Abstract
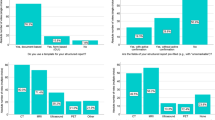
The aim of this study was to identify the risk factors associated with noncompliance of recommendations made by emergency radiologists. Between March 2012 and August 2012, our team retrospectively reviewed 20,000 consecutive emergency department (ED) patients receiving imaging to assess how often emergency radiologists made recommendations, how often they were followed, and what factors were associated with noncompliance. Faculty (Radiology or Emergency Medicine) were considered senior if they had been practicing for >5 years post residency/fellowship training. Faculty practicing <5 years were considered junior physicians. The following data was extracted from the electronic medical records and the hospital information system: recommendation in imaging report, age, gender, race (Caucasian, African-American, and others), insurance status, primary care contact, distance from the hospital to patient residence, and primary language. Recommendations were categorized as follows: (1) immediate follow-up, (2) follow-up 1–4 weeks, (3) follow-up 1–3 months, (4) follow-up 4–6 months, (5) follow-up 7–12 months, and (6) clinical/laboratory follow-up recommendations irrespective of time. We identified 1,650 recommendations (1,650/20,000 = 8.25 %). Using a one-to-one logistic regression analysis, the following factors were significant (P < 0.05) when evaluating noncompliance: increasing age, no primary care physician, lack of insurance, primary language other than English, increased distance from hospital, and extended follow-up interval. Noncompliance with recommended additional imaging (RAI) is multifactorial. Primary and/or referring physicians should take notice of the aforementioned compliance trends and mitigating factors, adopt systematic safety measures and create interdepartmental dialogue with radiology to ensure compliance, and counsel and educate patients about the importance of imaging recommendations.
Similar content being viewed by others
References
Gordon RW, Anderson SW, Ozonoff A, Rekhi S, Soto JA (2013) Blunt pancreatic trauma: evaluation with MDCT technology. Emerg Radiol 20(4):259–266
Plurad DS, Bricker S, Van Natta TL, Neville A, Kim D, Bongard F, Putnam B (2013) Penetrating cardiac injury and the significance of chest computed tomography findings. Emerg Radiol 20(4):279–284
Tempany CM, McNeil BJ (2001) Advances in biomedical imaging. JAMA 285(5):562–567
Ho CY, Hussain S, Alam T, Ahmad I, Wu IC, O'Neill DP (2013) Accuracy of CT cerebral perfusion in predicting infarct in the emergency department: lesion characterization on CT perfusion based on commercially available software. Emerg Radiol 20(3):203–212
Toomey RJ, Ryan JT, McEntee MF, Evanoff MG, Chakraborty DP, McNulty JP, Manning DJ, Thomas EM, Brennan PC (2010) Diagnostic efficacy of handheld devices for emergency radiologic consultation. AJR Am J Roentgenol 194(2):469–474
Arenson RL (2009) Recommendations for additional imaging in radiology reports: radiologists’ self-referral or good clinical practice? Radiology 253(2):291–292
Boland GW, Halpern EF, Gazelle GS (2010) Radiologist report turnaround time: impact of pay-for-performance measures. AJR Am J Roentgenol 195(3):707–711
Shuaib W, Johnson JO, Pande V, Salastekar N, Kang J, He Q, Khosa F (2014) Ventriculoperitoneal shunt malfunction: cumulative effect of cost, radiation, and turnaround time on the patient and the health care system. AJR Am J Roentgenol 202(1):13–17
Shuaib W, Vijayasarathi A, Tiwana MH, Johnson JO, Maddu KK, Khosa F (2013) The diagnostic utility of rib series in assessing rib fractures. Emergency radiology.
DeFlorio R, Coughlin B, Coughlin R, Li H, Santoro J, Akey B, Favreau M (2008) Process modification and emergency department radiology service. Emerg Radiol 15(6):405–412
Slovis TL (2008) The art of communication: strategies to improve patient and information flow : radiology perspective. Pediatr Radiol 38(Suppl 4):S651–S654
Eisinger F, Moatti JP, Béja V, Obadia Y, Alias F, Dressen C (1994) Attitude of the French female population to cancer screening. Bull Cancer 81(8):683–690
Katz SJ, Zemencuk JK, Hofer TP (2000) Breast cancer screening in the United States and Canada, 1994: socioeconomic gradients persist. Am J Public Health 90(5):799–803
Lagerlund M, Sparén P, Thurfjell E, Ekbom A, Lambe M (2000) Predictors of non-attendance in a population-based mammography screening programme; socio-demographic factors and aspects of health behaviour. Eur J Cancer Prev 9(1):25–33
Ruffin MT, Gorenflo DW, Woodman B (2000) Predictors of screening for breast, cervical, colorectal, and prostatic cancer among community-based primary care practices. J Am Board Fam Pract 13(1):1–10
Zackrisson S, Andersson I, Manjer J, Janzon L (2004) Non-attendance in breast cancer screening is associated with unfavourable socio-economic circumstances and advanced carcinoma. Int J Cancer 108(5):754–760
Khosa F, Krinsky G, Macari M, Yucel EK, Berland LL (2013) Managing incidental findings on abdominal and pelvic CT and MRI, part 2: white paper of the ACR Incidental Findings Committee II on vascular findings. J Am Coll Radiol 10(10):789–794
Khosa F, Romney BP, Costa DN, Rofsky NM, Manning WJ (2011) Prevalence of noncardiac findings on clinical cardiovascular MRI. AJR Am J Roentgenol 196(4):W380–W386
Khosa F, Warraich H, Khan A, Mahmood F, Markson L, Clouse ME, Manning WJ (2012) Prevalence of non-cardiac pathology on clinical transthoracic echocardiography. J Am Soc Echocardiogr 25(5):553–557
Waqas S, Johnson J-O, Salastekar N, Maddu KK, Khosa F (2013) Incidental findings detected on abdomino-pelvic multidetector computed tomography performed in the acute setting. The American journal of emergency medicine
Swinker M, Arbogast JG, Murray S (1993) Why do patients decline screening mammography? Fam Pract Res J 13(2):165–170
Beaulieu MD, Béland F, Roy D, Falardeau M, Hébert G (1996) Factors determining compliance with screening mammography. CMAJ 154(9):1335–1343
Sistrom CL, Dreyer KJ, Dang PP, Weilburg JB, Boland GW, Rosenthal DI, Thrall JH (2009) Recommendations for additional imaging in radiology reports: multifactorial analysis of 5.9 million examinations. Radiology 253(2):453–461
London S. American College of Emergency Physicians. Treat ED overcrowding by speeding admissions. (2010). http://www.acep.org/MobileArticle.aspx?id=72995&coll_id=693&parentid=740. Accessed 27 Nov 2013
Field DL, Hedges JR, Arnold KJ, Goldstein-Wayne B, Rouan GW (1988) Limitations of chest pain follow-up from an urban teaching hospital emergency department. J Emerg Med 6(5):363–368
Lerman B, Kobernick MS (1987) Return visits to the emergency department. J Emerg Med 5(5):359–362
Straus JH, Orr ST, Charney E (1983) Referrals from an emergency room to primary care practices at an urban hospital. Am J Public Health 73(1):57–61
Magnusson AR, Hedges JR, Vanko M, McCarten K, Moorhead JC (1993) Follow-up compliance after emergency department evaluation. Ann Emerg Med 22(3):560–567
Dorey F, Amstutz HC (1989) The validity of survivorship analysis in total joint arthroplasty. J Bone Joint Surg Am 71(4):544–548
Murray DW, Britton AR, Bulstrode CJ (1997) Loss to follow-up matters. J Bone Joint Surg (Br) 79(2):254–257
Shuaib W, Tiwana MH (2013) Interdepartmental communication. Ir J Med Sci.
Blane CE, Pinsky RW, Joe AI, Pichan AE, Blajan MR, Helvie MA (2007) Costs of achieving high patient compliance after recall from screening mammography. AJR Am J Roentgenol 188(4):894–896
Conflict of interest
The authors declare that they have no conflict of interest.
Author information
Authors and Affiliations
Corresponding author
Additional information
Faisal Khosa is an American Roentgen Ray scholar.
Rights and permissions
About this article
Cite this article
Shuaib, W., Vijayasarathi, A., Johnson, JO. et al. Factors affecting patient compliance in the acute setting: an analysis of 20,000 imaging reports. Emerg Radiol 21, 373–379 (2014). https://doi.org/10.1007/s10140-014-1209-1
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s10140-014-1209-1