Abstract
In Japan, β-lactamase-nonproducing, ampicillin-resistant organisms have been evident among Haemophilus influenzae type b (Hib) isolates since 2000, when no appropriate vaccine had been approved. We therefore performed molecular analysis of agents causing H. influenzae meningitis nationwide over the following 10 years. Some 285 institutions have participated in surveillance since 2000. The capsular type and resistance genes of 1,353 isolates and 23 cerebrospinal fluid samples from pediatric patients with meningitis we had received from 2000 to 2011 were analyzed by polymerase chain reaction. Blood and spinal fluid test results obtained when patients were admitted were examined for correlation with outcomes. Hib was found in 98.9 % of isolates. We received more than 100 Hib isolates per year until vaccination began in December 2008, when these isolates decreased, especially since establishment of a special fund to promote vaccination in November 2010. Decreased incidence among infants 7 months to 2 years old has been particularly notable. However, the rate of ampicillin-resistant organisms has increased to more than 60 % of all isolates since 2009. We received 587 replies to a questionnaire concerning outcomes, indicating 2 % mortality and 17.7 % serious morbidity. Age of 6 months or younger and presence of disseminated intravascular coagulation at admission were related to an unfavorable outcome (p < 0.05), but ampicillin resistance was not. Combination therapy with third-generation cephem and carbapenem agents was used initially for 72 % of patients. Routine immunization can prevent Hib meningitis in children.
Similar content being viewed by others
Introduction
Community-acquired bacterial meningitis in children is a serious infection that occasionally is fatal. Pathogens and infection rate differ according to patient age; availability of vaccination against Haemophilus influenzae type b (Hib), Streptococcus pneumoniae, and others; and location in a developed versus a developing country.
Hib is well known to cause meningitis, epiglottitis, purulent arthritis, pericarditis, pneumonia, and other infections in infants and children over 3 months of age. Based on data from our surveillance [1] and from Ishiwada et al. [2], the incidence of Hib is approximately 10 to 12 per 100,000 children under 5 years of age. However, Hib meningitis already is uncommon in many countries where Hib vaccination has been introduced. Unfortunately, Hib vaccine was not approved by the Japanese Ministry of Health, Labour and Welfare until January 2007, and voluntary vaccination of children only began in late 2008. In November 2010, vaccination of children with Hib and heptavalent pneumococcal conjugate vaccine (PCV7) was recommended by the Provisional Special Fund for the Urgent Promotion of Vaccination against Such Diseases as Cervical Cancer. The vaccination rate among infants at risk throughout Japan is estimated to be 40–60 % as of the end of 2011.
Meanwhile, the rate of β-lactamase-nonproducing, ampicillin (AMP)-resistant H. influenzae (BLNAR) and Hib isolates from patients with meningitis have increased rapidly in parallel with their exponential increase in patients with respiratory tract infections (RTI) [1, 3, 4]. Although BLNAR strains showing decreased affinity for β-lactam antibiotics were first described in the United States in the 1980s [5, 6], these strains have remained rare in that country [7, 8] and in the European Union (EU) [9–11], except for France.
The resistance mechanism in BLNAR involves mutations in the ftsI gene encoding penicillin-binding protein 3 (PBP3), which mediates septal peptidoglycan synthesis in the cell wall. PBP3 is the main target of cephalosporin antibiotics, which differs from that of penicillins and carbapenems. Accordingly, susceptibility to cephalosporin clearly is affected by ftsI gene mutations [12]. We have identified amino acid substitutions at three PBP3 positions mainly associated with decreased β-lactam susceptibility: Asn526Lys, Arg517His, and Ser385Thr. Strains with substitutions of either Asn526Lys or Arg517His and also Ser385Thr were classified as genotypic BLNAR (gBLNAR) based on correlations with β-lactam susceptibility. Other strains with only Asn526Lys or Arg517His substitutions were classified as genotypic Low-BLNAR (gLow-BLNAR). In Australia [13], France [14], and Norway [15], the incidence of gLow-BLNAR isolates possessing an Asn526Lys substitution with AAA sequences was significant, but not in Japan, where AAG sequences contributed to this substitution.
In this report, we describe results in H. influenzae isolates from meningitis patients collected by the Nationwide Surveillance for Bacterial Meningitis (NSBM) working group and impact on survival outcome and presence or absence of sequelae for the following: yearly changes in genotypic β-lactam resistance, blood and spinal fluid test results, and antibiotics initially used at disease onset.
Materials and methods
Patients and strains
A total of 1,353 H. influenzae strains isolated from cerebrospinal fluid (CSF) collected from pediatric patients with bacterial meningitis were sent to Kitasato Institute for Life Sciences from clinical laboratories at 285 Japanese medical institutions between January 2000 and December 2011. CSF samples sent by pediatricians for identification of the causative pathogen also included 23 samples containing H. influenzae DNA. These strains and clinical samples were sent to our laboratory accompanied by two documents that protected the anonymity of the patient: one is a record of the informed consent obtained from the guardians of the infants and children, and the other is a survey form that was filled out by the attending physician.
Genotypic determination of β-lactam resistance was performed immediately by polymerase chain reaction (PCR) on all isolates received to determine ftsI gene mutations as described in the following section. These PCR results were immediately reported to the referring pediatrician and the laboratory technicians.
Polymerase chain reaction
Conventional PCR [16] was performed on H. influenzae isolates using six sets of primers that we had constructed for routine use in our laboratory: P6 primers to amplify the p6 gene for identification of the H. influenzae species; TEM-1 primers to amplify a part of the TEM-1-type β-lactamase gene (bla TEM); ROB-1 primers to amplify a part of the ROB-1-type β-lactamase gene (bla ROB); PBP3-S primers to identify an Asn526Lys amino acid substitution in the ftsI gene; PBP3-BLN primers to identify Asn526Lys and Ser385Thr amino acid substitutions in the ftsI gene; and serotype b primers to amplify a part of the Hib-specific capB locus. PCR cycling conditions were 35 cycles at 94 °C for 15 s; 53 °C for 15 s, and 72 °C for 15 s.
Thereafter, Asn526Lys and Ser385Thr amino acid substitutions were separately identified by the real-time PCR method we constructed in 2007 [17].
Isolates suspected to have an Arg517His substitution based on susceptibility to ampicillin (AMP) and cefotaxime (CTX) were subjected to direct sequencing to detect this substitution, because useful primers could not be designed.
Genotypic resistance patterns were classified as follows: gBLNAS, without any of the three substitutions; gBLPAR, producing β-lactamase TEM-1 or ROB-1; gLow-BLNAR, with substitution of Asn526Lys or Arg517His; gBLNAR, with two or three substitutions, Asn526Lys or Arg517His, as well as Ser385Thr; gBLPACR-I, producing β-lactamase but having a gLow-BLNAR genotype; and gBLPACR-II, also producing β-lactamase but having a gBLNAR genotype.
Statistical analysis
We used Microsoft Excel 2010 for Statistics (SSRI, Tokyo, Japan) and Prism Version 5.0 (GraphPad Software, La Jolla, CA, USA) for data analysis. Categorical variables were compared using chi-squared tests. Continuous variables were compared using Student’s t test. A p value less than 0.05 indicated a significant difference between groups.
Results
Changes in resistance among strains for year to year
A breakdown of Hib and nontypeable H. influenzae (NTHi) among 1,353 isolates and 23 spinal fluid samples collected from pediatric inpatients with H. influenzae meningitis during the study period is shown in Table 1. Among all isolates, 98.9 % were identified to be serotype b; the remaining 1.1 % represented NTHi. One quarter of spinal fluid samples were shown to contain Hib DNA by real-time PCR. No other serotypes were recognized.
Figure 1 shows year-to-year changes in β-lactam resistance among strains. Resistance was identified molecularly by conventional PCR (from 2000 to 2009) and by real-time PCR (from 2010 to 2011) for the ftsI gene encoding PBP3, the bla TEM gene encoding TEM-1 β-lactamase, and the bla ROB gene encoding ROB-1 β-lactamase, respectively [16, 17]. For strains that showed discrepancies between their susceptibility for AMP or CTX and the results of PCR, the ftsI gene was analyzed by sequencing.
Year-to-year changes in genotypically classified resistance types among strains isolated between 2000 and 2011. g genotype; Hib type b Haemophilus influenzae; gBLNAS β-lactamase-nonproducing, ampicillin (AMP) susceptible H. influenzae; gBLNAR β-lactamase-nonproducing, AMP-resistant H. influenzae; gLow-BLNAR β-lactamase-nonproducing, low-level AMP-resistant H. influenzae; gBLPAR TEM-1 β-lactamase-producing, AMP-resistant H. influenzae; gBLPACR TEM-1 β-lactamase-producing, amoxicillin/clavulanic acid-resistant H. influenzae
As shown in Fig. 1, Hib gBLNAR first was identified as a novel resistant strain in 2000. Since then, the resistance rate has increased exponentially over time, exceeding 60 % in 2009 and reaching approximately 70 % in 2011. Over the same interval, gBLNAS and gBLPAR, respectively, decreased from 32 and 26 % in 2000 to 8 and 0 % in 2011.
Distributions of patient age and β-lactam resistance by year
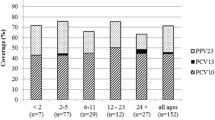
Yearly distribution of patient age and β-lactam resistance according to genotypic identification is shown in Fig. 2. Hib vaccination of children began on a voluntary basis on December 19, 2008. Subsequently, the immunization rate for Hib in Japanese children up to 1 year old is estimated to have been approximately 10 % in 2009, 20 % in 2010, and 50–60 % in 2011, representing an increase every year (data not shown here).
Although longitudinal surveillance demonstrated that the largest number of patients up to 1 year old continued until 2008, these patients decreased beginning in 2009 when Hib vaccination started. In 2011, the total of cases decreased dramatically to 46, about half the usual collected strains. Further, no differences in prevalence of gBLNAR were seen between age groups.
Details of sequelae
Details of sequelae in patients with H. influenzae meningitis are listed in Table 2.
This information was obtained from the questionnaires completed by attending physicians. Among the 655 responses, details concerning patients with or without sequelae were recorded in 587 cases. Death was reported in 12 patients (2.0 %), whereas serious sequelae, mainly including brain atrophy or infarction, motor dysfunction, and auditory or visual dysfunction, were noted in 104 (17.7 %).
Characteristics of patients with and without sequelae
Table 3 compares characteristics of patients with versus without sequelae after the onset of Hib meningitis. Although sequelae were more frequent in patients 6 months old or younger at the time of onset, significant differences in onset age were observed between the two groups (p < 0.05). The presence of disseminated intravascular coagulation (DIC) also significantly affected sequelae.
No significant differences were noted in blood test and spinal fluid test results. Outcome also was not affected by resistance type of the Hib pathogen, namely, whether gBLNAR or not.
Correlation between antimicrobial choice and outcome
Relationships between initial antimicrobial therapy given to meningitis patients on hospital admission and outcomes are shown in Fig. 3. Half the patients (n = 305, 52.3 %) received initial therapy with combinations of a third-generation cephem and a carbapenem agent, namely, CTX and meripenem (MEM) or panipenem (PAM), or ceftriaxone (CRO) and MEM or PAM. The next most frequent treatment was AMP and CTX or CRO therapy (18.3 %). Monotherapy with CTX or CRO was given only to 12.7 %.
When the causative agent was identified as H. influenzae, the therapeutic regimen was changed to combination therapy. A significant relationship between antimicrobial choice and outcome was not observed.
Discussion
Bacterial meningitis is an infectious disease with a high occurrence rate of fatalities and serious sequelae in children. Accordingly, vaccine development has been attempted for many years. The Hib conjugate vaccine was developed to prevent occurrence of bacterial meningitis and severe infections caused by capsular type b H. influenzae, the most frequent causative organism. In the United States, Hib vaccine was licensed for use in children in 1987 and entered the standard vaccination schedule in 1990 [18, 19]. As a result, a dramatic decrease in bacterial meningitis from Hib became evident after a few years [19–21]. This vaccination then was introduced in many other countries, where Hib infection now has become a largely eradicated disease.
In Japan, introduction of Hib vaccine was much delayed, for reasons including a low incidence of bacterial meningitis from Hib relative to other countries; high accessibility of Japanese medical institutions; easily used antibiotics; and lack of a feeling of urgency concerning vaccination.
During the decade preceding Japanese adoption of the vaccine, gBLNAR, a new resistant strain, emerged among Hib isolates [1]. These resistant bacteria increased rapidly, causing a major therapeutic problem. Previously, 22–26 % of Hib isolates were β-lactamase-producing strains [1, 3], so the first-choice agent was a third-generation cephem, CTX [22]. To address the problem of gBLNAR, treatment shifted heavily to combination therapy with a third-generation cephem and carbapenem [22], based on the mechanism of resistance in these strains. The targets of β-lactam antibiotics are the penicillin-binding proteins (PBPs) involved in peptidoglycan synthesis; in BLNAR, the ftsI gene encoding PBP3 shows a number of important mutations [12].
Therefore, BLNAR susceptibility to cephems, which target mainly PBP3, is 50–100 times decreased compared to that of susceptible organisms. However, because the main target of carbapenems is unrelated to PBP3, susceptibility of BLNAR to carbapenem is not affected [3]. A synergistic effect from a combination of two kinds of agents with their different target sites is expected.
The Hib vaccine was approved in Japan in January 26, 2007, and has been marketed since December 19, 2008. Accurate nationwide vaccination numbers are not available, but the estimated vaccination rate in the infant population (up to 1 year of age), based on numbers of vials delivered, was 10 % in 2009, 20 % in 2010, and 40–60 % in 2011. The high vaccination rate in 2011 is attributable largely to official support provided by the Provisional Special Fund for the Urgent Promotion of Vaccination Against Such Diseases as Cervical Cancer. This initiative includes Hib and PCV7 vaccination of infants.
Incidence of Hib meningitis among children 7 months to 1 year of age has decreased gradually since 2009 in our results, reflecting the effect achieved by Hib vaccination. However, the decrease in incidence among infants under 6 months of age is less evident than that among those between 7 months and 3 years old. Infants vaccinated at such a young age may have difficulty producing antibody titers sufficient to prevent Hib infection at that stage.
Continued surveillance is needed to see how the incidence of Hib meningitis may change in the future.
References
Hasegawa K, Chiba N, Kobayashi R, Murayama SY, Iwata S, Sunakawa K, et al. Rapidly increasing prevalence of β-lactamase-nonproducing, ampicillin-resistant Haemophilus influenzae type b in meningitis. Antimicrob Agents Chemother. 2004;48:1509–14.
Ishiwada N, Kurosaki T, Terashima I, Ishikawa N, Kaneko K, Kuroki H, et al. The incidence of pediatric Haemophilus influenzae systemic infections. Shounikagaku Zasshi. 2007;111:1568–72 (in Japanese).
Hasegawa K, Kobayashi R, Takada E, Ono A, Chiba N, Morozumi M, et al. High prevalence of type b beta-lactamase-non-producing ampicillin-resistant Haemophilus influenzae in meningitis: the situation in Japan where Hib vaccine has not been introduced. J Antimicrob Chemother. 2006;57:1077–82.
Ubukata K. Problems associated with high prevalence of multi-drug resistant bacteria in patients with community-acquired infections. J Infect Chemother. 2003;9:285–91.
Mendelman PM, Chaffin DO, Stull TL, Rubens CE, Mack KD, Smith AL. Characterization of non-β-lactamase-mediated ampicillin resistance in Haemophilus influenzae. Antimicrob Agents Chemother. 1984;26:235–44.
Parr TR Jr, Bryan LE. Mechanism of resistance of an ampicillin-resistant, β-lactamase-negative clinical isolate of Haemophilus influenzae type b to β-lactam antibiotics. Antimicrob Agents Chemother. 1984;25:747–53.
Karlowsky JA, Critchley IA, Blosser-Middleton RS, Karginova EA, Jones ME, Thornsberry C, et al. Antimicrobial surveillance of Haemophilus influenzae in the United States during 2000–2001 leads to detection of clonal dissemination of a β-lactamase-negative and ampicillin-resistant strain. J Clin Microbiol. 2002;40:1063–6.
Heilmann KP, Rice CL, Miller AL, Miller NJ, Beekmann SE, Pfaller MA, Richter SS, Doern GV. Decreasing prevalence of beta-lactamase production among respiratory tract isolates of Haemophilus influenzae in the United States. Antimicrob Agents Chemother. 2005;49:2561–4.
Jansen WT, Verel A, Beitsma M, Verhoef J, Milatovic D. Surveillance study of the susceptibility of Haemophilus influenzae to various antibacterial agents in Europe and Canada. Curr Med Res Opin. 2008;24:2853–61.
Pérez-Trallero E, Martín-Herrero JE, Mazón A, García-Delafuente C, Robles P, Iriarte V, et al. Antimicrobial resistance among respiratory pathogens in Spain: latest data and changes over 11 years (1996–1997 to 2006–2007). Antimicrob Agents Chemother. 2010;54:2953–9.
Witherden EA, Montgomery J, Henderson B, Tristram SG. Prevalence and genotypic characteristics of β-lactamase-negative ampicillin-resistant Haemophilus influenzae in Australia. J Antimicrob Chemother. 2011;66:1013–5.
Ubukata K, Shibasaki Y, Yamamoto K, Chiba N, Hasegawa K, Takeuchi Y, et al. Association of amino acid substitutions in penicillin-binding protein 3 with β-lactam resistance in β-lactamase-negative ampicillin-resistant Haemophilus influenzae. Antimicrob Agents Chemother. 2001;45:1693–9.
Witherden EA, Kunde D, Tristram SG. An evaluation of SNP-based PCR methods for the detection of β-lactamase-negative ampicillin-resistant Haemophilus influenzae. J Infect Chemother. doi:10.1007/s10156-011-0356-5.
Dabernat H, Delmas C, Seguy M, Pelissier R, Faucon G, Bennamani S, et al. Diversity of beta-lactam resistance conferring amino acid substitutions in penicillin-binding protein 3 of Haemophilus influenzae. Antimicrob Agents Chemother. 2002;46:2208–18.
Skaare D, Allum AG, Anthonisen IL, Jenkins A, Lia A, Strand L, et al. Mutant ftsI genes in the emergence of penicillin-binding protein-mediated beta-lactam resistance in Haemophilus influenzae in Norway. Clin Microbiol Infect. 2010;16:1117–24.
Hasegawa K, Yamamoto K, Chiba N, Kobayashi R, Nagai K, Jacobs MR, et al. Diversity of ampicillin-resistance genes in Haemophilus influenzae in Japan and the United States. Microb Drug Resist. 2003;9:39–46.
Kishii K, Morozumi M, Chiba N, Ono A, Ubukata K. Direct detection by real-time PCR of ftsI gene mutations affecting MICs of β-lactam agents for Haemophilus influenzae isolates from meningitis. J Infect Chemother. 2011;17:671–7.
Schoendorf KC, Adams WG, Kiely JL, Wenger JD. National trends in Haemophilus influenzae meningitis mortality and hospitalization among children, 1980 through 1991. Pediatrics. 1994;93:663–8.
Adams WG, Deaver KA, Cochi SL, Plikaytis BD, Zell ER, Broome CV, et al. Decline of childhood Haemophilus influenzae type b (Hib) disease in the Hib vaccine era. JAMA. 1993;269:221–6.
Centers for Disease Control and Prevention (CDC). Progress toward eliminating Haemophilus influenzae type b disease among infants and children—United States, 1987–1997. MMWR Morb Mortal Wkly Rep 1998;47:993–8.
Heikki P. Worldwide Haemophilus influenzae type b disease at the beginning of the 21st century: global analysis of the disease burden 25 years after the use of the polysaccharide vaccine and a decade after the advent of conjugates. Clin Microbiol Rev. 2000;13:302–17.
Sakai F, Hanaki H, Ikeda-Dantsuji Y, Hirao Y, Nonoyama M, Iwata S, et al. Trends in empirical chemotherapy of bacterial meningitis in children aged more than 4 months in Japan: a survey from 1997 through 2008. J Infect Chemother. 2011;17:358–62.
Acknowledgments
We deeply thank the pediatricians and laboratory technicians belonging to the 285 medical institutions for active cooperation. We also thank Keiko Hamano-Hasegawa for cooperation in construction of the PCR method and surveillance study. This study was supported in part by a grant under the category “Research on Emerging and Re-emerging Infectious Diseases” (number H21-002 and H22-013) from the Japanese Ministry of Health, Labour and Welfare (to K. Ubukata).
Author information
Authors and Affiliations
Consortia
Corresponding author
About this article
Cite this article
Ubukata, K., Chiba, N., Morozumi, M. et al. Longitudinal surveillance of Haemophilus influenzae isolates from pediatric patients with meningitis throughout Japan, 2000–2011. J Infect Chemother 19, 34–41 (2013). https://doi.org/10.1007/s10156-012-0448-x
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s10156-012-0448-x