Abstract
The purpose of this study is to emphasize the imaging features of complications of gallstones beyond the cystic duct on ultrasound (US), enhanced and nonenhanced computed tomography (CECT and NECT), magnetic resonance imaging (MRI), magnetic resonance cholangiopancreatography (MRCP), and endoscopic retrograde cholangiopancreatography (ERCP). This article includes a brief overview of gallstone imaging and emerging trends in the detection of gallstones. This review article will highlight complications of gallstones, including choledocholithiasis, gallstone pancreatitis, acute cholangitis, Mirizzi syndrome, cholecystobiliary and cholecystoenteric fistulas, and gallstone ileus. Imaging findings and limitations of US, CT, MRI, and ERCP will be discussed. The review article will also briefly discuss the management of each disease. The presence of gallstones beyond the level of the cystic duct can lead to a spectrum of diseases, and emergency radiologists play a critical role in disease management by providing a timely diagnosis. Documenting the location of a gallstone within the common bile duct (CBD) in symptomatic cholelithiasis and the presence of acute interstitial edematous pancreatitis and/or ascending cholangitis plays a pivotal role in disease management. Establishing the presence of ectopic gallstones and biliary-enteric fistulae has a significant role in directing patient management.










Similar content being viewed by others
Data availability
Not applicable.
Code availability
Not applicable.
References
Zimmer V, Lammert F (2015) Acute bacterial cholangitis. Viszeralmedizin 31(3):166–172. https://doi.org/10.1159/000430965
Chang L et al (2018) Clinical and radiological diagnosis of gallstone ileus: a mini review. Emerg Radiol 25(2):189–196. https://doi.org/10.1007/s10140-017-1568-5
Kratzer W, Mason RA, Kächele V (1999) Prevalence of gallstones in sonographic surveys worldwide. J Clin Ultrasound 27(1):1–7
Sakorafas GH, Milingos D, Peros G (2007) Asymptomatic cholelithiasis: is cholecystectomy really needed? A critical reappraisal 15 years after the introduction of laparoscopic cholecystectomy. Dig Dis Sci 52(5):1313–1325
Gracie WA, Ransohoff DF (1982) The natural history of silent gallstones: the innocent gallstone is not a myth. N Engl J Med 307(13):798–800
Ruhl CE, Everhart JE (2011) Gallstone disease is associated with increased mortality in the United States. Gastroenterology 140(2):508–516
McIntosh DM, Penney HF (1980) Gray-scale ultrasonography as a screening procedure in the detection of gallbladder disease. Radiology 136(3):725–727. https://doi.org/10.1148/radiology.136.3.7403554
Bortoff GA et al (2000) Gallbladder stones: imaging and intervention. Radiographics 20(3):751–766. https://doi.org/10.1148/radiographics.20.3.g00ma16751
MacDonald FR, Cooperberg PL, Cohen MM (1981) The WES triad — a specific sonographic sign of gallstones in the contracted gallbladder. Gastrointest Radiol 6(1):39–41. https://doi.org/10.1007/BF01890219
Ratanaprasatporn L et al (2018) Multimodality imaging, including dual-energy CT, in the evaluation of gallbladder disease. Radiographics 38(1):75–89. https://doi.org/10.1148/rg.2018170076
Patel NB, Oto A, Thomas S (2013) Multidetector CT of emergent biliary pathologic conditions. Radiographics 33(7):1867–1888. https://doi.org/10.1148/rg.337125038
Gore RM et al (2010) Gallbladder imaging. Gastroenterol Clin North Am 39(2):265–287. https://doi.org/10.1016/j.gtc.2010.02.009
Uyeda JW, Richardson IJ, Sodickson AD (2017) Making the invisible visible: improving conspicuity of noncalcified gallstones using dual-energy CT. Abdom Radiol (NY) 42(12):2933–2939. https://doi.org/10.1007/s00261-017-1229-x
Yang CB et al (2017) Clinical application of dual-energy spectral computed tomography in detecting cholesterol gallstones from surrounding bile. Acad Radiol 24(4):478–482. https://doi.org/10.1016/j.acra.2016.10.006
Bae JS et al. (2019) Utilization of virtual non-contrast images derived from dual-energy CT in evaluation of biliary stone disease: virtual non-contrast image can replace true non-contrast image regarding biliary stone detection. Eur J Radiol 116: 34–40. https://www.sciencedirect.com/science/article/pii/S0720048X19301408. Accessed 2 Nov 2021
Murphy MC et al (2020) Gallstones top to toe: what the radiologist needs to know. Insights Imaging 11(1):13. https://doi.org/10.1186/s13244-019-0825-4
Mendler MH et al (1998) Value of MR cholangiography in the diagnosis of obstructive diseases of the biliary tree: a study of 58 cases. Am J Gastroenterol 93(12):2482–2490
Gutt C, Schläfer S, Lammert F (2020) The treatment of gallstone disease. Dtsch Arztebl Int 117(9):148–158
Tazuma S (2006) Epidemiology, pathogenesis, and classification of biliary stones (common bile duct and intrahepatic). Best Pract Res Clin Gastroenterol 20(6):1075–1083. https://doi.org/10.1016/j.bpg.2006.05.009
Perveze Z, Krishnamurthy C, Duckworth CW (2008) The incidence of choledocholithiasis in a community setting. Gastrointest Endosc 67(5):AB297. https://doi.org/10.1016/j.gie.2008.03.863
Dasari BV et al (2013) Surgical versus endoscopic treatment of bile duct stones. Cochrane Database Syst Rev 12:CD003327. https://doi.org/10.1002/14651858.cd003327.pub4
Molvar C, Glaenzer B (2016) Choledocholithiasis: evaluation, treatment, and outcomes. Semin Intervent Radiol 33(4):268–276
Condon FJ (2019) Choledocholithiasis and cholangitis: incidence, initial management, and surgical management. In: Lim R (ed) Multidisciplinary approaches to common surgical problems. Springer International Publishing, Cham, pp 161–166
Abraham S et al (2014) Surgical and nonsurgical management of gallstones. Am Fam Physician 89(10):795–802
Perret RS, Sloop GD, Borne JA (2000) Common bile duct measurements in an elderly population. J Ultrasound Med 19(11):727–730. https://doi.org/10.7863/jum.2000.19.11.727
Einstein DM et al (1984) The insensitivity of sonography in the detection of choledocholithiasis. Am J Roentgenol 142(4):725–728. https://doi.org/10.2214/ajr.142.4.725
Veronica B et al (2019) Imaging of biliary colic and cholecystitis. In: Cova MA, Stacul F (eds) Pain imaging: a clinical-radiological approach to pain diagnosis. Springer International Publishing, Cham, pp 229–245
Wertz JR et al (2018) Comparing the diagnostic accuracy of ultrasound and CT in evaluating acute cholecystitis. AJR Am J Roentgenol 211(2):W92-w97
Anderson SW et al (2006) Accuracy of MDCT in the diagnosis of choledocholithiasis. Am J Roentgenol 187(1):174–180. https://doi.org/10.2214/AJR.05.0459
Verma D et al (2006) EUS vs MRCP for detection of choledocholithiasis. Gastrointest Endosc 64(2):248–254
Makmun D, Fauzi A, Shatri H (2017) Sensitivity and specificity of magnetic resonance cholangiopancreatography versus endoscopic ultrasonography against endoscopic retrograde cholangiopancreatography in diagnosing choledocholithiasis: the Indonesian experience. Clin Endosc 50(5):486–490
Gurusamy KS et al (2015) Endoscopic retrograde cholangiopancreatography versus intraoperative cholangiography for diagnosis of common bile duct stones. Cochrane Database Syst Rev 2015(2):Cd010339
Kint JF et al (2015) Percutaneous treatment of common bile duct stones: results and complications in 110 consecutive patients. Dig Surg 32(1):9–15
Jung GS et al (2019) Percutaneous transcholecystic removal of common bile duct stones: case series in 114 patients. Radiology 290(1):238–243
Pereira J et al (2017) Accuracy of ultrasound in the diagnosis of acute cholecystitis with coexistent acute pancreatitis. Eur J Trauma Emerg Surg 43(1):79–83. https://doi.org/10.1007/s00068-015-0619-4
Koo BC, Chinogureyi A, Shaw AS (2010) Imaging acute pancreatitis. Br J Radiol 83(986):104–112. https://doi.org/10.1259/bjr/13359269
Surlin V, Saftoiu A, Dumitrescu D (2014) Imaging tests for accurate diagnosis of acute biliary pancreatitis. World J Gastroenterol 20(44):16544–16549. https://doi.org/10.3748/wjg.v20.i44.16544
Neoptolemos JP et al (2005) The urgent diagnosis of gallstones in acute pancreatitis: a prospective study of three methods. Br J Surg 71(3):230–233. https://doi.org/10.1002/bjs.1800710324
Shah AP, Mourad MM, Bramhall SR (2018) Acute pancreatitis: current perspectives on diagnosis and management. J Inflamm Res 11:77–85. https://doi.org/10.2147/jir.s135751
Baron RL et al (1983) Computed tomographic features of biliary obstruction. AJR Am J Roentgenol 140(6):1173–1178
Vege SS et al (2018) Initial medical treatment of acute pancreatitis: American Gastroenterological Association Institute technical review. Gastroenterology 154(4):1103–1139. https://doi.org/10.1053/j.gastro.2018.01.031
O’Connor OJ, McWilliams S, Maher MM (2011) Imaging of acute pancreatitis. AJR Am J Roentgenol 197(2):W221–W225. https://doi.org/10.2214/ajr.10.4338
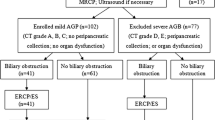
Alexakis N, Neoptolemos JP (2005) Algorithm for the diagnosis and treatment of acute biliary pancreatitis. Scand J Surg 94(2):124–129. https://doi.org/10.1177/145749690509400208
Perera M et al (2013) A case of concomitant perforated acute cholecystitis and pancreatitis. Case Rep Surg 2013:263046. https://doi.org/10.1155/2013/263046
Friedman GD (1993) Natural history of asymptomatic and symptomatic gallstones. Am J Surg 165(4):399–404
Catalano OA et al (2009) Biliary infections: spectrum of imaging findings and management. Radiographics 29(7):2059–2080. https://doi.org/10.1148/rg.297095051
Reynolds BM, Dargan EL (1959) Acute obstructive cholangitis; a distinct clinical syndrome. Ann Surg 150(2):299–303. https://doi.org/10.1097/00000658-195908000-00013
Bader TR et al (2001) MR imaging findings of infectious cholangitis. Magn Reson Imaging 19(6):781–788. https://doi.org/10.1016/s0730-725x(01)00401-5
Ahmed M (2018) Acute cholangitis - an update. World J Gastrointest Pathophysiol 9(1):1–7. https://doi.org/10.4291/wjgp.v9.i1.1
Lee JG (2009) Diagnosis and management of acute cholangitis. Nat Rev Gastroenterol Hepatol 6(9):533–541. https://doi.org/10.1038/nrgastro.2009.126
Lai EC, Lau WY (2006) Mirizzi syndrome: history, present and future development. ANZ J Surg 76(4):251–257. https://doi.org/10.1111/j.1445-2197.2006.03690.x
Beltran MA (2012) Mirizzi syndrome: history, current knowledge and proposal of a simplified classification. World J Gastroenterol 18(34):4639–4650. https://doi.org/10.3748/wjg.v18.i34.4639
Beltran MA, Csendes A (2005) Mirizzi syndrome and gallstone ileus: an unusual presentation of gallstone disease. J Gastrointest Surg 9(5):686–689. https://doi.org/10.1016/j.gassur.2004.09.058
Beltran MA, Csendes A, Cruces KS (2008) The relationship of Mirizzi syndrome and cholecystoenteric fistula: validation of a modified classification. World J Surg 32(10):2237–2243. https://doi.org/10.1007/s00268-008-9660-3
Csendes A et al (1989) Mirizzi syndrome and cholecystobiliary fistula: a unifying classification. Br J Surg 76(11):1139–1143. https://doi.org/10.1002/bjs.1800761110
Abou-Saif A, Al-Kawas FH (2002) Complications of gallstone disease: Mirizzi syndrome, cholecystocholedochal fistula, and gallstone ileus. Am J Gastroenterol 97(2):249–254. https://doi.org/10.1111/j.1572-0241.2002.05451.x
Lubbers EJ (1983) Mirizzi syndrome. World J Surg 7(6):780–785. https://doi.org/10.1007/bf01655221
Montefusco P, Spier N, Geiss AC (1983) Another facet of Mirizzi’s syndrome. Arch Surg 118(10):1221–1223. https://doi.org/10.1001/archsurg.1983.01390100083021
Dietrich KF (1963) Stenosis of the hepatic duct in lithiasis of the gallbladder neck and cystic duct (Mirizzi syndrome). Bruns Beitr Klin Chir 206:9–22
Redaelli CA et al (1997) High coincidence of Mirizzi syndrome and gallbladder carcinoma. Surgery 121(1):58–63
Beltrán MA (2012) Mirizzi syndrome: history, current knowledge and proposal of a simplified classification. World J Gastroenterol 18(34):4639–4650
Solis-Caxaj CA (2009) Mirizzi syndrome: diagnosis, treatment and a plea for a simplified classification. World J Surg 33(8):1783–1784. https://doi.org/10.1007/s00268-009-9929-1
Shirah BH, Shirah HA, Albeladi KB (2017) Mirizzi syndrome: necessity for safe approach in dealing with diagnostic and treatment challenges. Ann Hepatobiliary Pancreat Surg 21(3):122–130. https://doi.org/10.14701/ahbps.2017.21.3.122
Tan KY et al (2004) Mirizzi syndrome: noteworthy aspects of a retrospective study in one centre. ANZ J Surg 74(10):833–837. https://doi.org/10.1111/j.1445-1433.2004.03184.x
Choi BW et al (2000) Radiologic findings of Mirizzi syndrome with emphasis on MRI. Yonsei Med J 41(1):144–146. https://doi.org/10.3349/ymj.2000.41.1.144
Chen H et al (2018) Current trends in the management of Mirizzi Syndrome: a review of literature. Medicine (Baltimore) 97(4):e9691. https://doi.org/10.1097/md.0000000000009691
Balent E, Plackett TP, Lin-Hurtubise K (2012) Cholecystocolonic fistula. Hawaii J Med Public Health 71(6):155–157
Liang X et al (2015) Comparative analysis of MDCT and MRI in diagnosing chronic gallstone perforation and ileus. Eur J Radiol 84(10):1835–1842. https://doi.org/10.1016/j.ejrad.2015.06.009
Oskam J, Heitbrink M, EeftinckSchattenkerk M (1993) Intermittent gallstone ileus following endoscopic biliary sphincterotomy. A case report. Acta Chir Belg 93(2):43–5
Foss H, Summers J (1942) Intestinal obstruction from gallstones. Ann Surg 115:721
Masannat Y, Masannat Y, Shatnawei A (2006) Gallstone ileus: a review. Mt Sinai J Med 73(8):1132–1134
Halabi WJ et al (2014) Surgery for gallstone ileus: a nationwide comparison of trends and outcomes. Ann Surg 259(2):329–335. https://doi.org/10.1097/sla.0b013e31827eefed
Alemi F, Seiser N, Ayloo S (2019) Gallstone disease: cholecystitis, Mirizzi syndrome, Bouveret syndrome, gallstone ileus. Surg Clin North Am 99(2):231–244. https://doi.org/10.1016/j.suc.2018.12.006
Lassandro F et al (2005) Role of helical CT in diagnosis of gallstone ileus and related conditions. AJR Am J Roentgenol 185(5):1159–1165. https://doi.org/10.2214/ajr.04.1371
Prasad RM, Weimer KM, Baskara A (2017) Gallstone ileus presenting as intussusception: a case report. Int J Surg Case Rep 30:37–39. https://doi.org/10.1016/j.ijscr.2016.11.036
Ayantunde AA, Agrawal A (2007) Gallstone ileus: diagnosis and management. World J Surg 31(6):1292–1297. https://doi.org/10.1007/s00268-007-9011-9
Beuran M, Ivanov I, Venter MD (2010) Gallstone ileus–clinical and therapeutic aspects. J Med Life 3(4):365–371
Yu CY et al (2005) Value of CT in the diagnosis and management of gallstone ileus. World J Gastroenterol 11(14):2142–2147. https://doi.org/10.3748/wjg.v11.i14.2142
Jakubauskas M, et al. (2019) Gallstone ileus: management and clinical outcomes. Medicina (Kaunas) 55(9). https://doi.org/10.3390/medicina55090598
Author information
Authors and Affiliations
Contributions
Dr. Kiran Maddu, Dr. Carrie Hoff, and Dr. Arie Neymotin contributed to the study conception. All authors contributed to the design. Material preparation, including images, was performed by Dr. Maddu, Dr. Hoff, and Dr. Neymotin. The first draft of the manuscript was written by Andrew Tran, Karunesh Polireddy, Dr. Kiran Maddu, Dr. Carrie Hoff, and Dr. Arie Neymotin. All authors commented on previous versions of the manuscript. All authors read and approved the final manuscript.
Corresponding author
Ethics declarations
Ethics approval
Not applicable.
Consent to participate
Not applicable.
Consent for publication
Alterations to figures (to anonymize any patient identifiers) do not distort meaning.
Conflict of interest
The authors declare that they have no conflict of interest.
Additional information
Publisher's note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Rights and permissions
About this article
Cite this article
Tran, A., Hoff, C., Polireddy, K. et al. Beyond acute cholecystitis—gallstone-related complications and what the emergency radiologist should know. Emerg Radiol 29, 173–186 (2022). https://doi.org/10.1007/s10140-021-01999-y
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s10140-021-01999-y