Abstract
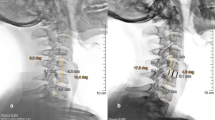
In ventral fusion after anterior cervical discectomy there is still a remarkable number of cage subsidence and segmental kyphosis seen. The aim of the present study is to assess whether the cage design influences the extent of correction loss during follow-up. Sixty patients with single-level cervical disc herniation were randomly treated with two different cervical inter-body cages (group1: Solis™ cage, Stryker Company and group2: Shell™ cage, AMT Company). Clinical and radiological follow-up was done before and after surgery, 3 and 6 months post-surgery. Clinical follow-up was done with the help of Odom’s criteria. Both groups were similar in the baseline parameters (age, sex, treated level). Statistically, the subsidence was significantly higher at 3 and 6-month follow-ups in group1 than in group2, however, clinical results showed no significant differences. In 67%, subsidence was seen in the anterior lower aspect of the treated segment. Segmental kyphosis was seen in seven patients of group1 and two patients of group2. A significant correlation is found between Odom’s criteria and subsidence. Although there was no significant difference in a short-term clinical result between the two treatment groups, we recommend the use of cages which preserve the determined segmental height and lordosis.




Similar content being viewed by others
References
Barlocher CB, Barth A, Krauss JK, Binggeli R, Seiler RW (2002) Comparative evaluation of microdiscectomy only, autograft fusion, polymethylmethacrylate interposition, and threaded titanium cage fusion for treatment of single-level cervical disc disease: a prospective randomized study in 125 patients. Neurosurg Focus 12(1):E4
Bertalanffy H, Eggert HR (1988) Clinical long-term results of anterior discectomy without fusion for treatment of cervical radiculopathy and myelopathy. A follow-up of 164 cases. Acta Neurochir 90:127–135
Bruneau M, Nisolle JF, Gilliard C, Gustin T (2001) Anterior cervical interbody fusion with hydroxyapatite graft and plate system. Neurosurg Focus 10(4):E8
Cloward RB (1958) The anterior approach for removal of ruptured cervical discs. J Neurosurg 15:602–617
Frederic S, Benedict R, Payer M (2006) Implantation of an empty carbon fiber cage or a tricortical iliac crest autograft after cervical discectomy for single-level disc herniation: a prospective comparative study. J Neurosurg Spine 4:292–299
Haden N, Latimer M, Seeley HM, Laing RJ (2005) Loss of inter-vertebral disc height after anterior cervical discectomy. Br J Neurosurg 19:469–474
Hamburger C, Festenberg FV, Uhl E (2001) Ventral discectomy with PMMA interbody fusion for cervical disc disease: long-term results in 249 patients. Spine 26:249–255
Heary RF, Schlenk RP, Sacchieri TA, Barone D, Brotea C (2002) Persistent iliac crest donor site pain: independent outcome assessment. Neurosurgery 50:510–517
Katsuura A, Hukuda S, Saruhashi Y, Mori K (2001) Kyphotic malalignment after anterior cervical fusion is one of the factors promoting the degenerative process in adjacent intervertebral levels. Eur Spine J 10:320–324
Kemmesies D, Meier U (2005) Experience with five different intervertebral disc spacers for cervical spondylodesis. Zentralbl Neurochir 66:24–33
Kwon B, Kim DH, Marvin A, Jenis LG (2005) Outcomes following anterior cervical discectomy and fusion: the role of interbody disc height, angulation, and spinous process distance. J Spinal Disord Tech 18:304–308
Laing RJ, Ng I, Seeley HM, Hutchinson PJ (2001) Prospective study of clinical and radiological outcome after anterior cervical discectomy. Br J Neurosurg 15:319–323
Mastronardi L, Ducati A, Ferrante L (2006) Anterior cervical fusion with polyetheretherketone (PEEK) cages in the treatment of degenerative disc disease. Preliminary observations in 36 consecutive cases with a minimum 12-month follow-up. Acta Neurochir 148:307–312
Meier U, Kemmesies D (2004) [Experiences with six different intervertebral disc spacers for spondylodesis of the cervical spine]. Orthopade 33:1290–1299 (German)
Odom GL, Finney W, Woodhall B (1958) Cervical disc lesions. JAMA 166:23–28
Peolsson A, Hedlund R, Vavruch L, Oberg B (2003) Predictive factors for the outcome of anterior cervical decompression and fusion. Eur Spine J 12:274–280
Ryu SI, Mitchell M, Kim DH (2006) A prospective randomized study comparing a cervical carbon fiber cage to the Smith–Robinson technique with allograft and plating: up to 24 months follow-up. Eur Spine J 15:157–164
Schmieder K, Wolzik-Grossmann M, Pechlivanis I, Engelhardt M, Scholz M, Harders A (2006) Subsidence of the wing titanium cage after anterior cervical interbody fusion: 2-year follow-up study. J Neurosurg Spine 4:447–453
Shad A, Leach JC, Teddy PJ, Cadoux-Hudson TA (2005) Use of the Solis cage and local autologous bone graft for anterior cervical discectomy and fusion: early technical experience. J Neurosurg Spine 2:116–122
Siddiqui AA, Jackowski A (2003) Cage versus tricortical graft for cervical interbody fusion. A prospective randomised study. J Bone Joint Surg Br 85:1019–1025
Silber JS, Anderson DG, Daffner SD, Brislin BT, Leland JM, Hilibrand AS et al (2003) Donor site morbidity after anterior iliac crest bone harvest for single-level anterior cervical discectomy and fusion. Spine 28:134–139
Smith AW, Robinson RA (1958) The treatment of certain spine disorders by anterior removal of the intervertebral disc and interbody fusion. J Bone Joint Surg Am 40:607–624
Singh A, Crockard HA (2001) Comparison of seven different scales used to quantify severity of cervical spondylotic myelopathy and post-operative improvement. J Outcome Meas 5:798–818
Tureyen K (2003) Disc height loss after anterior cervical microdiscectomy with titanium intervertebral cage fusion. Acta Neurochir 145:565–569
van Jonbergen HP, Spruit M, Anderson PG, Pavlov PW (2005) Anterior cervical interbody fusion with a titanium box cage: early radiological assessment of fusion and subsidence. Spine J 5:645–649
Vavruch L, Hedlund R, Javid D, Leszniewski W, Shalabi A (2002) A prospective randomized comparison between the cloward procedure and a carbon fiber cage in the cervical spine: a clinical and radiologic study. Spine 27:1694–701
Author information
Authors and Affiliations
Corresponding author
Additional information
Comments
Peter Ulrich, Offenbach, Germany
The authors deal in their prospective study with a typical complication of anterior cervical discectomy, the loss of disc height and increasing kyphosis. Despite recent advances in spacer technology, the problem is far from being solved. Furthermore, the variety of solutions extolled by the industry makes it more difficult to make the right choice. The purpose of the study was to evaluate, in a randomized controlled protocol, whether the cage design influences the extent of correction loss and the clinical results. At 6 months after mono-segmental discectomy, the cage with the greater contact surface area increased at the anterior lower aspect (Shell™ cage, AMT Company, Nonnweiler, Germany) yielded significantly better results in the radiologic outcome than its counterpart (Solis™ cage, Stryker Company, Kalamazoo, USA). The correlation between radiologic criteria and clinic was less compelling. The authors present an innovative method of measuring segmental height, which seems quite valuable. The conclusion that a careful choice of the proper cage is crucial for obtaining good radiological and clinical results confirms a widespread experience. Despite a limited number of patients enrolled in the study and a relatively short follow-up, the paper presents a remarkable contribution to the ongoing discussion about the best technique in ventral fusion after anterior cervical discectomy.
Hiroshi Nakagawa, Nagoya, Japan
This is a randomized prospective clinical study on subsidence following anterior cervical inter-body fusion using two different cages made of PEEK.
It demonstrated a well-analyzed data which recommended usage of cages with a large-enough contact surface area to preserve the segmental height and lordosis, although this study is of limited value because of a relatively small number of cases, rather short follow-ups, and no CT follow-ups.
For the last decade, we have had some experience of more than 400 cases with cervical myelopathy and radiculopathy which were treated by anterior inter-body cage fixation using cyrindrical titanium cages. In cervical discs and spondylosis, two cages were inserted side by side in a locked fashion and with the anterior cage surface placed along the anterior cortex of the vertebrae in order to minimize the subsidence of the cages.
One thing I can not understand is that the authors used anterior plating in addition to inter-body cages in cases with cervical myelopathy. Is there any rationale for this? In our series, about 70% of the cases have myelopathy and have been treated mostly by cages only without much problem.
With more experience and cases, I hope they will come up with a lesser invasive method in the future.
Disclaimer
None of the authors has received any financial support from any company cited in this study, and none of the authors has any financial or other interest in a company involved in this study.
Rights and permissions
About this article
Cite this article
Kast, E., Derakhshani, S., Bothmann, M. et al. Subsidence after anterior cervical inter-body fusion. A randomized prospective clinical trial. Neurosurg Rev 32, 207–214 (2009). https://doi.org/10.1007/s10143-008-0168-y
Received:
Revised:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s10143-008-0168-y