Abstract
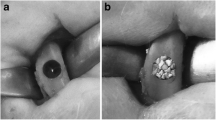
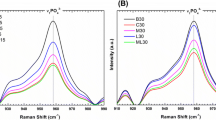
The aim of this study was to evaluate the osseointegration of implants placed in areas grafted with different osteoconductive bone substitutes irradiated with infrared low-level laser therapy (LLLT). Fifty-six rats were randomly allocated into 4 groups: DBB, bone defects filled with deproteinized bovine bone graft (DBB); HA/TCP, bone defects filled with biphasic ceramic made of hydroxyapatite and β-tricalcium phosphate (HA/TCP); DBB-L, bone defects filled with DBB and treated by LLLT; HA/TCP-L, bone defects filled with HA/TCP and treated by LLLT. Bone defects were performed in the tibia of each animal and filled with the different biomaterials. The grafted areas were treated with LLLT (λ 808 nm, 100 mW, ϕ ∼ 0.60 mm) in 7 sessions with 48 h between the irradiations. After the 60-day period, the implants were placed, and the animals were euthanized after 15 and 45 days. The osseointegration and bone repair in the grafted area were evaluated by biomechanical, microtomographic and histometric analyses, and the expression of some bone biomarkers was evaluated by immunohistochemistry analysis. LLLT induced higher degree of osseointegration, which was associated with the greater expression of BMP2 and OCN. LLLT performed in areas grafted with osteoconductive bone substitutes prior to implant placement improves osseointegration.





Similar content being viewed by others
References
Ravald N, Dahlgren S, Teiwik A, Grondahl K (2013) Long-term evaluation of Astra tech and Branemark implants in patients treated with full-arch bridges. Results after 12–15 years. Clin Oral Implants Res 24:1144–1151. https://doi.org/10.1111/j.1600-0501.2012.02524.x
Sherif S, Susarla SM, Hwang JW, Weber HP, Wright RF (2011) Clinician- and patient-reported long-term evaluation of screw- and cement-retained implant restorations: a 5-year prospective study. Clin Oral Investig 15:993–999. https://doi.org/10.1007/s00784-010-0460-4
Papageorgiou SN, Papageorgiou PN, Deschner J, Gotz W (2016) Comparative effectiveness of natural and synthetic bone grafts in oral and maxillofacial surgery prior to insertion of dental implants: systematic review and network meta-analysis of parallel and cluster randomized controlled trials. J Dent 48:1–8. https://doi.org/10.1016/j.jdent.2016.03.010
Sanz-Sanchez I, Ortiz-Vigon A, Sanz-Martin I, Figuero E, Sanz M (2015) Effectiveness of lateral bone augmentation on the alveolar crest dimension: a systematic review and meta-analysis. J Dent Res 94:128S–142S. https://doi.org/10.1177/0022034515594780
Garcia-Gareta E, Coathup MJ, Blunn GW (2015) Osteoinduction of bone grafting materials for bone repair and regeneration. Bone 81:112–121. https://doi.org/10.1016/j.bone.2015.07.007
Spin-Neto R, Stavropoulos A, Coletti FL, Pereira LA, Marcantonio E Jr, Wenzel A (2015) Remodeling of cortical and corticocancellous fresh-frozen allogeneic block bone grafts--a radiographic and histomorphometric comparison to autologous bone grafts. Clin Oral Implants Res 26:747–752. https://doi.org/10.1111/clr.12343
Nkenke E, Neukam FW (2014) Autogenous bone harvesting and grafting in advanced jaw resorption: morbidity, resorption and implant survival. Eur J Oral Implantol 7(Suppl 2):S203–S217
Froum SJ, Wallace SS, Cho SC, Elian N, Tarnow DP (2008) Histomorphometric comparison of a biphasic bone ceramic to an organic bovine bone for sinus augmentation: 6- to 8-month postsurgical assessment of vital bone formation. A pilot study. Int J Periodontics Restorative Dent 28:273–281
Mardas N, Chadha V, Donos N (2010) Alveolar ridge preservation with guided bone regeneration and a synthetic bone substitute or a bovine-derived xenograft: a randomized, controlled clinical trial. Clin Oral Implants Res 21:688–698. https://doi.org/10.1111/j.1600-0501.2010.01918.x
Danesh-Sani SA, Wallace SS, Movahed A, El Chaar ES, Cho SC, Khouly I, Testori T (2016) Maxillary sinus grafting with biphasic bone ceramic or autogenous bone: clinical, histologic, and histomorphometric results from a randomized controlled clinical trial. Implant Dent 25:588–593. https://doi.org/10.1097/ID.0000000000000474
Carmagnola D, Adriaens P, Berglundh T (2003) Healing of human extraction sockets filled with bio-Oss. Clin Oral Implants Res 14:137–143
Barallat L, Ruiz-Magaz V, Levi PA Jr, Mareque-Bueno S, Galindo-Moreno P, Nart J (2014) Histomorphometric results in ridge preservation procedures comparing various graft materials in extraction sockets with nongrafted sockets in humans: a systematic review. Implant Dent 23:539–554. https://doi.org/10.1097/ID.0000000000000124
Meloni SM, Jovanovic SA, Lolli FM, Cassisa C, De Riu G, Pisano M, Lumbau A, Luglie PF, Tullio A (2015) Grafting after sinus lift with anorganic bovine bone alone compared with 50:50 anorganic bovine bone and autologous bone: results of a pilot randomised trial at one year. Br J Oral Maxillofac Surg 53:436–441. https://doi.org/10.1016/j.bjoms.2015.02.012
Kim SJ, Shin HS, Shin SW (2010) Effect of bone block graft with rhBMP-2 on vertical bone augmentation. Int J Oral Maxillofac Surg 39:883–888. https://doi.org/10.1016/j.ijom.2010.05.004
Lin GH, Lim G, Chan HL, Giannobile WV, Wang HL (2016) Recombinant human bone morphogenetic protein 2 outcomes for maxillary sinus floor augmentation: a systematic review and meta-analysis. Clin Oral Implants Res 27:1349–1359. https://doi.org/10.1111/clr.12737
Jakse N, Payer M, Tangl S, Berghold A, Kirmeier R, Lorenzoni M (2007) Influence of low-level laser treatment on bone regeneration and osseointegration of dental implants following sinus augmentation. An experimental study on sheep. Clin Oral Implants Res 18:517–524. https://doi.org/10.1111/j.1600-0501.2007.01369.x
Mayer L, Gomes FV, Carlsson L, Gerhardt-Oliveira M (2015) Histologic and resonance frequency analysis of Peri-implant bone healing after low-level laser therapy: an in vivo study. Int J Oral Maxillofac Implants 30:1028–1035. https://doi.org/10.11607/jomi.3382
Pereira CL, Sallum EA, Nociti FH Jr, Moreira RW (2009) The effect of low-intensity laser therapy on bone healing around titanium implants: a histometric study in rabbits. Int J Oral Maxillofac Implants 24:47–51
Franco GR, Laraia IO, Maciel AA, Miguel NM, Dos Santos GR, Fabrega-Carvalho CA, Pinto CA, Pettian MS, Cunha MR (2013) Effects of chronic passive smoking on the regeneration of rat femoral defects filled with hydroxyapatite and stimulated by laser therapy. Injury 44:908–913. https://doi.org/10.1016/j.injury.2012.12.022
Marquez Martinez ME, Pinheiro AL, Ramalho LM (2008) Effect of IR laser photobiomodulation on the repair of bone defects grafted with organic bovine bone. Lasers Med Sci 23:313–317. https://doi.org/10.1007/s10103-007-0488-0
Pinheiro AL, Martinez Gerbi ME, de Assis Limeira F Jr, Carneiro Ponzi EA, Marques AM, Carvalho CM, de Carneiro Santos R, Oliveira PC, Noia M, Ramalho LM (2009) Bone repair following bone grafting hydroxyapatite guided bone regeneration and infra-red laser photobiomodulation: a histological study in a rodent model. Lasers Med Sci 24:234–240. https://doi.org/10.1007/s10103-008-0556-0
Soares LG, Magalhaes EB, Magalhaes CA, Ferreira CF, Marques AM, Pinheiro AL (2013) New bone formation around implants inserted on autologous and xenografts irradiated or not with IR laser light: a histomorphometric study in rabbits. Braz Dent J 24:218–223. https://doi.org/10.1590/0103-6440201302186
Garcia VG, da Conceicao JM, Fernandes LA, de Almeida JM, Nagata MJ, Bosco AF, Theodoro LH (2013) Effects of LLLT in combination with bisphosphonate on bone healing in critical size defects: a histological and histometric study in rat calvaria. Lasers Med Sci 28:407–414. https://doi.org/10.1007/s10103-012-1068-5
Park JJ, Kang KL (2012) Effect of 980-nm GaAlAs diode laser irradiation on healing of extraction sockets in streptozotocin-induced diabetic rats: a pilot study. Lasers Med Sci 27:223–230. https://doi.org/10.1007/s10103-011-0944-8
de Oliveira G, Aroni MAT, Medeiros MC, Marcantonio E Jr, Marcantonio RAC (2018) Effect of low-level laser therapy on the healing of sites grafted with coagulum, deproteinized bovine bone, and biphasic ceramic made of hydroxyapatite and beta-tricalcium phosphate. In vivo study in rats. Lasers Surg Med. https://doi.org/10.1002/lsm.22787
de Oliveira GJ, de Paula LG, Spin-Neto R, Stavropoulos A, Spolidorio LC, Marcantonio E Jr, Marcantonio RA (2014) Effect of avocado/soybean unsaponifiables on osseointegration: a proof-of-principle preclinical in vivo study. Int J Oral Maxillofac Implants 29:949–957. https://doi.org/10.11607/jomi.3498
de Vasconcellos LM, Barbara MA, Deco CP, Junqueira JC, do Prado RF, Anbinder AL, de Vasconcellos LG, Cairo CA, Carvalho YR (2014) Healing of normal and osteopenic bone with titanium implant and low-level laser therapy (GaAlAs): a histomorphometric study in rats. Lasers Med Sci 29:575–580. https://doi.org/10.1007/s10103-013-1326-1
Campanha BP, Gallina C, Geremia T, Loro RC, Valiati R, Hubler R, de Oliveira MG (2010) Low-level laser therapy for implants without initial stability. Photomed Laser Surg 28:365–369. https://doi.org/10.1089/pho.2008.2429
Khadra M, Ronold HJ, Lyngstadaas SP, Ellingsen JE, Haanaes HR (2004) Low-level laser therapy stimulates bone-implant interaction: an experimental study in rabbits. Clin Oral Implants Res 15:325–332. https://doi.org/10.1111/j.1600-0501.2004.00994.x
Verzola MH, Frizzera F, de Oliveira GJ, Pereira RM, Rodrigues-Filho UP, Nonaka KO, Orrico SR (2015) Effects of the long-term administration of alendronate on the mechanical properties of the basal bone and on osseointegration. Clin Oral Implants Res 26:1466–1475. https://doi.org/10.1111/clr.12492
Rasouli Ghahroudi AA, Rokn AR, Kalhori KA, Khorsand A, Pournabi A, Pinheiro AL, Fekrazad R (2014) Effect of low-level laser therapy irradiation and bio-Oss graft material on the osteogenesis process in rabbit calvarium defects: a double blind experimental study. Lasers Med Sci 29:925–932. https://doi.org/10.1007/s10103-013-1403-5
Torres CS, dos Santos JN, Monteiro JS, Amorim PG, Pinheiro AL (2008) Does the use of laser photobiomodulation, bone morphogenetic proteins, and guided bone regeneration improve the outcome of autologous bone grafts? An in vivo study in a rodent model. Photomed Laser Surg 26:371–377. https://doi.org/10.1089/pho.2007.2172
Barbosa D, de Souza RA, Xavier M, da Silva FF, Arisawa EA, Villaverde AG (2013) Effects of low-level laser therapy (LLLT) on bone repair in rats: optical densitometry analysis. Lasers Med Sci 28:651–656. https://doi.org/10.1007/s10103-012-1125-0
Gerbi ME, Marques AM, Ramalho LM, Ponzi EA, Carvalho CM, Santos Rde C, Oliveira PC, Noia M, Pinheiro AL (2008) Infrared laser light further improves bone healing when associated with bone morphogenic proteins: an in vivo study in a rodent model. Photomed Laser Surg 26:55–60. https://doi.org/10.1089/pho.2007.2026
Mandal CC, Das F, Ganapathy S, Harris SE, Choudhury GG, Ghosh-Choudhury N (2016) Bone morphogenetic protein-2 (BMP-2) activates NFATc1 transcription factor via an autoregulatory loop involving Smad/Akt/Ca2+ signaling. J Biol Chem 291:1148–1161. https://doi.org/10.1074/jbc.M115.668939
Tsao YT, Huang YJ, Wu HH, Liu YA, Liu YS, Lee OK (2017) Osteocalcin mediates biomineralization during osteogenic maturation in human mesenchymal stromal cells. Int J Mol Sci 18. https://doi.org/10.3390/ijms18010159
Freddo AL, Rodrigo SM, Massotti FP, Etges A, de Oliveira MG (2009) Effect of low-level laser therapy after implantation of poly-L-lactic/polyglycolic acid in the femurs of rats. Lasers Med Sci 24:721–728. https://doi.org/10.1007/s10103-008-0627-2
Esnouf A, Wright PA, Moore JC, Ahmed S (2007) Depth of penetration of an 850nm wavelength low level laser in human skin. Acupunct Electrother Res 32:81–86
Acknowledgements
The authors would like to thank the laboratory technicians Leandro Alves dos Santos and Ana Claudia Gregolin Costa Miranda for their technical support during the histological analysis. This study was financed by the Brazilian agencies FAPESP (Fundação de Amparo a pesquisa do Estado de São Paulo, 2013/24318-0) and CNPq (Conselho Nacional de Desenvolvimento Científico e Tecnológico, 459984/2014-4).
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
Conflict of interest
The authors declare that they have no conflict(s) of interest.
Additional information
Publisher’s note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Rights and permissions
About this article
Cite this article
de Oliveira, G.J.P.L., Aroni, M.A.T., Pinotti, F.E. et al. Low-level laser therapy (LLLT) in sites grafted with osteoconductive bone substitutes improves osseointegration. Lasers Med Sci 35, 1519–1529 (2020). https://doi.org/10.1007/s10103-019-02943-w
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s10103-019-02943-w