Abstract
Multisegment intramedullary spinal cord tumors (MSICT) are a special type of spinal cord tumor. Up to now, no comparative clinical study of MSICT has been performed according to different age groups. Seventy-seven patients underwent microsurgery for MSICT. As grouped with two different methods, the parametric and nonparametric data of MSICT and patients were comparatively analyzed using statistically correlative methods. Forty-eight patients were males and 29 were females, ranging in age from 4 to 64 years (mean, 32.9 years). Among the six groups, being divided with intervals of 10 years, the whole difference in the initial symptoms of patients (Z = 17.4, P = 0.004) and in the histological classification of tumors (Z = 12.5, P = 0.03) was statistically significant, respectively. Neurodevelopmental tumor and benign glioma predominated in adolescents and decreased in frequency into adulthood where ependymoma became more predominant. In the 25 years old grouping method, there were 27 adolescent and 50 adult patients. The difference in initial symptoms of patients (Z = −2.08, P = 0.04) was statistically significant between the two groups. Pain with motor weakness and gait deterioration predominated in adolescents and decreased in frequency into adulthood where sensory disturbances became more predominant.



Similar content being viewed by others
References
Boström A, Hans FJ, Reinacher PC et al (2008) Intramedullary hemangioblastomas: timing of surgery, microsurgical technique and follow-up in 23 patients. Eur Spine J 17:882–886
Chang UK, Choe WJ, Chung SK et al (2002) Surgical outcome and prognostic factors of spinal intramedullary ependymomas in adults. J Neuro-oncol 57:133–139
Crawford JR, Zaninovic A, Santi M et al (2009) Primary spinal cord tumors of childhood: effects of clinical presentation, radiographic features, and pathology on survival. J Neurooncol 95:259–269
Dudek RW (2001) Skeletal system. In: Nieginski E (ed) High-yield embryology, 2nd edn. Lippincott Williams & Wilkins, Maryland, p 100
Houten JK, Weiner HI (2000) Pediatric intramedullary spinal cord tumors: special considerations. J Neuro-oncol 47:225–230
Huddart R, Traish D, Ashley S et al (1993) Management of spinal astrocytoma with conservative surgery and radiotherapy. Br J Neurosurg 7:473–481
Kasim KA, Thurnher MM, Mckeever P et al (2008) Intradural spinal tumors: current classification and MRI features. Neuroradiology 50:301–314
Kim MS, Chung CK, Choe GY et al (2001) Intramedullary spinal cord astrocytoma in adults: postoperative outcome. J Neuro-oncol 52:85–94
Lin YH, Huang CI, Wong TT et al (2005) Treatment of spinal cord ependymomas by surgery with or without postoperative radiotherapy. J Neuro-oncol 71:205–210
Makridou A, Argyriou AA, Karanasios P et al (2008) Bilateral drop foot secondary to a primary tumor in the conus medullaris. Muscle Nerve 37:778–780
McGirt MJ, Chaichana KL, Attenello F et al (2008) Spinal deformity after resection of cervical intramedullary spinal cord tumors in children. Childs Nerv Syst 24:93–97
Miller DJ, McCutcheon IE (2000) Hemangioblastomas and other uncommon intramedullary tumors. J Neuro-oncol 47:253–270
Nakamura M, Ishii K, Watanabe K et al (2008) Surgical treatment of intramedullary spinal cord tumors: prognosis and complications. Spinal Cord 46:282–286
New PW, Epi MC (2007) The influence of age and gender on rehabilitation outcomes in nontraumatic spinal cord injury. J Spinal Cord Med 30:225–237
Sandalcioglu IE, Gasser T, Asgari S et al. (2005) Functional outcome after surgical treatment of intramedullary spinal cord tumors: experience with 78 patients. Spinal Cord 43:34–41
Sandler HM, Papadopoulos SM, Thornton AF et al (1992) Spinal cord astrocytomas: results of therapy. Neurosurgery 30:490–493
Sharma NC, Chandra T, Sharma A et al (2009) Long-segment intramedullary spinal dermoid. India J Radiol Imaging 19:148–150
Sun JJ, Wang ZY, Li ZD et al (2009) Microsurgical treatment and functional outcomes of multi-segment intramedullary spinal cord tumors. J Clin Neurosci 16:666–671
Sun JJ, Wang ZY, Xie JC et al (2010) Comparative analysis the difference between multi-segments intramedullary spinal cord congenital tumors and benign ependymomas. J Pek Uni (Heal Sci) 42:89–93, in Chinese
Wilson PE, Oleszek JL, Clayton GH (2007) Pediatric spinal cord tumors and masses. J Spinal Cord Med 30:S15–S20
Acknowledgement
This work was supported by the Science Foundation for The Excellent Youth Scholars of Ministry of Education of China (BSD-09-6-11) and Science Foundation for The Excellent Youth Scholars of Peking University Third Hospital (74496-01). The authors thank Dr. Simon Glynn (from the Department of Neurology, University of Pennsylvania School of Medicine) for the revision and comments on the manuscript and Ms. Isabelle Liu (from the Washington University in St. Louis School of Medicine) for the final careful English-language editing.
Author information
Authors and Affiliations
Corresponding author
Additional information
Comments
Jörg Klekamp, Quakenbrück, Germany
Surgery on intramedullary tumors has come a long way since von Eiselsberg’s first successful operation on such a neoplasm in 1907. He observed a period of neurological deterioration before the patient made a good recovery. Such gratifying results were exceptional in those times when the surgeon’s major concern was saving the patient’s life rather than his neurological function. Throughout the past decades, every article on these tumors emphasized the need for an early diagnosis and an early operation as surgical morbidity was and still is directly related to the patient’s preoperative neurological function. With modern imaging techniques, we are in the fortunate position now to diagnose patients early. With modern microsurgical techniques and intraoperative neurophysiological monitoring, the preservation of function has become the rule rather than the exception if surgery is performed by experienced neurosurgeons. Wang et al. present their analysis of 77 multilevel intramedullary spinal cord tumors. Apart from well-established differences in the literature concerning the predominating tumor histologies in children and adults, the authors found lower surgical morbidities in younger patients both in terms of immediate postoperative function as well as potential recovery from a postoperative deterioration. These are important informations for preoperative patient counseling. Almost all patients experience some permanent loss of sensory function after an operation on a multilevel tumor. This may have significant consequences for coordination of movements. Preservation of motor functions alone may not be enough to preserve the patient’s walking abilities. Spinal ataxia is difficult to rehabilitate in elderly patients in particular. Regarding intraoperative neurophysiological monitoring, almost every paper focuses exclusively on the preservation of motor-evoked potentials. Many colleagues consider attempting to preserve sensory-evoked potentials a meaningless undertaking. I do not agree with such a view. To try to preserve as much sensory function as possible lowers postoperative morbidity. Furthermore, with exposure and removal of such a tumor, the posterior part of the spinal cord with its sensory pathways is manipulated before the anterior parts containing the motor tracts are reached. The surgeon can learn intraoperatively how to handle an individual tumor looking at SEP reactions. If SEPs are preserved, the chances to preserve MEPs as well will rise for certain.
Reference
1. Eiselsberg A Freiherr von, Ranzi E (1913) Über die chirurgische Behandlung der Hirn- und Rückenmarkstumoren. Arch Klin Chir 102:309–468
Jacques Brotchi, Brussels, Belgium
The authors bring interesting data in their comparative analysis on the diagnosis and treatments of MSICT between the different age groups. They point out differences in symptoms, histology, and prognosis. Nevertheless, I have several constructive criticisms, which may be summarized as follows:
–Lumbosacral tumors are not intramedullary lesions. Most are myxopapillary ependymomas arising from the filum and they should be included as true intramedullary tumors.
–If a midline myelotomy is the perfect approach for most ependymomas and astrocytomas [1, 2], that approach is not recommended for vascular tumors (hemangioblastomas, cavernomas). Most hemangioblastomas are subpial and should cautiously be separated from normal spinal cord through careful division of the pia all around the lesion [3, 4]. A myelotomy is surely not indicated.
–Astrocytoma may successfully remove in around 40% of cases. They cannot be completely removed with ease. This is in opposition with the literature [2, 5]. The infiltrating nature of most astrocytoma lesions makes total removal impossible without an unacceptable loss of neurological function [6].
–I am astonished to read that the overall postoperative status presented at the final follow-up review was improved in 84.4% of all patients (n = 65), unchanged in 11.7% (n = 9), and deteriorated in 3.9% (n = 3 with malignant gliomas). We know from the literature that the quality of the results closely depends on the preoperative neurological status. In large published series, it is said that more than 50% of patients are stabilized. Furthermore, in experienced hands, the rate of worsening runs from 5% to 20% in intramedullary low-grade gliomas according to the preoperative neurological status (McCormick grades I to III) [7]. Here, the authors report 3.9% worsening encountered in malignant gliomas only. It is surprising and in disagreement with classical data of the literature [7–10].
–My last comment concerns laminoplasty. It is true that, in China, many patients are poor and unable to cover the cost of screws and plates. But I wish to say that, in my practice, I have made several laminoplasties in children with very cheap silk sutures at the time we had not the small plates and screws in titanium. If we go back to the original papers from pediatric neurosurgeons, laminoplasty was made with silk sutures [11].
References
1. Brotchi J (2002) Intrinsic spinal cord tumor resection. Neurosurgery 50: 1059–1063
2. Brotchi J, Bruneau M, Lefranc F, Balériaux D (2006) Surgery of intraspinal cord tumors. Clin Neurosurg 53:209–216
3. Roonprapunt C, Silvera VM, Setton A, Freed D, Epstein FJ, Jallo GI (2001) Surgical management of isolated hemangioblastomas of the spinal cord. Neurosurgery 49:321–328
4. Anson JA, Spetzler RF (1993) Surgical resection of intramedullary spinal cord malformations. J Neurosurg 78:446–451
5. Cooper PR. (1989) Outcome after operative treatment of intramedullary spinal cord tumors in adults: intermediate and long-term results in 51 patients. Neurosurgery 25:855–859
6. Houten, JK, Cooper PR (2000) Spinal cord astrocytomas: presentation, management and outcome. J Neurooncol 47:219–224
7. McCormick PC, Torres R, Post KD, Stein BM (1990) Intramedullary ependymoma of the spinal cord. J Neurosurg 72:523–532
8. Fischer G., Brotchi J (1995) Intramedullary spinal cord tumors. Thieme, Stuttgart, 115 pp
9. Constantini S, Miller DC, Allen JC, Rorke LB, Freed D, Epstein FJ (2000) Radical excision of intramedullary spinal cord tumors: surgical morbidity and long-term follow-up evaluation in 164 children and young adults. J Neurosurg 93(2 Suppl):183–193
10. Schwartz TH, McCormick PC (2000) Intramedullary ependymomas: clinical presentation, surgical treatment strategies and prognosis. J Neuro-Oncol 47:211–218
11. Raimondi AJ, Gutteriez FA, Di Rocco C (1976) Laminotomy and total reconstruction of the posterior spinal arch in spinal canal surgery in childhood. J Neurosurg 45:555–560
All of our clinical studies were permitted by the patients and the Ethics Committee of Peking University Third Hospital.
Electronic supplementary material
Below is the link to the electronic supplementary material.
Fig4
Attached Figure 1 A 42-year-old male patient with ependymoma spanning C4–T2 segments was surgically treated. a Preoperative contrast MRI scan show the MSICT; b the whole laminas of vertebra was removed together; c the dura was opened; d after strict midline myelotomy; e the tumor was total removed; f remaining space after the tumor was taken out; g the pia mater reattached at the end of the tumor resection; h the dura was closed; i the laminoplasty was completed; j postoperative CT scan show laminoplasty; k postoperative contrast MRI scan show no tumor remained (JPEG 256 kb)
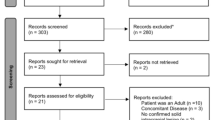
ESM 2
(JPEG 22 kb)
ESM 3
(JPEG 50 kb)
ESM 4
(JPEG 63 kb)
ESM 5
(JPEG 8 kb)
ESM 6
(JPEG 52 kb)
ESM 7
(JPEG 54 kb)
ESM 8
(JPEG 15 kb)
ESM 9
(JPEG 26 kb)
ESM 10
(JPEG 209 kb)
ESM 11
(JPEG 247 kb)
Attached Table 1
The initial symptoms ratio of adolescent patients to adult patients (DOCX 12 kb)
Attached Table 2
The detailed initial symptoms ratio of adolescent patients to adult patients (DOCX 12 kb)
Attached Table 3
The IJOA difference value grading ratio of adolescent patients to adult patients (DOCX 12 kb)
Rights and permissions
About this article
Cite this article
Wang, Zy., Sun, Jj., Xie, Jc. et al. Comparative analysis on the diagnosis and treatments of multisegment intramedullary spinal cord tumors between the different age groups. Neurosurg Rev 35, 85–93 (2012). https://doi.org/10.1007/s10143-011-0345-2
Received:
Revised:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s10143-011-0345-2