Abstract
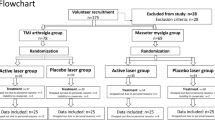
Women with temporomandibular disorders (TMD) frequently report pain areas in body regions. This process is associated with central sensitization phenomena, present in chronic pain. The low-level laser therapy (LLLT) has been reported as a therapeutic option for the painful TMD treatment. The aim of this study was to analyze the effect of LLLT on pain intensity (visual analogue scale, VAS), pain sensitivity in orofacial and corporal points (pressure pain threshold, PPT), and on Short Form-McGill Pain Questionnaire (SF-MPQ) indexes of women with myofascial pain (subtype of muscle TMD). Ninety-one women (18–60 years) were included in the study, among which 61 were diagnosed with myofascial pain (Research Diagnostic Criteria for Temporomandibular Disorder—Ia and Ib) and were divided into laser (n = 31) and placebo group (n = 30), and 30 were controls. The LLLT was applied at pre-established points, twice a week, eight sessions (780 nm; masseter and anterior temporal = 5 J/cm2, 20 mW, 10 s; TMJ area = 7.5 J/cm2, 30 mW, 10 s). Pain intensity, pain sensitivity, and the SF-MPQ indexes were measured at the baseline, during laser sessions, and 30 days after treatment. For intra-group comparisons, the Friedman test was performed, and for inter-group, the Mann-Whitney test. Increased pain sensitivity was found in women with myofascial pain when compared to controls (p < 0.05). There was a reduction in pain intensity for both groups after LLLT. The LLLT did not change the PPT for any group (p > 0.05). Active laser and placebo reduced the indexes of sensory, total pain, and VAS, maintaining the results after 30 days; there was a reduction in the affective pain rating index for both groups, with no maintenance after 30 days for placebo, and the present pain intensity decreased in the laser group and did not change in the placebo after LLLT. In conclusion, the LLLT active or placebo are effective in reducing the overall subjective perception of myofascial pain (VAS and SF-MPQ indexes); however, they have no effectiveness in reducing the pain sensitivity in orofacial and corporal points (PPT increase).



Similar content being viewed by others
References
De Leeuw R, Klasser GD (2013) Orofacial pain: guidelines for assessment, diagnosis and management. Quintessense: Chicago
Scrivani SJ, Keith DA, Kaban LB (2008) Temporomandibular disorders. N Engl J Med 359(25):2693–705
Ribeiro Da Silva MC, Fillingim RB, Wallet SM (2016) Estrogen-induced monocytic response correlates with temporomandibular disorder pain: a case control study. J Dent Res. doi: 0022034516678599
Aaron LA, Buchwald D (2003) Chronic diffuse musculoskeletal pain, fibromyalgia and co-morbid unexplained clinical conditions. Best Pract Res Clin Rheumatol 17:563–574
Fernández-de-las-Peñas C, Galán-del-Río F, Fernández-Carnero J, Pesquera J, Arendt-Nielsen L, Svensson P (2009) Bilateral widespread mechanical pain sensitivity in women with myofascial temporomandibular disorder: evidence of impairment in central nociceptive processing. J Pain 10(11):1170–8
Lim PF et al (2010) Development of temporomandibular disorders is associated with greater bodily pain experience. Clin J Pain 26:116–120
Da Cunha CO et al (2014) Determination of a pressure pain threshold cut-off value for the diagnosis of temporomandibular joint arthralgia. J Oral Rehabil 41(5):323–329
Carlsson AM (1983) Assessment of chronic pain, aspects of the reliability and validity of the visual analogue scale. Pain 16:87–101
Price DD et al (1994) A comparison of pain measurement characteristics of mechanical visual analogue and simple numerical rating scales. Pain 56:217–226
Ohrbach R, Gale EM (1989) Pressure pain threshold, clinical assessment, and differential diagnosis: reliability and validity in patients with myogenic pain. Pain 39:157–169
Santos Silva RS et al (2005) Pressure pain threshold in the detection of masticatory myofascial pain: an algometer-based study. J Orofac Pain 19(4):318–324
Melzack R (1975) The McGill Pain Questionnaire: major properties and scoring methods. Pain 1:277–99
Menezes Costa L da C et al (2011) The Brazilian-Portuguese versions of the McGill Pain Questionnaire were reproducible, valid, and responsive in patients with musculoskeletal pain. J Clin Epidemiol 64(8):903-912.
Ferreira KA, de Andrade DC, Teixeira MJ (2013) Development and validation of a Brazilian version of the short-form McGill pain questionnaire (SF-MPQ). Pain Manag Nurs 14(4):210–219
Cetiner S, Kahraman SA, Yücetaş S (2006) Evaluation of low-level laser therapy in the treatment of temporomandibular disorders. Photomed Laser Surg 24(5):637–641
Fikácková H et al (2007) Effectiveness of low-level laser therapy in temporomandibular joint disorders: a placebo-controlled study. Photomed Laser Surg 25(4):297–303
Emshoff R et al (2008) Low-level laser therapy for treatment of temporomandibular joint pain: a double-blind and placebo-controlled trial. Oral Surg Oral Med Oral Pathol Oral Radiol Endod 105(4):452–456
Melchior MO et al (2013) Does low intensity laser therapy reduce pain and change orofacial myofunctional conditions? Cranio 31(2):133–139
Ahrari F et al (2014) The efficacy of low-level laser therapy for the treatment of myogenous temporomandibular joint disorder. Lasers Med Sci 29(2):551–557
Gao X, Xing D (2009) Molecular mechanisms of cell proliferation induced by low power laser irradiation. J Biomed Sci 16:1–16
Carrasco TG et al (2008) Low intensity laser therapy in temporomandibular disorder: a phase II double-blind study. Cranio 26(4):274–281
Da Silva MAMR et al (2012) Low level laser therapy as na adjunctive technique in the management of temporomandibular disorders. Cranio 30(4):264–71
De Moraes Maia ML et al (2014) Evaluation of low-level laser therapy effectiveness on the pain and masticatory performance of patients with myofascial pain. Lasers Med Sci 29(1):29–35
Da Cunha LA et al (2008) Efficacy of low-level laser therapy in the treatment of temporomandibular disorder. Int Dent J 58(4):213–217
Petrucci A et al (2011) Effectiveness of low-level laser therapy in temporomandibular disorders: a systematic review and meta-analysis. J Orofac Pain 25(4):298–307
Chen J et al (2015) Efficacy of low-level laser therapy in the treatment of TMDs: a meta-analysis of 14 randomised controlled trials. J Oral Rehabil 42(4):291–299
De Moraes Maia ML et al (2012) Effect of low-level laser therapy on pain levels in patients with temporomandibular disorders: a systematic review. J Appl Oral Sci 20(6):594–602
Schiffman EL et al (2010) The Research Diagnostic Criteria for Temporomandibular Disorders. V: methods used to establish and validate revised Axis I diagnostic algorithms. J Orofac Pain 24:63–78
Bragdon EE et al (2002) Group differences in pain modulation: pain-free women compared to pain-free men and to women with TMD. Pain 96(3):227–237
Fishbain DA, Lewis JE, Gao J (2012) Is there significant correlation between self-reported low back pain visual analogic scores and low back pain scores determined by pressure pain induction matching? Pain Pract 13:358–363
Wolfe F et al (1990) The American College of Rheumatology 1990 criteria for the classification of fibromyalgia: report of the Multicenter Criteria Committee. Arthritis Rheum 33:160–172
Sancakli E et al (2015) Early results of low-level laser application for masticatory muscle pain: a double-blind randomized clinical study. BMC Oral Health 15(1):131–136
Desiderá AC et al (2015) Laser therapy reduces gelatinolytic activity in the rat trigeminal ganglion during temporomandibular joint inflammation. Oral Dis 21(5):652–658
Do Nascimento GC, Leite-Panissi CR (2014) Time-dependent analysis of nociception and anxiety-like behavior in rats submitted to persistent inflammation of the temporomandibular joint. Physiol Behav 125:1–7
Lund I et al (2005) Lack of interchangeability between visual analogue and verbal rating pain scales: a cross sectional description of pain etiology groups. BMC Med Res Methodol 5:31–36
Chouchou F, Lavigne GJ (2014) Placebo analgesia and sleep. Pathol Biol 62(5):270–275
Gourion D, Mouchabac S (2016) Placebo effect: clinical, biological and therapeutical involvements in depression. Encéphale 42:24–30
Vedolin GM et al (2009) The impact of stress and anxiety on the pressure pain threshold of myofascial pain patients. J Oral Rehabil 36(5):313–321
Sanches ML et al (2015) Correlation between pressure pain threshold and pain intensity in patients with temporomandibular disorders who are compliant or non-compliant with conservative treatment. Oral Surg Oral Med Oral Pathol Oral Radiol 120(4):459–468
Lauche R et al (2014) Neck pain intensity does not predict pressure pain hyperalgesia: re-analysis of seven randomized controlled trials. J Rehabil Med 46(6):553–560
Latremoliere A, Woolf CJ (2009) Central sensitization: a generator of pain hypersensitivity by central neural plasticity. J Pain 10(9):895–926
Drobek W, De Laat A, Schoenaers J (2001) Tactile threshold and pressure pain threshold during treatment of orofacial pain: an explorative study. Clin Oral Investig 5(3):185–193
Slade GD et al (2014) Pressure pain thresholds fluctuate with, but do not usefully predict, the clinical course of painful temporomandibular disorder. Pain 55(10):2134–2143
Greenspan JD et al (2013) Pain sensitivity and autonomic factors associated with development of TMD: the OPPERA prospective cohort study. J Pain 14:63–74
Cao Y, Chen HM, Fu KY (2008) Investigation on clinical pain features in temporomandibular disorders. Zhonghua Kou Qiang Yi Xue Za Zhi 43(5):293–295
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
Conflict of interest
The authors declare that they have no conflict of interest.
Funding source
This study was financially supported by São Paulo Research Foundation (FAPESP) and Coordination for the Improvement of Higher Education Personnel (CAPES).
Ethical approval and informed consent
All procedures were performed in accordance with the guidelines of the Brazilian Ethics Committee on Human Research. This study was conducted after approval by the Ethics Committee of the School of Dentistry of Ribeirão Preto (under protocol: 33658114.7.0000.5419). All subjects were informed about the study and signed a consent form (approved by the Ethics Committee). Patients who composed the placebo group and did not have pain reduction after the study completion were invited to receive treatment with LLLT, in the same parameters of the active laser group.
Rights and permissions
About this article
Cite this article
Magri, L.V., Carvalho, V.A., Rodrigues, F.C.C. et al. Effectiveness of low-level laser therapy on pain intensity, pressure pain threshold, and SF-MPQ indexes of women with myofascial pain. Lasers Med Sci 32, 419–428 (2017). https://doi.org/10.1007/s10103-016-2138-x
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s10103-016-2138-x