Abstract
Background
Cervical disc herniation is a common cause of neck, upper limb, and upper back pain. In severe cases, neurological deficit might occur. It is surgically treated anteriorly or posteriorly, anteriorly through both cervical discectomy and fusion (ACDF) using cages alone or using cages plus plating.
Objectives
We aimed to evaluate the fusion rate and the clinical outcome of multiple level anterior cervical discectomy followed by cage fusion alone and cage fusion with plate insertion.
Materials and methods
In this prospective comparative study, 33 patients were included. Patients were divided into 2 groups: group A: 19 cases received ACDF and group B: 14 patients had ACDF plus plate fixation. Fusion rate was assessed by radiographs. Clinical outcome was assessed by the visual analog scale (VAS). Overall patients’ satisfaction postoperatively was graded according to Odom’s criteria.
Results
The rate of fusion was 78.9% of patients in group A and 85.7% of patients in group B. Clinical outcomes were similar in both groups. Patient satisfaction according to Odom’s criteria of outcome grading showed 36.8% of patients had excellent recovery and 31.6% had good recovery in group A. While in group B, 42.9% of patients had excellent recovery and 21.4% had good recovery. The differences between both groups were not statistically significant (P = 0.19).
Conclusions
ACDF with or without plate fixation in more than two-level cervical discectomies achieves good stability and functional outcome. Addition of anterior cervical plate fixation resulted in a higher fusion rate and reduced cage subsidence than that of cage alone.
Similar content being viewed by others
Introduction
Cervical disc herniation is commonly treated by anterior cervical discectomy and fusion (ACDF) if conservative treatment has failed. Cervical intervertebral disc replacement with cage achieves immediate load bearing support to the anterior column, restoration of disc height, and foraminal decompression and facilitates interbody fusion [1, 2].
Anterior ligamentous structures are absent after ACDF with interbody fusion. That applies little stabilization during extension. The stand-alone cage is less invasive and had less donor-site morbidity [3].
The most frequent complication of ACDF using cage is the cage subsidence. Postoperative cage subsidence may occur along the follow-up period leading to subsequent foraminal stenosis. Patients may show recurrence of radiculopathy and axial neck pain after surgery [4]. On the other hand, radiological evidence of cage subsidence does not necessarily lead to recurrence of radiculopathy in other patients.
We reviewed the two techniques, ACDF with cage alone or with cage and plate, for patients suffering from more than two levels cervical disc herniation. Our aim is to evaluate the fusion rate and the clinical outcome of both techniques.
Materials and methods
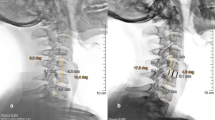
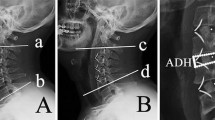
The study was conducted prospectively on 33 patients suffering from more than 2 levels cervical degenerative disc disease who were unresponsive to adequate conservative therapy. They were all treated at the Neurosurgery Department, in the period from 2012 to 2016. Patients were selected from the outpatient clinic of our hospital. The procedures we followed were in accordance with the ethical standards of the responsible committee on human experimentation and with the Helsinki Declaration principles. Informed consent was obtained from all participants, and we obtained permission from the ethical committee in our institution before starting our study. Exclusion criteria were as follows: patients with 2 levels or less cervical degenerative disc disease, past cervical disc surgery patients, and cases responsive to adequate conservative therapy. All patients in this study were subjected to history taking and complete general and neurological examination. Patients were divided into 2 groups. In group A, 19 cases received ACDF with peek interbody cage packed with allograft and synthetic bone graft, 11 were males and 8 females, and the mean age of patients was 54.6 years (range 39 to 76 years). In group B, there were 14 patients, 8 were males and 6 females, and the average age of patients was 52.2 years (range 43 to 68 years). They were treated with anterior cervical cage and plate fixation (Figs. 1 and 2).
Before surgery and at each follow-up, both neck pain and shoulder (radicular) pain were assessed with a 10-point visual analog scale (VAS) with words that convey “no pain” at one end and “worst pain” at the opposite end. The patient’s subjective perception of overall satisfaction with the outcome of the procedure was graded according to Odom’s criteria as excellent, good, fair, or poor as shown in Table 1.
Statistical analysis
Statistical analysis was done using IBM SPSS statistics version 20. IBM Corp. Armonk, NY, USA. Data were presented as mean ± standard deviation, frequencies, and range. All the numerical data were analyzed by analysis of variance (ANOVA). Non-numerical data were analyzed using chi-square or Fischer exact test as appropriate. A probability value (P value) less than 0.05 was considered statistically significant.
Results
In group A, there were 14 patients who underwent 3-level discectomies and 5 patients who underwent 4-level discectomies. In group B, 10 patients underwent 3-level discectomies while the remaining 4 patients underwent 4-level discectomies as shown in Table 2. Frequency of preoperative neurological symptoms and signs among both study groups is shown in Fig. 3 and the postoperative improvement in Fig. 4.
Postoperative clinical assessment was done immediately postoperatively and during patient’s stay in the hospital (average 7 days). Patients were followed up at 1, 3, 6, 12 months after discharge.
The mean postoperative VAS pain scores for neck pain showed improvement compared to the preoperative scores. There was a statistically significant relief of cervical pain after surgery in both groups (P = 0.02 and 0.01 respectively) but no significant difference between the two groups (P = 0.64). There was a statistically significant relief of brachialgia after surgery in both groups (P < 0.01 in both groups). Patient’s clinical outcome is given in Table 3.
Improvement in motor power was more gradual than pain improvement and in most cases occurred within the first 3 months. Following surgery, the numbness improved in nine (72.7%) of group A patients and in five (71.4%) of group B patients within the first 2 days after surgery while it did not improve in two (27.3%) of group A patients and in two (28.6%) of group B patients.
Patient satisfaction was assessed using Odom’s criteria of outcome grading; in group A, seven patients (36.8%) had excellent recovery, six patients (31.6%) had good recovery, three patients (15.8%) had fair recovery, and three patients (15.8%) had poor recovery. In group B, six patients (42.9%) had excellent recovery, three patients (21.4%) had good recovery, two patients (14.3%) had fair recovery, and three patients (21.4%) had poor recovery. The differences between both groups were not statistically significant (P = 0.19). Patient satisfaction among both groups is shown in Fig. 5.
At 1-year follow-up examination, the fusion was observed radiologically in both groups through detection of presence of trabecular bone across the interfaces without lucencies between the cage and vertebral endplates, also through lack of motion in the postoperative dynamic X-rays. The rate of fusion was 78.9% (15/19 patients) in group A and 85.7% (12/14 patients) in group B, and this difference was statistically insignificant (P > 0.05). Complications reported in our study were transient dysphagia and transient hoarseness which improved overtime. Infection, hematoma, dural tear, and spinal cord injury occurred in one case each and treated conservatively. Cage subsidence was reported in seven cases with no nerve root compression symptoms which did not require any further management. Loosening of a screw and pseudoarthrosis were managed by maintaining the neck collar for at least 6 weeks and conservative treatment. Complications among both groups are shown in Table 4.
Discussion
Interbody fusion cages were developed as a stand-alone device to augment arthrodesis via the anterior approach. Their introduction caused resurgence in interbody fusion for degenerative disorders. Cages have demonstrated their ability to function as load-sharing devices and to adequately fixate the spine and increase segmental stiffness thus achieves acceptable fusion rates [5].
Some surgeons have reported poor outcomes and fusion rates secondary to a high rate of cage subsidence and pseudoarthrosis. They believed that this phenomenon occurred as a result of insufficient fixation power of cage alone. Allowing postoperative micro-motions to continuously occur between the contact surfaces of the cage and vertebra, these continuous micro-motions prevent the induction of bone fusion [6]. Internal fixation using anterior cervical plate (ACP) has been developed in order to enhance the stability provided by the intervertebral cages, to help prevent graft dislodgement, and ultimately to promote mature bony fusion of the spinal segment. Some authors reported lesser graft dislocations or collapse and higher fusion rates after ACDF with internal fixation compared with ACDF alone [7].
In postoperative results in our study, there was a statistically significant relief of cervical pain after surgery in both groups (P < 0.05) but no significant difference between the two groups (P = 0.64). In Hwang and colleagues [8] series, he showed similar results in both groups.
In our study, brachialgia was significantly improved after surgery in both groups (P < 0.01 in both groups). In Liu and colleagues [9] series, the mean post-operative VAS arm pain score was significantly improved compared with preoperative score.
We assessed patient satisfaction using Odom’s criteria of outcome grading. In group A, 36.8% of patients had excellent recovery, 31.6% had good recovery, 15.8% had fair recovery, and 15.8% had poor recovery. In group B, 42.9% had excellent recovery, 21.4% had good recovery, 2 patients 14.3% had fair recovery, and 21.4% of patients had poor recovery.
In Uribe and colleagues [10] series, 83.3% of patients had excellent recovery, 14.3% had good recovery, 2.34% had fair recovery, and no patients had poor recovery among 42 non-plated patients. In the study by Wang and colleagues [7], 28.1% had excellent recovery, 50.9% had good recovery, 15.8% had fair recovery, and 5.2% of patients had poor recovery among 57 plated patients.
At 1-year follow-up examination, we achieved 78.9% fusion rate in group A and 85.7% in group B. In Hwang and colleagues [8] series, the rate of fusion at 1-year follow-up was 90.6% in 32 non-plated patients and 91.7% in 24 plated patients. Criteria of fusion included detection of presence of bone formation between the cage and vertebral endplates, also through lack of motion in the postoperative dynamic X-rays.
Cervical plate fixation, however, is not free from complications and morbidity. Significantly higher complication rate was reported in patients managed by anterior cervical plate than patients managed by interbody fusion cages alone. After surgery, we reported adverse effects such as transient dysphagia which was the most common complication. It occurred in 10 (52.6%) of group A patients and in 12 (85.7%) of group B patients. Dysphagia was probably more accentuated in group B patients due to longer duration of surgery and traction on the esophagus. Dysphagia was mild in all these patients and lasted only for few days. Dogan and colleagues [11] mentioned in his series that transient dysphagia occurred in 5 (22.7%) of 22 non-plated patients while Song and colleagues [12] reported dysphagia in 4 (9.3%) of 43 plated patients.
In our study, transient hoarseness of voice occurred in two (10.5%) of group A patients and in four (28.6%) of group B patients. The hoarseness lasted only for few days in all cases and resolved spontaneously. Cage subsidence occurred in five (26.3%) of group A patients and in two (14.3%) of group B patients in this study. Subsidence was referred to loss of height as ≥ 3 mm of the direct postoperative intervertebral height compared to the intervertebral one or presence of pseudoarthrosis at the follow-up radiographs. In all these patients, the subsidence occurred within the first 3 months but no further progression was demonstrated on follow-up radiographs 12 months after surgery and the subsidence did not produce any symptoms in these cases without recurring nerve root compression and required no further management. In other series, rate of subsidence was 32.3% in the stand-alone cage group as compared to 9.7% in the cage and plate group [13].
In Erol and colleagues [14] cohorts, subsidence of cages was measured by any decrease in the disc space narrowing of at least 3 mm. They assumed that subsidence in cervical stand-alone interbody cage fusion is a major problem and additional stabilization is necessary to avoid this problem [15]. Thus due to cage subsidence, the foraminal height decrease, loss of segmental lordosis, and cervical spine instability can lead to adjacent segment degeneration [16].
To minimize the risk of subsidence, the surgeon should avoid aggressive removal of the bony end-plate; the best is to remove parts of the end plate to promote fusion and to leave other parts intact to minimize subsidence. Proper size of the cage should be used as a larger cage size will increase the possibility of subsidence. Also, avoidance of overdistraction and forceful implantation reduces the risk of subsidence [17].
In our study, 2 patients (14.3%) in group B developed instrumentation failure in the form of loosening of a plate and screw with no clinical problems or neurological complications and were managed conservatively. There were no cases of plate or screw fracture. This coincides with the results of Song and colleagues [18] series in which 3 (14.3%) of 21 patients developed instrumentation failure in the form of loosening of a plate and screw.
Conclusions
We conclude that addition of anterior cervical plate fixation to interbody cage-based fusion resulted in a lower rate of cage subsidence and a higher fusion rate than non-plated patients at 1 year follow-up examination. However, the difference between both groups was not statistically significant.
Abbreviations
- ACDF:
-
Anterior cervical discectomy and fusion
- ACP:
-
Anterior cervical plate
- MRI:
-
Magnetic resonance imaging
- VAS:
-
Visual analog scale
References
Dunn RN, Pretorius C. Cervical PEEK cage standalone fusion–the issue of subsidence. SA Orthop J. 2011;10(1):25–9.
Oh J, Kim T, Lee H, You N, Choi G, Yi S, et al. Stand-alone cervical cages versus anterior cervical plate in 2-level cervical anterior interbody fusion patients: clinical outcomes and radiologic changes. J Spinal Disorder Tech. 2013;26(8):415–20.
Shunsuke F, Masashi N, Takashi N. Stand-alone interbody cage versus anterior cervical plate for treatment of cervical disc herniation: sequential changes in cage subsidence. J Clin Neurosci. 2008;15:1017–22.
Vavruch L, Hedlung R, Javid D, Leszniewski W, Shalabi A. A prospective randomized comparison between the Cloward procedure and a carbon fiber cage in the cervical spine: a clinical and radiologic study. Spine. 2002;27:1694–701.
Avadhani A, Rajasekaran S, Shetty AP. Comparison of prognostic value of different MRI classifications of signal intensity change in cervical spondyltoic myelopathy. Spine. 2010;10(6):475–85.
Joo Y, Lee J, Kwon K, Rhee J, Lee H. Comparison of fusion with cage alone and plate instrumentation in two-level cervical degenerative disease. J Korean Neurosurg Soc. 2010;48(4):342–6.
Wang J, McDonough PW, Kanim LE. Increased fusion rates with cervical plating for three-level anterior cervical discectomy and fusion. Spine. 2001;26:643–6.
Hwang S, Lin C, Lieu A, Lee K, Kuo T, Hwang Y, et al. Three-level and four-level anterior cervical discectomies and titanium cage-augmented fusion with and without plate fixation. J Neurosurg (Spine 1). 2004;2:160–7.
Liu H, Ploumis A, Li C, Yi X, Li LH. Polyetheretherketone cages alone with allograft for three-level anterior cervical fusion. ISRN Neurol. 2012;2012:1–5.
Uribe J, Sangala J, Duckworth E, Vale F. Comparison between anterior cervical discectomy fusion and cervical corpectomy fusion using titanium cages for reconstruction, analysis of outcome and long-term follow-up. Eur Spine J. 2009;18:654–62.
Dogan S, Turkkan A, Kocaeli H, Korfali E, Bekar A. Clinical and radiologic analysis of 3-level anterior cervical discectomy and fusion with interbody cages without plate fixation. Neurosurgery. 2008;18(3):188–94.
Song J, Yoon J, Lee B. Three and four-level anterior cervical discectomy and fusion with a PEEK cage and plate construct. Eur Spine J. 2012;10:1007–10.
Khaled S, Hazem M. A comparative study of ACD with peek stand alone cervical cages versus cage and plate fixation, study of 100 patients. World Spinal Column J. 2012;3:1–6.
Erol G, Vincent A, Josee D, Dante M. Subsidence of stand-alone cervical cages in anterior interbody fusion: warning. Eur Spine J. 2003;12:513–6.
Shimamoto N, Cunningham BW, Dmitriev AE, Minami A, McAfee P. Biomechanical evaluation of stand-alone interbody fusion cages in the cervical spine. Spine. 2001;26:432–6.
Yang J, Hun Yu C, Chang B, Yeom J, Lee J, Lee C. Subsidence and nonunion after anterior cervical interbody fusion using a stand-alone polyetheretherketone (PEEK) cage. Clin Orthop Surg. 2011;3:16–23.
Green C, Butler J, Eustace S, Poynton A, O’Byrne M. Imaging modalities for cervical spondylotic stenosis and myelopathy. Adv Orhop. 2011;20:1–5.
Song K, Taghavi C, Hsu M, Lee K, Kim G, Song J. Plate augmentation in anterior cervical discectomy and fusion with cage for degenerative cervical spinal disorders. Eur Spine J. 2010;19:1677–83.
Acknowledgements
Not applicable
Funding
No funding was obtained.
Availability of data and materials
The datasets used and/or analyzed during the current study are available from the corresponding author on reasonable request. E-mail of the corresponding author (drahmed73@gmail.com).
Author information
Authors and Affiliations
Contributions
AE performed the design of the study, wrote the manuscript, and participated in the clinical work and surgical intervention of the patients included in this study. SS had done the statistical analysis, analyzed and interpreted the data, and had a clinical role in the study. All authors were involved in revising the article for important intellectual content, and all authors approved the final version to be published.
Corresponding author
Ethics declarations
Ethics approval and consent to participate
-The name of the ethics committee that approved this study: Neurosurgery ethical review committee, Faculty of Medicine, Cairo University
-the committee’s date: 25 July 2012
All participants had signed a written consent to participate in the study after explaining the details, benefits as well as risks to them.
Consent for publication
Not applicable
Competing interests
The authors declare that they have no competing interests.
Publisher’s Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Rights and permissions
Open Access This article is distributed under the terms of the Creative Commons Attribution 4.0 International License (http://creativecommons.org/licenses/by/4.0/), which permits unrestricted use, distribution, and reproduction in any medium, provided you give appropriate credit to the original author(s) and the source, provide a link to the Creative Commons license, and indicate if changes were made.
About this article
Cite this article
Elsayed, A., Sakr, S. Fixation of multiple level anterior cervical disc using cages versus cages and plating. Egypt J Neurol Psychiatry Neurosurg 55, 12 (2019). https://doi.org/10.1186/s41983-019-0062-2
Received:
Accepted:
Published:
DOI: https://doi.org/10.1186/s41983-019-0062-2