Abstract
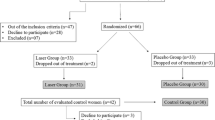
Myofacial pain dysfunction syndrome (MPDS) is the most common reason for pain and limited function of the masticatory system. The effects of low-level lasers (LLLs) for controlling the discomfort of patients are investigated frequently. However, the aim of this study was to evaluate the efficacy of a particular source producing 660 nm and 890 nm wavelengths that was recommended to reduce of the pain in the masticatory muscles. This was a double-blind and placebo-controlled trial. Sixteen MPDS patients were randomly divided into two groups. For the laser group, two diode laser probes (660 nm (nanometers), 6.2 J/cm2, 6 min, continuous wave, and 890 nm, 1 J/cm2 (joules per square centimetre), 10 min, 1,500 Hz (Hertz)) were used on the painful muscles. For the control group, the treatment was similar, but the patients were not irradiated. Treatment was given twice a week for 3 weeks. The amount of patient pain was recorded at four time periods (before and immediately after treatment, 1 week after, and on the day of complete pain relief). A visual analog scale (VAS) was selected as the method of pain measurement. Repeated-measures analysis of variance (ANOVA), the t-test and the paired t-test were used to analyze the data. In each group the reduction of pain before and after the treatment was meaningful, but, between the two groups, low-level laser therapy (LLLT) was more effective (P = 0.031) According to this study, this type of LLLT was the effective treatment for pain reduction in MPDS patients.




Similar content being viewed by others
References
Blasberg B, Greenberg MS (2008) Temporomandibular disorders In: Greenberg MS, Glick M, Ship JA(ed) Burket’s oral medicine, 11th edn. BC Decker, Hamilton, Ontario, pp 223–255
Miloro M, Ghali GE, Larsen PE, Waite PD(2004) Peterson’s principles of oral and maxillofacial surgery, 2nd edn, vol 2. BC Decker, Hamilton, Ontario, Canada, pp 931–1014
Okeson JP. (2003) Management of temporomandibular disorders and occlusion, 5th edn. Mosby, St. Louis
Fikácková H, Dostálová T, Navrátil L, Klaschka J (2007) Effectiveness of low-level laser therapy in temporomandibular joint disorders: a placebo-controlled study. Photomed Laser Surg 25:297–303
Mazzetto MO, Carrasco TG, Bidinelo EF, de Andrade Pizzo RC, Mazzetto RG (2007) Low intensity laser application in temporomandibular disorders: a phase I double- blind study. J Craniomandib Pract 25:186–192
Cetiner S, Kahraman SA, Yücetaş S (2006) Evaluation of low-level laser therapy in the treatment of temporomandibular disorders. Photomed Laser Surg 24:637–641
Kulekcioglu S, Sivrioglu K, Ozcan O, Parlak M (2003) Effectiveness of low-level laser therapy in temporomandibular disorder. Scand J Rheumatol 32:114–118
Emshoff R, Bösch R, Pümpel E, Schöning H, Strobl H (2008) Low-level laser therapy for treatment of temporomandibular joint pain: a double-blind and placebo-controlled trial. Oral Surg Oral Med Oral Pathol Oral Radiol Endod 105:452–456
Abreu Venancio R, Camparis CM, Fátima Zanirato Lizarelli R (2005) Low intensity laser therapy in the treatment of temporomandibular disorders: a double-blind study. J Oral Rehabil 32:800–807
Conti PC (1997) Low level laser therapy in the treatment of temporomandibular disorders (TMD): a double-blind pilot study. J Craniomandib Pract 15:144–149
Hansen HJ, Thorøe U (1990) Low power laser biostimulation of chronic oro-facial pain. A double-blind placebo controlled cross-over study in 40 patients. Pain 43:169–179
Tunér J, Hode L (2004) The laser therapy handbook. Prima Books, Grängesberg, pp 236–240
Bertolucci LE, Grey T (1995) Clinical analysis of mid-laser versus placebo treatment of arthralgic TMJ degenerative joints. J Craniomandib Pract 13:26–29
Kogawa EM, Kato MT, Santos CN, Conti PCR (2005) Evaluation of the efficacy of low-level laser therapy (LLLT) and the micro electric neurostimulation (MENS) in the treatment of myogenic temporomandibular disorders: a randomized clinical trial. J Appl Oral Sci 13:280–285
De Medeiros JS, Vieira GF, Nishimura PY (2005) Laser application effects on the bite strength of the masseter muscle, as an orofacial pain treatment. Photomed Laser Surg 23:373–376
Núñez SC, Carcez AS, Suzuki SS, Ribeiro MS (2006) Management of mouth opening in patients with temporomandibular disorders through low level laser therapy and transcutaneous electrical neural stimulation. Photomed Laser Surg 24:45–49
Hansson T (1989) Infrared laser in the treatment of craniomandibular disorders, arthrogenous pain. J Prosthet Dent 61:614–617
Walsh LJ, Goharkhay K, Verheyen P, Mortiz A (2006) Low level laser therapy. In: Mortiz A (ed) Oral laser application. Quintessenz, Berlin, pp 521–537
Kamenova J (2004) Treatment of occlusal traumatic symptoms using low power laser irradiation. J Oral Laser Appl 4:29–41
Conti PC (1997) low level laser therapy in the treatment of temporomandibular disorders (TMD): a double blind pilot study. J Craniomandib Pract 15:144–149
Kim K, Kim Y (1988) Comparative study of the clinical effects of splint, laser acupuncture and laser therapy for temporomandibular disorders. J Dent Coll Seoul Natl Univ 1:195–201
Kim S-Y, Park J-S (1996) The effect of low level laser therapy at the trigger points in masseter and other muscles. J Korean Acad Oral Med 21:1–3
Gray RJ, Quayle AA, Hall CA, Schofield MA (1994) Physiotherapy in the treatment of temporomandibular joint disorders: a comparative study of four treatment methods. Br Dent J 176:257–261
Passarella S (1989) He-Ne laser irradiation of isolated mitochondria. J Photochem Photobiol 3:642–643
Yu W, Naim JO, McGowan M, Ippolito K, Lanzafame RJ (1997) Photomodulation of oxidative metabolism and electron chain enzymes in rat liver mitochondria. Photochem Photobiol 66:866–871
Walker JB (1983) Relief from chronic pain by low power laser irradiation. Neurosci Lett 43:339–344
Yamamoto H, Ozaki A, Iguchi N, Kinochita S (1988) Antinociceptive effects of laser irradiation of Hoku point in rats. Pain Clin 8:43–48
Ailioaie C, Lupusoru-Ailioaie LM (1999) Beneficial effects of laser therapy in the early stages of rheumatoid arthritis onset. Laser Ther 11:79–87
Mester E, Mester AF, Mester A (1985) The biomedical effects of laser application. Lasers Surg Med 5:31–39
Kemmotsu O, Sato K, Furumido H, Harada K, Takigawa C, Kaseno S et al (1991) Efficacy of low reactive-level laser therapy for pain attenuation of postherpetic neuralgia. Laser Ther 3:71–75
Schindl A, Schindl M, Schon H, Knobler R, Havelec LO, Schindl L (1998) Low intensity laser improves skin circulation in patients with diabetic microangiopathy. Diabetes Care 21:390–394
Mannheimer JS (2007) Limited evidence to support the use of physical therapy for temporomandibular disorder. Evid Based Dent 8:110–111
Bradley P, Tuner J (2007) Laser phototherapy in dentistry In: Gutknecht N et al (eds) Proceedings of the 1st International Workshop of Evidence Based Dentistry on Lasers in Dentistry. Quintessence, Surrey, UK, pp 1–24
Author information
Authors and Affiliations
Corresponding author
Rights and permissions
About this article
Cite this article
Shirani, A.M., Gutknecht, N., Taghizadeh, M. et al. Low-level laser therapy and myofacial pain dysfunction syndrome: a randomized controlled clinical trial. Lasers Med Sci 24, 715–720 (2009). https://doi.org/10.1007/s10103-008-0624-5
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s10103-008-0624-5