Abstract
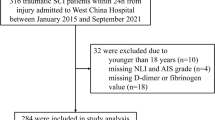
This study sought to describe and evaluate any relationship between D-dimer values and progressive hemorrhagic injury (PHI) after traumatic brain injury (TBI). In patients with TBI, plasma D-dimer was measured while a computed tomography (CT) scan was conducted as soon as the patient was admitted to the emergency department. A series of other clinical and laboratory parameters were also measured and recorded. A logistic multiple regression analysis was used to identify risk factors for PHI. A cohort of 194 patients with TBI was evaluated in this clinical study. Eighty-one (41.8%) patients suffered PHI as determined by a second CT scan. The plasma D-dimer level was higher in patients who demonstrated PHI compared with those who did not (P < 0.001. Using a receiver–operator characteristic curve to predict the possibility by measuring the D-dimer level, a value of 5.00 mg/L was considered the cutoff point, with a sensitivity of 72.8% and a specificity of 78.8%. Eight-four patients had D-dimer levels higher than the cut point value (5.0 mg/L); PHI was seen in 71.4% of these patients and in 19.1% of the other patients (P < 0.01). Factors with P < 0.2 on bivariate analysis were included in a stepwise logistic regression analysis to identify independent risk factors for TBI coagulopathy. Logistic regression analysis showed that the D-dimer value was a predictor of PHI, and the odds ratio (OR) was 1.341 with per milligram per liter (P = 0.020). The stepwise logistic regression also identified that time from injury to the first CT shorter than 2 h (OR = 2.118, P = 0.047), PLT counts lesser than 100 × 109/L (OR = 7.853, P = 0.018), and Fg lower than 2.0 g/L (OR = 3.001, P = 0.012) were risk factors for the development of PHI. When D-dimer values were dichotomized at 5 mg/L, time from injury to the first CT scan was no longer a risk factor statistically while the OR value of D-dimer to the occurrence of PHI elevated to 11.850(P < 0.001). The level of plasma D-dimer after TBI can be a useful prognostic factor for PHI and should be considered in the clinical management of patients in combination with neuroimaging and other data.

Similar content being viewed by others
References
Association for the Advancement of Automotive Medicine (1990) The Abbreviated Injury Scale, 1990 Revision. Association for the Advancement of Automotive Medicine, Des Plaines, IL
Barber M, Langhorne P, Rumley A, Lowe GD, Stott DJ (2004) Hemostatic function and progressing ischemic stroke: D-dimer predicts early clinical progression. Stroke 35:1421–1425
Bullock R, Chesnut RM, Clifton G, Ghajar J, Marion DW, Narayan RK (1996) Guidelines for the management of severe head injury. Brain Trauma Foundation. Eur J Emerg Med 3:109–127
Carrick MM, Tyroch AH, Youens CA, Handley T (2005) Subsequent development of thrombocytopenia and coagulopathy in moderate and severe head injury: support for serial laboratory examination. J Trauma 58:725–730
Chao A, Pearl J, Perdue P, Wang D, Bridgemann A, Kennedy S et al (2001) Utility of routine serial computed tomography for blunt intracranial injury. J Trauma Inj Infect Crit Care 51:870–876
Delgado P, Alvarez-Sabin J, Abilleira S, Santamarina E, Purroy F, Arenillas JF et al (2006) Plasma D-dimer predicts poor outcome after acute intracerebral hemorrhage. Neurology 67:94–98
Engstrom M, Romner B, Schalén W, Reinstrup P (2005) Thrombocytopenia predicts progressive hemorrhage after head trauma. J Neurotrauma 22:291–296
Juvela S, Siironen J (2006) D-dimer as an independent predictor for poor outcome after aneurysmal subarachnoid hemorrhage. Stroke 7:1451–1456
Kaups KL, Davis JW, Parks SN (2004) Routinely repeated computed tomography after blunt head trauma: does it benefit patients? J Trauma Inj Infect Crit Care 56:475–481
Khotari RU, Brott T, Broderick JP, Barsan WG, Sauerbeck LR, Zuccarello M et al (1996) The ABCs of measuring intracerebral hemorrhage volume. Stroke 27:1304–1305
Kuo JR, Chou TJ, Chio CC (2004) Coagulopathy as a parameter to predict the outcome in head injury patients—analysis of 61 cases. J Clin Neurosci 11:710–714
Kuo JR, Lin KC, Luc L, Lin HJ, Wang CC, Chang CH (2007) Correlation of a high D-dimer level with poor outcome in traumatic intracranial hemorrhage. Eur J Neurol 14:1073–1078
Lee K, Kawai N, Kim S, Sagher O, Hoff JT (1997) Mechanisms of edema formation after intracerebral hemorrhage: effects on thrombin on cerebral blood flow, blood-brain barrier permeability, and cell survival in a rat model. J Neurosurg 86:272–278
Levi M, Ten CH (1999) Disseminated intravascular coagulation. N Engl J Med 341:586–592
Lobato RD, Sarabia R, Cordobes F (1988) Posttraumatic cerebral hemispheric swelling. Analysis of 55 cases studied with computerized tomography. J Neurosurg 68:417–423
Mirvis SE, Wolf AL, Numaguchi Y (1990) Posttraumatic cerebral infarction diagnosed by CT: prevalence, origin, and outcome. Am J Roentgenol 154:1293–1298
Oertel M, Kelly DF, Mcarthur D, Boscardin WJ, Glenn TC, Lee JH et al (2002) Progressive hemorrhage after head trauma: predictors and consequences of the evolving injury. J Neurosurg 96:109–116
Rathbun SW, Whitsett TL, Vesely SK, Raskob GE (2004) Clinical utility of D-dimer in patients with suspected pulmonary embolism and nondiagnostic lung scans or negative CT findings. Chest 125:851–855
Robson SC, Shepard EG, Kirsch RE (1994) Fibrin degradation products D-dimer induces the synthesis and release of biologically active IL-1B, IL-6 and plasminogen activator inhibitors from monocytes in vitro. Br J Haematol 86:322–326
Rutland-Brown W, Langlois JA, Thomas KE, Xi YL (2006) Incidence of traumatic brain injury in the United States. J Head Trauma Rehabil 21:544–548
Sanus GZ, Taner T, Ilker A, Sabri A, Mustafa U (2004) Evolving traumatic brain lesions: predictors and results of ninety-eight head-injured patients. Neurosurg Q 14:97–104
Servadei F, Nanni A, Nasi MT, Zappi D, Vergoni G, Giuliani G et al (1995) Evolving brain lesions in the first 12 hours after head injury: analysis of 37 comatose patients. Neurosurgery 37:899–907
Stein DM, Dutton RP, Kramer ME, Scalea TM (2009) Reversal of coagulopathy in critically ill patients with traumatic brain injury: recombinant factor VIIa is more cost-effective than plasma. J Trauma 66:63–72, discussion 73-5
Stein SC, Spettell C, Young G, Ross SE (1993) Delayed and progressive brain injury in closed-head trauma: radiological demonstration. Neurosurgery 32:25–31
Stein SC, Young GS, Talucci RC, Greenbaum BH, Ross SE (1992) Delayed brain injury after head trauma: significance of coagulopathy. Neurosurgery 30:160–165
Tagliaferri F, Compagnone C, Korsic M, Servadei F, Kraus J (2006) A systematic review of brain injury epidemiology in Europe. Acta Neurochir 148:255–267
Talving P, Benfield R, Hadjizacharia P, Inaba K, Chan LS, Demetriades D et al (2008) Coagulopathy in severe traumatic brain injury: a prospective study. J Trauma 66:55–61, discussion 61-62
Tian HL, Geng Z, Cui YH, Hu J, Xu T, Cao HL et al (2008) Risk factors for posttraumatic cerebral infarction in patients with moderate or severe head trauma. Neurosurg Rev 31:431–437
Wells PS, Anderson DR, Rodger M, Forgie M, Kearon C, Dreyer J et al (2003) Evaluation of D-dimer in the diagnosis of suspected deep-vein thrombosis. N Engl J Med 349:1227–1235
Williams MT, Aravindan N, Wallace MJ, Riedel BJ, Shaw AD (2003) Venous thromboembolism in the intensive care unit. Crit Care Clin 19:185–207
Zaaroor M, Soustiel JF, Brenner B, Bar-Lavie Y, Martinowitz U, Levi L (2008) Administration off label of recombinant factor-VIIa (rFVIIa) to patients with blunt or penetrating brain injury without coagulopathy. Acta Neurochir (Wien) 150:663–668, Epub 2008 May 12
Author information
Authors and Affiliations
Corresponding author
Additional information
Comments
Jorge Humberto Tapia-Pérez, Magdeburg, Germany
In this study, the authors tried to explain the role of D-dimer as predictor for progression of hemorrhagic injury (PHI) in trauma patients. The sufficient number of patients could have been shown more detail; nevertheless, with the given data, many interesting conclusions are obtained. The patients with PHI displayed more frequent abnormalities in coagulation parameters; based on these observations, it could be expressed that a kind of coagulopathy is associated. Pathophysiologic considerations allow us, assuming that inflammation and endothelial injury are contributing. Recently, a study from Canada showed that coagulation abnormalities detected in routine laboratory tests in the first hours are predictors of hemorrhagic progression [1]. This study provides support to this observation. The causal relationship between coagulopathy and progression will require further studies.
The relevance as therapeutic target has been described by Narayan et al. [2] in their study about factor VIIa. A consideration is that the delay or limitation of PHI could not redound in a clinical improvement, despite the association of bad outcome described by Tian et al. In this way, targeting traumatic coagulopathy could be just an additional therapy, if the future studies do not demonstrate an increased risk of thrombotic events.
The first regression model presented showed the time to first CT scan as risk factor for PHI, but it should not necessarily be considered as that. An early CT scan could not detect lesions because some of them do not develop yet. It is probably an evidence of a natural PHI after trauma, which is linked to coagulation disorders; further studies are needed.
The authors' conclusion provides us an easy clinical tool. Reasonably, in patients with severe head injury, admitted early, and with abnormalities in coagulation (especially DD) can the performance of a CT scan be very useful. Evidently, the therapeutic decision must be taken in context of each case.
References
1. Allard CB, Scarpelini S, Rhind SG, Baker AJ, Shek PN, Tien H, Fernando M, Tremblay L, Morrison LJ, Pinto R, Rizoli SB. Abnormal coagulation tests are associated with progression of traumatic intracranial hemorrhage. J Trauma 2009;67:959–967.
2. Narayan RK, Maas AI, Marshall LF, Servadei F, Skolnick BE, Tillinger MN; rFVIIa Traumatic ICH Study Group. Recombinant factor VIIA in traumatic intracerebral hemorrhage: results of a dose-escalation clinical trial. Neurosurgery 2008 ;62:776–778.
Ignacio J. Previgliano, Buenos Aires, Argentina
This paper by Tian et al. is very interesting in addressing the issue of bleeding disorders following head injury.
Although based on retrospective data, their finding that D-dimer at a cutoff point of 5 mg/l with a sensitivity of 72.8% and a specificity of 78.8% is an important clue for further investigation.
The authors gave substantial bibliographic support for the use of D-dimer as a prognostic toll of progressive hemorrhagic injury in patients with traumatic brain injury. Most of their findings showed that patients with D-dimer above 5 mg/l were older and had a severe head injury according to the initial GCS, so they underwent early to diagnostic studies. They also pointed out in the paper that D-dimer is augmented in many acute neurological disorders mainly to the activation of the coagulation process due to the liberation of tissue factor.
Nevertheless, some important points should be highlighted:
(a) In the logistic regression model, only patients with determinations above the cutoff point were included.
(b) It was not possible to identify the exact coagulation problem in most of the study population.
(c) Regarding this dilution, coagulopathy and disseminated intravascular coagulation (DIC) diagnosis should be ruled out for the reason that a different therapeutic approach is needed.
The International Society on Thrombosis and Haemostasis developed a simple scoring system for the diagnosis of overt DIC (see Table 1). A score of 5 or greater indicates overt DIC, whereas a score of less than 5 does not rule out DIC, but may indicate non-overt DIC. Studies have demonstrated the DIC score to be 93% sensitive and 98% specific for DIC.

Table 1. DIC scoring system. Modify from Taylor Jr FB, Thromb Haemost 2001;86:1327–1330.
I think this is a good tool for the neurosurgeon to confront acute bleeding disorders in head injury patients.
As stated above, this paper is a good starting point for further research in such important issue as the prognosis of delayed hematomas.
Susanne Mink, Zurich, Switzerland
It still remains challenging to find outcome predictors for progression of acute hemorrhagic injury (PHI) of traumatic brain-injured patients. In this comprehensive article, the authors summarize their experience with D-dimer levels in nearly 200 patients with traumatic brain injury. The results and conclusion of the study are very interesting and may be one part of the facts for clinical judgement and therapeutic decisions in the acute state of injury. A relevant limitation of the study represents the retrospective character. However, more detailed and additional information should be addressed in further prospective studies. Thereby, subgroup analysis and enhanced CT time management would be of interest in these cases. Early CT scans can miss lesions which are not developed at the time of examination. This leads to the necessity for definition of exact time intervals of D-dimer plasma levels and further coagulation parameters. Sawamura et al. (1) described the parameters of disseminated intravascular coagulation in general traumatic patients in more detail, considering, additionally, ratios to be more specific and significant in outcome prediction. Generally, contributing factors in PHI are endothelial damage and associated inflammation which seek still for causal relationship between coagulopathy and the PHI.
Reference
1. Sawamura A, Hayakawa M, Gando S, et al. Disseminated intravascular coagulation with a fibrinolytic phenotype at an early phase of trauma predicts mortality. Thromb Res 2009;124:608–613.
Rights and permissions
About this article
Cite this article
Tian, HL., Chen, H., Wu, BS. et al. D-dimer as a predictor of progressive hemorrhagic injury in patients with traumatic brain injury: analysis of 194 cases. Neurosurg Rev 33, 359–366 (2010). https://doi.org/10.1007/s10143-010-0251-z
Received:
Revised:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s10143-010-0251-z