77%) occurred even with the intervention of a pharmacist, failure to follow the recommendation by the prescriber was the main reason (72.60%) (Table 4). Lack of cooperation by the patient (6.85%) was another reason. In 15 cases (20.55%), DRP remained unsolved even though the pharmacist’s recommendations were followed by the prescriber (Table 4). Some typical cases are listed in the appendix for ease of understanding.
Among the 56 unresolved DRPs due to lack of cooperation by the patient or prescriber, 10 cases of DRP induced consequences, such as acute kidney disease, mental agitation and elevated blood glucose. The most serious consequence induced by DRP was systemic submucosal hemorrhage in a hemodialysis patient with pneumonia; according to the pharmacist’s evaluation using the World Health Organization (WHO) Uppsala adverse events scale, this symptom was likely caused by an improper dosage of cefoperazone sodium and sulbactam sodium. Among the remaining 46 unsolved DRPs, there was clearly an irrational use of medication, but no severe consequences were reported.
Contributing factors of DRPs
CKD stage 4, number of comorbid diseases, number of prescribed medications, and hospitalization days were contributing factors of DRPs in both the univariate and multivariate logistic regression models (Table 5). In contrast to the results of the univariate regression analysis, CKD stage 5 showed no statistical significance in the multivariate regression model.
Discussion
In this prospective study, we established that the clinical pharmacist’s intervention could identify and address DRPs in hospitalized patients with CKD by attending ward rounds, reviewing order daily and providing MRE. The services of clinical pharmacists have been effective in decreasing DRPs in China [23, 24]. To our knowledge, this is the first large prospective study that was performed for one year to assess the potential role of clinical pharmacist services in hospitalized patients with CKD in China.
According to a systematic review of 20 studies in 2021, the prevalence of DRP in CKD patients ranged from 12% to 87%, with 0.4–1.7 DRPs per patient [14]. In this study, 45.95% (420/914) of CKD inpatients experienced DRPs, with an average of 0.51 (SD, 0.60) DRPs per person before pharmacist intervention. In a 2014 retrospective study conducted in another general hospital in Zhejiang Province, researchers analyzed 1733 lines of medication prescriptions from 202 patients with CKD and found that the prevalence of inappropriate medication prescriptions in hospitalized patients with CKD was 15.18% [9]. These data indicate that DRPs are a common phenomenon in hospitalized patients with CKD in China. The major reason for DRPs was drug/dose selection (89.85%), according to the PCNE classification tool version 9.00, a general DRP analysis method [6]. Regarding drug selection, the irrational use of antibiotics (32.84%) and cardiovascular agents (28.66%) were the main contributors to DRPs, similar to other studies [9, 10, 25]. We found that the most common comorbidities of patients with CKD were hypertension (74.84%) and diabetes mellitus (34.79%), which might explain why the unreasonable use of cardiovascular agents was common. This was largely due to unreasonable drug combinations or inappropriate drug selection in this study. For instance, the combination of a losartan potassium hydrochlorothiazide tablet and irbesartan tablet has been observed in this study. This is a typical irrational drug combination because both drugs contain the same mechanism of action. However, most DRPs due to the wrong dosage were caused by the antimicrobials. This was consistent with the data reported by Yang Ping, with unreasonable dosages of antimicrobial drugs (89.29%) being the most common category [9]. Some antibacterial drugs, such as levofloxacin and vancomycin which are mainly excreted through the kidneys, need dosage adjustment in the patients with end-stage renal disease [12, 13]. Excessive use of these drugs is usually accompanied by the deterioration of renal function. However, dose adjustment was not always strictly implemented, as there were 83 DRPs due to overdose in our study.
In this study, 85.53% of pharmacist’s recommendations were accepted, and 84.23% of DRPs were consequently solved. Through intervention by the pharmacist, the proportion of patients who experienced DRPs decreased from a possible 45.95% to 7.77%, with the average number of DRPs per patient decreasing sharply (possible, 0.51 ± 0.60 vs. actual, 0.08 ± 0.28). These findings suggest that even only one clinical nephrology pharmacist in the nephrology ward, clinical pharmacist can play an important role in facilitating the identification of DRPs in patients with CKD and assisting physicians resolve DRPs in this single center study in China. It should be noted that 67 pharmacist recommendations were not accepted, with objections from doctors being the main reason (91.04%) in this study. Physician’s objections to pharmacist interventions are known to be common [18, 26]. In this hospital the possible reasons for physicians to not accept pharmacist’s interventions might have been: first, when the laboratory indicators in a CKD patient are slightly abnormal, the clinical pharmacist may be more inclined to adjust the medication order. Doctors often tend to pay more attention to dynamic indicator change trends and adjust the prescriptions only when parameters become highly abnormal or relevant clinical symptoms appear. We also noted that in 61 cases of DRPs, the clinicians initially disagreed with the pharmacist, whereas only 53 DRPs were not resolved due to the lack of cooperation by the prescriber (Tables 3 and 4). This indicated that in 8 DRP cases, the clinician eventually adopted the pharmacist’s medication plan. Second, pharmacist prefer medication treatment regimens in line with guidelines or drug instructions; however, physicians consider the efficacy and safety of treatment, patient compliance, financial status of the patient and make clinical decisions after comprehensive consideration. In 5 cases, DRPs remained unsolved due to the lack of cooperation by patients. These findings suggest that pharmacist needs to obtain an in-depth clinical understanding of the needs of patients to provide the most appropriate pharmaceutical advice.
Comorbidities and number of prescribed medicines ≥ 5 are contributing factors in the occurrence of DRPs, and this has been proven in several studies [5, 10, 11]. Two studies have demonstrated that a hospitalization period longer than five days increases the possibility of DRPs [11, 25]. We obtained similar conclusions in this study: the number of comorbid diseases, use of multiple prescription drugs, and an extended length of hospital stay were contributing factors of DRPs. Some studies have shown that CKD stage is an independent risk factor for DRPs [5, 11, 25, 27]. However, we found that only stage 4 CKD was remarkably correlated with DRPs in both the univariate and multivariate logistic regression analyses. The possible reasons are as follows: most patients with stage 5 CKD are receiving regular dialysis, visit the hospital frequently, and receive more attention from clinicians than patients with lower stages. Moreover, doctors clearly know whether a medication is appropriate and how to adjust the dose for dialysis patients. We observed that a tailored approach for patients with stage 4 CKD might be more complicated and difficult for doctors. Dapagliflozin, for instance, is forbidden in patients undergoing dialysis; however, many clinicians ignore the contraindication when the eGFR is < 30 mL/min/1.73 m2. CKD stage 5 was a statistically significant variable in the univariate logistic regression model, but significance was not retained in the multiple regression model. This might be due to the high proportion of patients with stage 5 CKD (64.44%) in the total sample. These data remind us that patients with severe renal insufficiency should receive more care from both clinicians and pharmacists, regardless of whether they are undergoing dialysis.
Limitations
This study has some limitations. First, only one clinical nephrology pharmacist was present in the hospital where the study was conducted. This led to the observed results in this study highly dependent on this pharmacist. If multiple clinical pharmacists together participate in the management of DRPs in hospitalized patients with CKD, the incidence and intervention effect of DRPs might differ from this study’s results. Second, this single-center study is likely to have sampling bias due to the large population base of CKD in China. The data obtained from multi-center study might be closer to the reality.
Conclusion
This study confirmed that DRPs are common among hospitalized patients with CKD in China. CKD stage 4, comorbidities, use of multiple prescription drugs, and an extended length of hospital stay were contributing factors for DRPs. Even only one clinical nephrology pharmacist in the nephrology ward, clinical pharmacist can play an important role in facilitating the identification of DRPs in patients with CKD and assisting physicians resolve DRPs in this single center study in China.
Data Availability
All data generated during this study are included in this published article. The dataset analyzed during the study is available from the corresponding author upon reasonable request.
Abbreviations
- CI:
-
Confidence interval
- CKD:
-
Chronic kidney disease
- CK-NET:
-
China Kidney Disease Network
- DRP:
-
Drug-related problem
- eGFR:
-
Estimated glomerular filtration rate
- HIS:
-
Hospital information system
- KDIGO:
-
Kidney Disease: Improving Global Outcomes
- MEM:
-
Medication evaluation and management
- MR:
-
Medication reconciliation
- MRE:
-
Medication-related education
- OR:
-
Odds ratio
- PCNE:
-
Pharmaceutical Care Network Europe
- SD:
-
Standard deviation
References
GBD Chronic Kidney Disease Collaboration. Global, regional, and national burden of chronic Kidney Disease, 1990–2017: a systematic analysis for the global burden of Disease Study 2017. Lancet. 2020;395(10225):709–33.
Lin B, Shao L, Luo Q, Ou-yang L, Zhou F, Du B, He Q, Wu J, Xu N, Chen J. Prevalence of chronic Kidney Disease and its association with metabolic Diseases: a cross-sectional survey in Zhejiang Province, Eastern China. BMC Nephrol. 2014;15:36.
Wang F, Yang C, Long J, Zhao X, Tang W, Zhang D, Bai K, Su Z, Gao B, Chu H, Wang J, Sun X, Wang S, Zuo L, Wang Y, Yu F, Wang H, Zhang L, Zhao MH. Executive summary for the 2015 Annual Data Report of the China Kidney Disease Network (CK-NET). Kidney Int. 2019;95(3):501–5.
Subeesh VK, Abraham R, Satya-Sai MV, Koonisetty KS. Evaluation of prescribing practices and drug-related problems in chronic Kidney Disease patients: a cross-sectional study. Perspect Clin Res. 2020;11(2):70–4.
Garedow AW, Mulisa-Bobasa E, Desalegn-Wolide A, Kerga-Dibaba F, Gashe-Fufa F, Idilu-Tufa B, Debalke S, Kumela-Goro K. Drug-Related Problems and Associated Factors among Patients Admitted with Chronic Kidney Disease at Jimma University Medical Center, Jimma Zone, Jimma, Southwest Ethiopia: A Hospital-Based Prospective Observational Study. Int J Nephrol. 2019; 2019:1504371.
Pharmaceutical Care Network Europe (PCNE) DRP Classification V9.00. 2019. https://www.pcne.org/upload/files/410_PCNE_classification_V9-0m.pdf. Accessed 29 Sept 2023.
Ni XF, Yang CS, Bai YM, Hu ZX, Zhang LL. Drug-related problems of patients in primary health care institutions: a systematic review. Front Pharmacol. 2021;17:1–14.
Tonelli M, Wiebe N, Guthrie B, James MT, Quan H, Fortin M, Klarenbach SW, Sargious P, Straus S, Lewanczuk R, Ronksley PE, Manns BJ, Hemmelgarn BR. Comorbidity as a driver of adverse outcomes in people with chronic Kidney Disease. Kidney Int. 2015;88(4):859–66.
Yang P, Chen N, Wang RR, Li L, Jiang SP. Inappropriateness of medication prescriptions about chronic Kidney Disease patients without dialysis therapy in a Chinese tertiary teaching hospital. Ther Clin Risk Manag. 2016;12:1517–24.
Saleem A, Masood I. Pattern and predictors of medication dosing errors in chronic Kidney Disease patients in Pakistan: a single center retrospective analysis. PLoS ONE. 2016;11(7):e0158677.
Saleem A, Masood I, Khan TM. Clinical relevancy and determinants of potential drug-drug interactions in chronic Kidney Disease patients: results from a retrospective analysis. Integr Pharm Res Pract. 2017;6:71–7.
Hoff BM, Maker JH, Dager WE, Heintz BH. Antibiotic dosing for critically Ill adult patients receiving intermittent hemodialysis, prolonged intermittent renal replacement therapy, and continuous renal replacement therapy: an update. Ann Pharmacother. 2020;54(1):43–55.
Crew P, Heintz SJ, Heintz BH. Vancomycin dosing and monitoring for patients with end-stage renal Disease receiving intermittent hemodialysis. Am J Health Syst Pharm. 2015;72(21):1856–64.
Alruqayb WS, Price MJ, Paudyal V, Cox AR. Drug-related problems in hospitalised patients with chronic Kidney Disease: a systematic review. Drug Saf. 2021;44(10):1041–58.
Stemer G, Lemmens-Gruber R. Clinical pharmacy activities in chronic Kidney Disease and end-stage renal Disease patients: a systematic literature review. BMC Nephrol. 2011;12:35.
Salgado TM, Moles R, Benrimoj SI, Fernandez-Llimos F. Pharmacists’ interventions in the management of patients with chronic Kidney Disease: a systematic review. Nephrol Dial Transplant. 2012;27(1):276–92.
Quintana-Bárcena P, Lord A, Lizotte A, Berbiche D, Lalonde L. Prevalence and management of drug-related problems in chronic Kidney Disease patients by severity level: a subanalysis of a cluster randomized controlled trial in community pharmacies. J Manag Care Spec Pharm. 2018;24(2):173–81.
Hailu BY, Berhe DF, Gudina EK, Gidey K, Getachew M. Drug related problems in admitted geriatric patients: the impact of clinical pharmacist interventions. BMC Geriatr. 2020;20(1):13.
Al-Raiisi F, Stewart D, Fernandez-Llimos F, Salgado TM, Mohamed MF, Cunningham S. Clinical pharmacy practice in the care of chronic Kidney Disease patients: a systematic review. Int J Clin Pharm. 2019;41(3):630–66.
Song YK, Jeong S, Han N, Na H, Jang HY, Sohn M, Kim YS, Joo KW, Oh KH, Kim DK, Lee H, Oh JM, DrugTEAM Study Group. Effectiveness of clinical Pharmacist Service on Drug-related problems and patient outcomes for hospitalized patients with chronic Kidney Disease: a Randomized Controlled Trial. J Clin Med. 2021;10(8):1788.
Garin N, Sole N, Lucas B, Matas L, Moras D, Rodrigo-Troyano A, Gras-Martin L, Fonts N. Drug related problems in clinical practice: a cross-sectional study on their prevalence, risk factors and associated pharmaceutical interventions. Sci Rep. 2021;11(1):883.
Pai AB, Boyd A, Depczynski J, Chavez IM, Khan N, Manley H. Reduced drug use and hospitalization rates in patients undergoing hemodialysis who received pharmaceutical care: a 2-year, randomized, controlled study. Pharmacotherapy. 2009;29(12):1433–40.
Zhu XT, Hang YF. Clinical pharmacists’ pharmaceutical care and practice in the department of nephrology. Chinese Journal of clinical pharmacology and therapeutics. Chin J Clin Pharmacol Ther. 2018;23(10):1174–8.
Le KD, Liang Y, Yang CQ. Medication reconciliation by clinical pharmacists for patients with chronic Kidney Disease. Chin J New Drugs 2017,26(10):1213–8.
Prajapati A, Ganguly B. Appropriateness of drug dose and frequency in patients with renal dysfunction in a tertiary care hospital: a cross-sectional study. J Pharm Bioallied Sci. 2013;5(2):136–40.
Ma Z, Sun S, Zhang C, Yuan X, Chen Q, Wu J, Wang X, Liu L. Characteristics of drug-related problems and pharmacists’ interventions in a geriatric unit in China. Int J Clin Pharm. 2021;43(1):270–4.
Sheen SS, Choi JE, Park RW, Kim EY, Lee YH, Kang UG. Overdose rate of Drugs requiring renal dose adjustment: data analysis of 4 years prescriptions at a tertiary teaching hospital. J Gen Intern Med. 2008;23(4):423–8.
Acknowledgements
We would like to thank Editage (www.editage.cn) and SPRINGER NATURE Author Servieces for English language editing.
Funding
The study was funded by the Public welfare Program of the Science and Technology Department of Zhejiang Province(LGF20H310005); Zhejiang Provincial Project for Medical and Health Science and Technology(2022KY063,2020KY051); and Special scientific research fund project of Hospital Pharmacy of Zhejiang Pharmaceutical Association(2021ZYY30).
Author information
Authors and Affiliations
Contributions
SZ collected the sociodemographic data of inpatients with CKD and wrote the manuscript. XLY, the nephrology clinical pharmacist in this study, identified DRPs and provided pharmaceutical suggestions. GBZ,PH, YR, BL and YFS contributed to data analysis and manuscript revision. All the authors have read and approved the manuscript.
Corresponding author
Ethics declarations
Ethics approval and consent to participate
All intervention process in this study were approved by Ethics Committee of Zhejiang Provincial People’s Hospital (ZJPPHEC 2019O(014)). Participation of patients was entirely voluntary. Each participant or its legal guardian was asked to sign a written informed consent before data collection and pharmacist intervention. All methods were carried out in accordance with relevant guidelines and regulations. The right of participants not to participate was respected. The patient confidentiality and data information are strictly protected.
Consent of publication
Not applicable.
Competing interests
All authors declare no competing interests in this study.
Additional information
Publisher’s Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Electronic supplementary material
Below is the link to the electronic supplementary material.
Rights and permissions
Open Access This article is licensed under a Creative Commons Attribution 4.0 International License, which permits use, sharing, adaptation, distribution and reproduction in any medium or format, as long as you give appropriate credit to the original author(s) and the source, provide a link to the Creative Commons licence, and indicate if changes were made. The images or other third party material in this article are included in the article’s Creative Commons licence, unless indicated otherwise in a credit line to the material. If material is not included in the article’s Creative Commons licence and your intended use is not permitted by statutory regulation or exceeds the permitted use, you will need to obtain permission directly from the copyright holder. To view a copy of this licence, visit http://creativecommons.org/licenses/by/4.0/. The Creative Commons Public Domain Dedication waiver (http://creativecommons.org/publicdomain/zero/1.0/) applies to the data made available in this article, unless otherwise stated in a credit line to the data.
About this article
Cite this article
Zhang, S., Zhang, Gb., Huang, P. et al. Drug-related problems in hospitalized patients with chronic kidney diseases and clinical pharmacist interventions. BMC Geriatr 23, 849 (2023). https://doi.org/10.1186/s12877-023-04557-y
Received:
Accepted:
Published:
DOI: https://doi.org/10.1186/s12877-023-04557-y