Abstract
Background
Blue laser imaging (BLI) is a new image-enhanced endoscopy technique that utilizes a laser light source developed for narrow-band light observation. The aim of this study was to evaluate the usefulness of BLI for the diagnosis of early gastric cancer.
Methods
This single center prospective study analyzed 530 patients. The patients were examined with both conventional endoscopy with white-light imaging (C-WLI) and magnifying endoscopy with BLI (M-BLI) at Kyoto Prefectural University of Medicine between November 2012 and March 2015. The diagnostic criteria for gastric cancer using M-BLI included an irregular microvascular pattern and/or irregular microsurface pattern, with a demarcation line according to the vessel plus surface classification system. Biopsies of the lesions were taken after C-WLI and M-BLI observation. The primary end point of this study was to compare the diagnostic performance between C-WLI and M-BLI.
Results
We analyzed 127 detected lesions (32 cancers and 95 non-cancers). The accuracy, sensitivity, and specificity of M-BLI diagnoses were 92.1, 93.8, and 91.6 %, respectively. On the other hand, the accuracy, sensitivity, and specificity of C-WLI diagnoses were 71.7, 46.9, and 80.0 %, respectively.
Conclusions
M-BLI had improved diagnostic performance for early gastric cancer compared with C-WLI. These results suggested that the diagnostic effectiveness of M-BLI is similar to that of magnifying endoscopy with narrow-band imaging (M-NBI).
Similar content being viewed by others
Introduction
Gastric cancer is the second most common cause of cancer-associated deaths worldwide [1]. Early detection and treatment has led to improved survival rates, with esophagogastroduodenoscopy (EGD) proving to be the most useful method of diagnosis for early gastric cancer (EGC). However, it is often difficult to detect gastric superficial adenocarcinomas using conventional endoscopy with white-light imaging (C-WLI). Many clinical studies have reported on the diagnostic performance of EGC by image-enhanced endoscopy (IEE) techniques such as narrow-band imaging (NBI) [2–9] or flexible spectral imaging color enhancement (FICE) [10–12]. In particular, magnifying endoscopy with NBI (M-NBI) is a powerful optical IEE that has demonstrated accurate real-time diagnostic performance in EGC compared with C-WLI [5, 7].
Recently, Fujifilm developed an endoscope system with a semiconductor laser as a light source. The system includes two types of lasers with wavelengths of 410 and 450-nm. The 450-nm laser irradiates phosphor to produce illumination light similar to that obtained with a xenon lamp. The combination of strong 410-nm laser light, weak 450-nm laser light, and fluorescent light enables blue laser imaging (BLI) via narrow-band light observation. Magnifying endoscopy with BLI (M-BLI) is useful for evaluating mucosal surface information such as surface blood vessel and structure patterns [13–16].
M-BLI has the potential to diagnose EGC as efficiently as M-NBI because it uses narrow-band laser light combined with illumination light. However, sufficient data have not been reported regarding its diagnostic performance for EGC. Therefore, we aimed to investigate whether M-BLI is more effective for diagnostic accuracy of EGC when compared with C-WLI.
Patients and methods
Patients
A prospective single-center study was conducted at the Department of Molecular Gastroenterology and Hepatology, Kyoto Prefectural University of Medicine. A total of 530 consecutive patients with EGC or superficial esophageal cancer underwent EGD prior to endoscopic submucosal dissection (ESD) at the University Hospital, Kyoto Prefectural University of Medicine were enrolled in this study between November 2012 and March 2015. All patients provided written informed consents to undergo EGD by both C-WLI and M-BLI. If undetected lesions were found and diagnosed as gastric adenoma or adenocarcinoma pathologically, ESD were performed on the day after obtaining additional informed consent from the patients.
This study was approved by the Ethical Review Committee of the Kyoto Prefectural University of Medicine and carried out in accordance with the Helsinki Declaration of the World Medical Association. In addition, this study was registered in the University Hospital Medical Information Network Clinical Trials Registry (UMIN-CTR) as No. UMIN000009216.
End points
The primary aim of this study was to compare the diagnostic performance (accuracy sensitivity, specificity, positive predictive value, and negative predictive value) between C-WLI and M-BLI. The secondary aim was to evaluate the features of misdiagnosed lesions by M-BLI.
Endoscopic system and device
All procedures were carried out with optical magnifying EG-L590ZW endoscopes and the LASEREO endoscopic system (Fujifilm Medical Co., Tokyo, Japan). BLI can be applied with the push of a button. In the BLI mode, the structure enhancement function was constantly set at the A6 level, with the color mode fixed at level 1. To obtain magnified endoscopic images of the lesion easily, we attached a black soft hood (MAJ-1989; Olympus Medical Systems, Tokyo, Japan) on the tip of the scope.
Participating endoscopists
All examinations were performed by four skilled endoscopists who had participated in more than 100 EGC cases of M-BLI; this minimized diagnostic variation of the analyses.
Endoscopic examination
In practice, when an elevated or depressive lesion on the gastric mucosa was diagnosed as cancer or there was a suspicion of cancer, the lesion was diagnosed by C-WLI as a target lesion. After the C-WLI diagnosis was complete, an assistant physician immediately recorded the results in the case notes. Next, M-BLI was performed and the results were recorded in the case notes. Afterwards, one forceps biopsy specimen was taken from each lesion. The following lesions were excluded from this study in order to evaluate the usefulness of M-BLI for diagnoses of the new detected lesions in daily clinical situation: (1) superficial gastric lesions with pathological diagnoses (cancer or non-cancer) before the study, (2) gastric polyps or protruding lesions, (3) superficial gastric lesions without detailed observation using M-BLI, (4) superficial gastric lesions diagnosed using C-WLI as benign with no need of biopsy, and (5) superficial gastric lesions with indeterminate pathological diagnoses obtained by biopsy specimen.
Diagnostic criteria
The diagnostic criteria for gastric cancer using C-WLI were shallow, depressed, or flat elevated lesions with both an irregular margin and an irregular mucosal area. The endoscopic diagnostic criteria for gastric cancer using M-BLI were defined based on previous reports of vessel plus surface (VS) classification: the presence of either an irregular microvascular pattern with a demarcation line, or the presence of an irregular microsurface pattern with a demarcation line [3].
Pathological diagnosis
Specimens of all lesions were obtained by biopsy or ESD and were subsequently fixed with 10 % formalin and evaluated pathologically. The pathological diagnoses were completed by a highly experienced clinical pathologist (A. Yanagisawa) who was blind to the actual magnified endoscopic findings, which were categorized according to the Japanese Classification of Gastric Carcinoma proposed by the Japanese Gastric Cancer Association [17]. If there were diagnostic differences between biopsy and ESD specimens, the final diagnoses were evaluated according to ESD specimens.
Statistical analysis
In a pilot study, 60 gastric lesions including 12 EGCs were examined using both C-WLI and M-BLI. Seven of 12 EGCs (58 %) had different diagnoses between C-WLI and M-BLI. The diagnoses of M-BLI were accurate compared with those of C-WLI in six of seven EGCs (86 %). These data indicated that the proportion of cancerous lesions with a different diagnosis for the response of matched pairs was 58 %, and the proportion of cancerous lesions with an improved diagnosis for BLI was 86 %. Accordingly, we needed to study 15 cancerous lesions with different diagnostic results to be able to reject a null hypothesis that the response difference was zero with probability (power) 0.8. The Type I error probability associated with a study of this null hypothesis is 0.05. Since the proportion of patients with a different diagnosis in the response of matched pairs was 58 %, the sample size was set to 26 cancerous lesions. The frequency of synchronous or metachronous multiple gastric cancers in patients with previous gastric cancers was reported as 3–5 per 100 patient-years [18–20]. Moreover, it was reported that the frequency of synchronous or metachronous gastric cancers was 7.7 % in patients with esophageal cancer [21]. Therefore, we hypothesized that the frequency of cancerous lesions would be 5.0 % for patients with gastric cancer or esophageal cancer and calculated the required size of the screening sample to be at least 520 patients.
McNemar’s test was used to analyze the accuracy of endoscopic diagnosis and biopsy diagnosis. The diagnostic accuracy of each of the endoscopic findings is presented as a percentage (95 % confidence interval). A p value of less than 0.05 was considered statistically significant. All statistical analyses were performed using SPSS, version 15.0 (SPSS Inc., Chicago, IL, USA).
Results
Between November 2012 and March 2015, 530 patients were enrolled in this study; 407 patients underwent EGD for EGC prior to ESD, 123 patients underwent EGD for superficial esophageal cancer prior to ESD. Among all patients, 139 previously undiagnosed lesions were detected during C-WLI in 132 patients. Among these detected lesions, the M-BLI findings in seven lesions were inappropriate due to difficulties in detail observation, and three lesions were impossible to judge for malignancy or benignancy on pathological diagnoses, while two lesions were diagnosed pathologically by biopsy specimens before the study. Other than these 12 cases, the 127 lesions comprised 32 gastric cancers, three gastric adenomas, and 92 non-tumorous tissues (86 chronic gastritis and 6 intestinal metaplasia). Resected gastric cancers included 29 well-differentiated adenocarcinomas, two moderately differentiated adenocarcinomas, and one poorly differentiated adenocarcinoma (Fig. 1). The clinicopathological features of the evaluated lesions are summarized in Table 1. The frequency of detected synchronous EGCs was 6.8 % (28 EGCs) in 407 patients with EGC prior to ESD and 3.2 % (4 EGCs) in 123 patients with superficial esophageal cancer prior to ESD.
The outcomes of C-WLI and pathological diagnoses for the 127 lesions are shown in Table 2. We diagnosed cancerous lesions in 34 of 127 superficial gastric lesions with C-WLI. However, only 15 of the 34 lesions diagnosed as cancers with C-WLI (44.1 %) were diagnosed pathologically to be cancers. The outcomes of M-BLI and pathological diagnoses for all of the 127 lesions evaluated are shown in Table 3. We diagnosed cancerous lesions for 38 of the 127 superficial gastric lesions with M-BLI; 30 of these 38 lesions (78.9 %) were diagnosed pathologically to be cancers. Three of eight of the false-positive lesions were diagnosed pathologically to be gastric adenomas. The other five false-positive lesions were shallow depressed lesions that were diagnosed pathologically to be chronic gastritis.
The sensitivity of M-BLI diagnoses was significantly higher than that of C-WLI (93.8 vs. 46.9 %, respectively), as was the specificity (80.0 vs. 91.6 %, respectively), positive predictive value (44.1 vs. 78.9 %, respectively), negative predictive value (81.7 vs. 97.7 %, respectively), and accuracy (71.2 vs. 92.1 %, respectively) (Table 4).
Representative cases
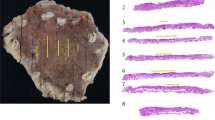
Representative C-WLI and M-BLI images of gastric cancer and non-cancerous lesions are shown in Figs. 2 and 3. Representative case 1 is a superficial elevated lesion on the lesser curvature of the middle gastric body. A slight irregular mucosal lesion is visible on the lesser curvature of the middle gastric body, but the margin of the lesion is unclear on C-WLI (Fig. 2a). Thus, the lesion was diagnosed as a non-cancerous lesion by C-WLI. The demarcation of the lesion is clearly distinguishable because of both the irregular microvascular pattern and the irregular microsurface pattern on M-BLI (Fig. 2b), and was thus diagnosed as a cancer. The lesion was diagnosed as a well-differentiated adenocarcinoma by ESD specimens (Fig. 2c). Representative case 2 is a superficial depressed lesion on the lesser curvature of the upper gastric body. A slight irregular mucosal lesion is visible on the lesser curvature of the middle gastric body, but the margin of the lesion is clear on C-WLI (Fig. 3a). Thus, the lesion was diagnosed as a cancer by C-WLI. The demarcation of the lesion is clearly visible because of both the irregular microvascular pattern and the irregular microsurface pattern (Fig. 3b). Thus, the lesion was diagnosed as a cancer by M-BLI. The lesion was diagnosed as fundic and pyloric gland mucosa with mild edema and inflammatory cell infiltration by a biopsy specimen (Fig. 3c).
A positive case with M-BLI diagnosis (case 1). Superficial elevated lesion on the lesser curvature of the middle gastric body. a C-WLI image shows a slight irregular mucosal lesion with unclear margin (arrowhead). b M-BLI image shows both irregular microvascular pattern and irregular microsurface pattern with a clear demarcation line (arrows). c Histopathological image of biopsy specimen shows a well-differentiated adenocarcinoma. C-WLI conventional endoscopy with white-light imaging, M-BLI magnifying endoscopy with blue laser imaging
A false-positive case with M-BLI diagnosis (case 2). Superficial depressed lesion on the posterior wall of the upper gastric body. a C-WLI image shows a reddish irregular mucosal lesion with clear margin (arrowhead). b M-BLI image shows both irregular microvascular pattern and irregular microsurface pattern with a demarcation line (arrows). c Histopathological image of biopsy specimen shows a fundic and pyloric gland mucosa with mild edema and inflammatory cell infiltration. C-WLI conventional endoscopy with white-light imaging, M-BLI magnifying endoscopy with blue laser imaging
Discussion
This is the first comparative report of M-BLI being useful for the diagnosis of EGC. In this study, M-BLI clearly detected microvascular pattern, microsurface pattern, and demarcation line. Thus, VS classification by M-BLI correlated well with the pathological diagnoses. The sensitivity, specificity, and accuracy of M-BLI after C-WLI were excellent at 93.8, 91.6, and 92.1 %, respectively. In previous reports, Ezoe et al. showed that the sensitivity, specificity, and accuracy of M-NBI after C-WLI for the diagnosis of small depressed lesions were excellent at 95.0, 96.8, and 96.6 %, respectively [7]. Yamada et al. showed that the sensitivity, specificity, accuracy, positive predictive value, and negative predictive value of M-NBI after C-WLI for the diagnosis of small depressed lesions were excellent at 95, 97, 97, 79, and 99 %, respectively [8]. Based on our findings, the M-BLI diagnoses using VS classification were excellent, as were the M-NBI diagnoses. Our study included both elevated and depressed lesions; thus, the sensitivity, specificity, and accuracy of M-BLI might be slightly lower score than that of M-NBI. In addition, the positive predictive value of M-BLI was slightly low at 78.9 % when compared with other scores. Moreover, we investigated the reasons why eight non-cancerous lesions were incorrectly diagnosed as cancers using M-BLI. In five non-tumorous lesions, the finding of irregular microvascular and microsurface pattern prompted a cancer diagnosis. In three other adenomas, flat-elevated lesions with focal irregular microsurface pattern and regular microvasuclar pattern were diagnosed as cancers using M-BLI. The difficulty of diagnosing these lesions was a limitation of M-BLI using VS classification.
It was previously reported that the sensitivity and specificity of the gastrofiberscopic biopsy method for gastric malignancies were 93.8 and 99.6 %, respectively, and the overall accuracy for all the patients was 97.4 % [22]. In our study, the sensitivity of M-BLI was as high as biopsy method. When the lesion is diagnosed to be a cancer by M-BLI, taking a biopsy specimen is highly recommended to confirm the pathology. On the other hand, specificity and negative predictive value of M-BLI was high in our study. When the lesion is not suspected to be a cancer by M-BLI, we could decrease the number of unnecessary biopsies.
Our study has a major limitation. This study provided only a limited evaluation of M-BLI and the VS classification system, which is a diagnostic tool for M-NBI. We previously reported the evaluation of endoscopic image between M-BLI and M-NBI. M-BLI could detect microvascular pattern and microsurface pattern the same as M-NBI. With VS classification criteria, the accuracy of M-NBI and M-BLI were 94.1 and 95.3 %, respectively. There was not significantly difference in appearance of microvascular pattern [23]. However, the number of patients was small and the data were gathered from a single center. Therefore, further multi-institutional studies with a large number of cases are required to evaluate the diagnostic accuracy and findings using VS classification for EGC between M-BLI and M-NBI. Thus, a multi-institutional prospective study (UMIN-CTR 000007300) has already been done and the data processing is now ongoing.
In conclusion, M-BLI had greater diagnostic performance for early gastric cancer than C-WLI. These results suggest that the diagnostic effectiveness of M-BLI is similar to that of M-NBI.
References
Ferlay J, Shin HR, Bray F, Forman D, Mathers C, Parkin DM. Estimates of worldwide burden of cancer in 2008: GLOBOCAN 2008. Int J Cancer. 2010;15(127):2893–917.
Nakayoshi T, Tajiri H, Matsuda K, Kaise M, Ikegami M, Sasaki H. Magnifying endoscopy combined with narrow band imaging system for early gastric cancer: correlation of vascular pattern with histopathology (including video). Endoscopy. 2004;36:1080–4.
Yao K, Anagnostopoulos GK, Ragunath K. Magnifying endoscopy for diagnosing and delineating early gastric cancer. Endoscopy. 2009;41(5):462–7.
Ezoe Y, Muto M, Horimatsu T, Minashi K, Yano T, Sano Y, et al. Magnifying narrow-band imaging versus magnifying white-light imaging for the differential diagnosis of gastric small depressive lesions: a prospective study. Gastrointest Endosc. 2010;71:477–84.
Kato M, Kaise M, Yonezawa J, Toyoizumi H, Yoshimura N, Yoshida Y, et al. Magnifying endoscopy with narrow-band imaging achieves superior accuracy in the differential diagnosis of superficial gastric lesions identified with white-light endoscopy: a prospective study. Gastrointest Endosc. 2010;72(3):523–9.
Kiyotoki S, Nishikawa J, Satake M, Fukagawa Y, Shirai Y, Hamabe K, et al. Usefulness of magnifying endoscopy with narrow-band imaging for determining gastric tumor margin. J Gastroenterol Hepatol. 2010;25(10):1636–41.
Ezoe Y, Muto M, Uedo N, Doyama H, Yao K, Oda I, et al. Magnifying narrowband imaging is more accurate than conventional white-light imaging in diagnosis of gastric mucosal cancer. Gastroenterology. 2011;141:2017–25.
Yamada S, Doyama H, Tao K, Uedo N, Ezoe Y, Oda I, et al. An efficient diagnostic strategy for small, depressed early gastric cancer with magnifying narrow-band imaging: a post hoc analysis of a prospective randomized controlled trial. Gastrointest Endosc. 2014;79(1):55–63.
Yao K, Doyama H, Gotoda T, Ishikawa H, Nagahama T, Yokoi C, et al. Diagnostic performance and limitations of magnifying narrow-band imaging in screening endoscopy of early gastric cancer: a prospective multicenter feasibility study. Gastric Cancer. 2014;17(4):669–79.
Osawa H, Yamamoto H, Miure Y, Ajibe H, Shinhata H, Yoshizawa M, et al. Diagnosis of depressed-type early gastric cancer using small-caliber endoscopy with flexible spectral imaging color enhancement. Dig Endosc. 2012;24(4):231–6.
Osawa H, Yamamoto H, Miura Y, Yoshizawa M, Sunada K, Satoh K, et al. Diagnosis of extent of early gastric cancer using flexible spectral imaging color enhancement. World J Gastrointest Endosc. 2012;4(8):356–61.
Dohi O, Yagi N, Wada T, Yamada N, Bito N, Yamada S, et al. Recognition of endoscopic diagnosis in differentiated-type early gastric cancer by flexible spectral imaging color enhancement with indigo carmine. Digestion. 2012;86(2):161–70.
Yoshida N, Hisabe T, Inada Y, Kugai M, Yagi N, Hirai F, et al. The ability of a novel blue laser imaging system for the diagnosis of invasion depth of colorectal neoplasms. J Gastroenterol. 2014;49:73–80.
Yoshida N, Yagi N, Inada Y, Kugai M, Okayama T, Kamada K, et al. The ability of a novel blue laser imaging system for the diagnosis of colorectal polyps. Dig Endosc. 2014;26:250–8.
Osawa H, Yamamoto H. Present and future status of flexible spectral imaging color enhancement and blue laser imaging technology. Dig Endosc. 2014;26(Suppl. 1):105–15.
Miyaki R, Yoshida S, Tanaka S, Kominami Y, Sanomura Y, Matsuo T, et al. A computer system to be used with laser-based endoscopy for quantitative diagnosis of early gastric cancer. J Clin Gastroenterol. 2015;49(2):108–15.
Japanese Gastric Cancer Association. Japanese classification of gastric carcinoma—3rd English edition. Gastric Cancer. 2011;14:101–12.
Aoi T, Marusawa H, Sato T, Chiba T, Maruyama M. Risk of subsequent development of gastric cancer in patients with previous gastric epithelial neoplasia. Gut. 2006;55:588–9.
Fukase K, Kato M, Kikuchi S, Inoue K, Uemura N, Okamoto S, et al. Effect of eradication of Helicobacter pylori on incidence of metachronous gastric carcinoma after endoscopic resection of early gastric cancer: an openlabel, randomised controlled trial. Lancet. 2008;372:392–7.
Nakajima T, Oda I, Gotoda T, Hamanaka H, Eguchi T, Yokoi C, et al. Metachronous gastric cancers after endoscopic resection: how effective is annual endoscopic surveillance? Gastric Cancer. 2006;9:93–8.
Natsugoe S, Natsugoe S, Matsumoto M, Okumura H, Ishigami S, Uenosono Y, et al. Multiple primary carcinomas with esophageal squamous cell cancer: clinicopathologic outcome. World J Surg. 2005;29:46–9.
Tatsuta M, Iishi H, Okuda S, Oshima A, Taniguchi H. Prospective evaluation of diagnostic accuracy of gastrofiberscopic biopsy in diagnosis of gastric cancer. Cancer. 1989;63:1415–20.
Yagi N, Naito Y, Dohi O, Yoshida N, Kamada K, Uchiyama K, et al. The efficacy of a novel blue LASER imaging system for the diagnosis of early gastric cancers; a prospective single center open trial. Gastrointest Endosc. 2013;77:Supplement AB458.
Acknowledgments
We thank all members of the Department of Molecular Gastroenterology and Hepatology, Graduate School of Medical Science, Kyoto Prefectural University of Medicine, for helping conduct this study. We also thank Kubo Masahiro and all personnel who assisted with operation of the Fujifilm LASEREO system.
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
Conflict of interest
Y. Naito received collaboration research funding from Fujifilm Medical Co., Ltd. (J132001115, J132001139). N. Yagi and Y. Itoh were affiliated with a department that was partially funded by Fujifilm Medical Co., Ltd. (J082003006). Fujifilm Medical Co., Ltd. had no role in the design, conduct, data collection, data interpretation, or reportage of the study.
Human rights statement and informed consent
All procedures followed were in accordance with the ethical standards of the responsible committee on human experimentation (The Ethical Review Committee of the Kyoto Prefectural University of Medicine and national) and with the Helsinki Declaration of 1964 and later versions. Informed consent or substitute for it was obtained from all patients included in the study.
Rights and permissions
About this article
Cite this article
Dohi, O., Yagi, N., Majima, A. et al. Diagnostic ability of magnifying endoscopy with blue laser imaging for early gastric cancer: a prospective study. Gastric Cancer 20, 297–303 (2017). https://doi.org/10.1007/s10120-016-0620-6
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s10120-016-0620-6