Abstract
For a long time, hand, foot and mouth disease (HFMD) was seen as a mild viral infection characterized by typical clinical manifestations that spontaneously resolved in a few days without complications. In the past two decades, HFMD has received new attention because of evidence that this disease could have clinical, epidemiological and aetiological characteristics quite different from those initially thought. In contrast to previous beliefs, it has been clarified that HFMD can be associated with complications, leading to severe neurological sequelae and, rarely, to death. This finding has led to an enormous number of studies that have indicated that several viruses in addition to those known to be causes of HFMD could be associated with the development of disease. Moreover, it was found that if some viruses were more common in some geographic areas, frequent modification of the molecular epidemiology of the infecting strains could lead to outbreaks caused by infectious agents significantly different from those previously circulating. Vaccines able to confer protection against the most common aetiologic agents in a given country have been developed. However, simultaneous circulation of more than one causative virus and modification of the molecular epidemiology of infectious agents make preparations based on a single agent relatively inadequate. Vaccines with multiple components are a possible solution. However, several problems concerning their development must be solved before adequate prevention of severe cases of HFMD can be achieved.
Similar content being viewed by others
Introduction
Hand, foot and mouth disease (HFMD) was first described in 1948 [1]. For a long time, no particular attention was paid to this disease because it was seen as a mild viral infection characterized by typical clinical manifestations that spontaneously resolved in a few days without complications. In the past two decades, HFMD has received new attention because of evidence that this disease could have clinical, epidemiological and aetiological characteristics quite different from those initially thought. There is evidence that a substantial number of cases could have atypical manifestations [2]. Moreover, several outbreaks of HFMD, involving millions of children, particularly in the Western Pacific Region, have been described [3]. Furthermore, there is evidence that some enteroviruses (EVs), already known as causes of very severe diseases, could be the aetiologic agents of HFMD [4]. Severe neurologic and cardiorespiratory problems have been associated with HFMD, which in some cases, could result in death [5]. Thus, research on HFMD has significantly increased, and attempts have been made to develop drugs [6] and vaccines [7] against the EVs associated with the most severe cases of HFMD. In recent years, knowledge on HFMD has significantly increased. The main aim of this paper is to discuss the most recent literature pertaining to HFMD, emphasizing epidemiology, characteristics of aetiologic agents and vaccine development.
Epidemiology
HFMD epidemiology only receives attention in regions where the disease is endemic and a number of severe cases have occurred. The Western Pacific World Health Organization (WHO) Region is the best example. In most of the countries included in this area, specific surveillance systems have been activated, and in some cases, notification of health authorities regarding disease has become mandatory. For example, in China, the country with the highest number of inhabitants and with one of the most advanced surveillance systems, HFMD has been categorized as a notifiable disease since 2008, and characteristics of infectious agents are continuously monitored [8]. During the period from May 2008 to June 2014, a total of 10,717,283 HFMD cases were reported in China, with 3046 deaths and a fatality rate of 0.03%. Among survivors, morbidity increased from 37.6/100,000 in 2008 to 139.6/100,000 in 2013 and peaked in 2012 at 166.8/100,000 [8]. More than 90% of the cases were diagnosed in children < 5 years of age. Mortality was higher among those ≤ 2 years old; 84.02% of the deaths occurred in this age group, indicating that susceptibility and severity of HFMD are associated with age [9]. Among other potentially associated factors, sex was not found to be associated with susceptibility but was found to be associated with disease severity. Infection rates are similar in males and females [10, 11], but males are more likely to develop symptoms, to have diffuse infections and to need medical assistance [12,13,14,15]. Moreover, poor hygiene and social contacts are associated with the development of HFMD [16]. Finally, in some cases, meteorological factors such as high temperature and humidity have been associated with HFMD susceptibility. It was found that in temperate regions of Asia, HFMD is more common during the late spring and early summer [17,18,19,20,21], whereas in tropical and subtropical Asia, outbreaks typically occur in the late spring and fall [22,23,24,25]. However, in other Asian regions, such as Thailand [26], Vietnam [27], Malaysia [28] and Singapore [29], an association with temperature and humidity cannot be demonstrated, and outbreaks occur throughout the year.
In Europe and America, the incidence of HFMD is not continuously monitored. Surveillance for EV infection occurs in several countries through passive systems that rely on voluntary participation from laboratories and collect information regarding hospitalized patients generally suffering from severe diseases [30]. These systems are designed to monitor EV circulation and the association between viral strains and severe disease rather than the incidence of the different EV-related diseases. Only outbreaks of HFMD characterized by a large number of severe cases are monitored, and the frequency of reports is greatly influenced by increased awareness and demand for testing during outbreak periods. A more sensitive method has been adopted in France; in 2010, France implemented a sentinel surveillance system run by paediatricians in ambulatory care settings that was effective in detecting HFMD outbreaks and the associated EV serotypes. This system was initially limited to a small geographic area [31] but has been extended to cover all of France [32]. However, even the most effective surveillance methods do not allow for the evaluation of the true epidemiology of HFMD. Underreporting is the rule because a substantial number of HFMD cases have atypical manifestations and are not correctly diagnosed.
Aetiology
HFMD is a disease caused by EVs from a genus of positive-sense single-stranded RNA virus members of the Picornaviridae family that, on the basis of genetic characteristics, are divided into four species (EV-A, EV-B, EV-C and EV-D). Each of these species includes several types [33]. Types responsible for HFMD belong to species A in more than 90% of cases [31]. The remaining cases were mainly due to coxsackievirus (CV)-B2 and CV-B5 until a few years ago [34]. However, recently, CV-B3 has been on the rise and has caused several outbreaks of HFMD in China and in neighbouring countries [35].
For many years, EV-A71 and CV-A16 were the most common causes of HFMD outbreaks worldwide [36,37,38]. However, recently, CV-A6 and CV-A10 have partially replaced EV-A71 and CV-A16 as the main pathogens associated with HFMD. Several outbreaks of HFMD due to these emerging viruses have been described in Asia, America and Europe since 2010 [39,40,41,42,43,44,45,46,47].
Phylogenetic studies of the different EVs identified during HFMD outbreaks have shown that EV-A71 strains can be divided into three different genotypes, A, B and C, and 11 sub-genotypes, each defined with a number. Most outbreaks were due to genotypes B and C or to a mixture of these genotypes. However, infecting sub-genotypes significantly differed among outbreaks, indicating sequential inter-genotype shifts. In some outbreaks, two or more sub-genotypes have simultaneously circulated, which led to recombination favouring the emergence of new genotypes that became the causes of new outbreaks. Typical in this regard is the recombination between EV-A71 C2 and CV-A8 that was the cause of the emergence of genotype B4, responsible for epidemics in Japan, Taiwan and other countries [48]. In Malaysia, epidemics were due to B4 and C1 during 1998–2000; B4, B5, and C1 during 2002–2003 and C1 and B5 during 2005–2006. In Singapore, the B3, B4 and B5 sub-genotypes were predominant during 1997–1999, 2000–2003 and in 2006–2008, respectively [49]. In other Asian countries, sub-genotype C was the most common. In China, sub-genotype C4, particularly variant C4a, was by far the most frequently detected [50]. In Europe, sub-genotype C1 was common until 2005 but was replaced by C2 after 2007 [51]. Moreover, cases of EV-A71 C4 HFMD have recently been described, suggesting the introduction of this sub-genotype from Asia [52].
CV-A16 has been classified into genotypes A and B. Genotype B was divided into B1 and B2 and again subdivided into B1a, B1b, B1c, B2a, B2b and B2c [53]. B1a and B1b have been the predominant genotypes reported in China and neighbouring regions, including Taiwan, Japan, Vietnam, Thailand, Malaysia and Australia [54].
The CV-A6 strains can be classified into genotypes A–F. Genotypes A, B and E were identified in India, Japan and the USA, whereas genotypes C and D were detected in Japan and China. Genotype F has been detected more recently, mainly in China [55]. However, genetic characterization of CV-A6 variants clearly indicates that more recently detected strains are derived from recombination of previously circulating groups [56].
Four genotypes (A–D) of CV-A10 were identified, and for each of these genotypes, a number of sub-genotypes were detected. In China, genotype B was common until 2008. Later, genotype C emerged. During the same period, this genotype was found in Spain and France [57]. Initially, sub-genotypes 1 and 2 were the most frequent, whereas during 2012, lineages 3 and 4 became more common [58].
However, during several outbreaks, the co-circulation of different viral genotypes and sub-genotypes frequently occurred. Recombination between circulating strains or spontaneous mutations of the viral genome can explain variations in the molecular epidemiology of viruses causing HFMD. Moreover, genetic changes may cause different antigenic properties of sub-genotypes and favour new infections in patients who have already suffered from HFMD.
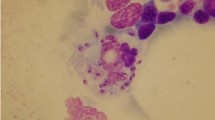
Clinical manifestations
Some of the EV infections that can cause HFMD are asymptomatic. However, the true incidence of asymptomatic infections is not known. Few studies have assessed asymptomatic infections, and the studies that have been conducted have frequently used debatable methodology. Moreover, differences in the virulence of EVs can influence symptom and sign development. However, on the basis of data collected during two prospective studies conducted during a large epidemic of EV-A71 infection, it was concluded that when this EV is circulating, approximately 30% of initially negative subjects seroconvert but do not have any clinical manifestations. This finding suggests that approximately one third of infections remain asymptomatic [59, 60]. The incubation period is thought to be 3–5 days, but qualified sources to confirm this estimate are lacking [3]. Recently collected data seem to indicate that the incubation period may be different in the different paediatric ages. An evaluation of symptom onset and sick absence dates of students diagnosed with HFMD found that the median incubation periods were 4.4 (95% confidence interval [CI] 3.8–5.1) days, 4.7 (95% CI 4.5–5.1) days and 5.7 (95% CI 4.6–7.0) days for children in kindergarten, primary school and secondary school, respectively. More accurate hygiene practices were considered the main reason for the longer incubation period for older children [61].
Symptomatic patients are mainly children < 5 years old. However, adults, particularly those living with infected children, can suffer from HFMD. During epidemics of EV-A6 infection described in Finland [62] and the USA [39], approximately 30% of cases occurred in adults. Patients with classic HFMD have low-grade fever with malaise associated with a maculopapular rash or blisters on the hands, soles and buttocks and painful ulcerative lesions of the throat, mouth and tongue. Fever usually subsides within 48 h, and cutaneous and mucosal lesions disappear in no more than 7–10 days. However, it is relatively common for a patient to exhibit only one or two of these symptoms [63]. Moreover, atypical cutaneous manifestations can occur. Several reports indicate that the emergence of skin lesions with unusual morphology or extent is associated with CV-A6 and, to a lesser extent, with CV-A16, although which virus causes the most relevant manifestations has not been precisely determined [45, 64,65,66]. In a study by Mathes et al., specifically planned to characterize atypical cutaneous presentations in the CVA6-associated North American enterovirus outbreak of 2011–2012, it was found that typical skin lesions in areas not traditionally involved were detectable in more than 60% of the 80 enrolled patients [64]. Moreover, in 55% of children, the eruption was accentuated in areas of previous or active atopic dermatitis. Haemorrhagic or purpuric lesions and an eruption similar to Gianotti-Crosti disease were observed in 17 and 37% of the cases, respectively. Finally, 52% of patients presented with desquamation of their palms or soles 1 to 3 weeks after the initial disease presentation. Generalized vesicular exanthema was reported by Hubiche et al. [66]. Lesions resembling eczema herpeticum or chickenpox were described by Sinclair et al. [45]. Superficial crusted erosions and vesicles symmetrically distributed in the perioral region, in the perianal region, and on the dorsum of the hands were reported by Flet et al. [65]. A late complication of HFMD involves nails. Several days after the onset of traditional HFMD manifestations (up to 40 days), regardless of the EV [67], nail shedding can occur [68]. In other cases, Beau’s lines and onychomadesis can develop. Transient nail matrix arrest is considered to be the main reason for this phenomenon [69]. The isolation of EV in nail fragments seems to indicate that these lesions directly depend on viral replication [70].
However, the most severe complications of HFMD involve the central nervous system (CNS). Aseptic meningitis, acute flaccid paralysis and encephalomyelitis with or without muscle weakness are the most common CNS complications. When the brainstem is damaged, autonomic dysregulation, pulmonary oedema and myocardial impairment leading to death can occur [71]. Patients may recover, but in most cases, survivors develop neurological sequelae such as cognitive and motor disorders [72, 73]. CNS damage is almost exclusively associated with EV-A71 [74, 75], but during recent epidemics, CNS involvement has been found to be associated with 3.6 to 18.2% of EV-A6 HFMD cases, and isolated cases due to other viruses have been reported [40, 76,77,78]. All genotypes and sub-genotypes have been associated with CNS involvement, but for some of them, such as C4 in China, and B3 and B4 in other Asian countries, reports of severe cases have been more common [79]. In Europe, C1 virus was the most common until 2005 but was replaced by C2 after 2007 [51]. However, in 2016, an outbreak of severe EV-A71 disease was described in Spain, and most of the cases were due to the C1 sub-genotype [80]. In India and Africa, D, E and F are the predominant genotypes [81].
The global prevalence of severe CNS involvement in HFMD is unknown. However, data from China’s surveillance system on over 7.2 million cases of HFMD during the period from 2008 to 2012 indicate that the rate of severe neurological or cardiovascular problems was 1.1% [82]. Persistent high fever, increased neutrophil count, male gender, young age and absence of mouth and skin lesions have been found to be risk factors for severe HFMD disease [4, 82]. Moreover, genetics could play a role, as several single-nucleotide polymorphisms of some chemokines such as motif chemokine ligand (CCL)-2, chemokine ligand (CXCL)-10, interleukin (IL)-8, IL-10 and interferon (INF)-γ, have been found to be associated with both susceptibility and severity of EV-A71 infection in the Chinese population [83, 84]. It has been suggested that the potentially negative evolution of brainstem encephalitis is related to the strong systemic and CNS inflammatory response that, together with excessive catecholamine secretion, accompanies CNS infection and leads to cardiotoxicity and pulmonary oedema [85]. A number of proinflammatory cytokines and chemokines have been detected in significant concentrations in the plasma and/or cerebrospinal fluid (CSF) of patients with brainstem encephalitis [86]. Recently, Shang et al. reported that the plasma expression levels of chemokines IL-8, RANTES, monocyte chemoattractant protein (MCP)-1, and IFN-γ-induced protein (IP)-10 and cytokines IL-4, IL-12, IL-18, tumor necrosis factor (TNF)-α and IFN-γ were significantly higher in patients with severe HFMD than in patients with mild HFMD and a control group (p < 0.01) [87]. Moreover, all of these proteins, with the exception of IL-8, were significantly higher in EV-A71-positive patients than in EV-A71-negative patients. These findings seem to indicate that monitoring of cytokines and chemokines in serum or CSF during significantly symptomatic HFMD cases could be useful for identifying subjects at risk of life-threatening disease.
Prevention and treatment
Currently, no approved specific antiviral treatment for HFMD is available. Mild cases are managed with symptomatic measures. Steroids should be avoided because their administration has been found to be associated with an increased risk of severe HFMD development [88]. To treat severe infections, the use of immunoglobulins (IVIG) has been suggested based on evidence of a possible significant benefit through the reduction of the associated CNS inflammatory response. Wang et al. reported that in children with EV71-related brainstem encephalitis complicated by autonomic nervous system dysfunction and pulmonary oedema, the administration of IVIG led to a significant reduction of plasma levels of IFN-γ, IL-6, IL-8, IL-10 and IL-13 [86]. However, the systematic use of IVIG has been debated. First, in vitro studies have found that the IgG3 fraction of human IVIG, in contrast to the IgG 1 and 2 subclasses, does not have neutralizing activity but enhances EV-A71 infection [89]. Moreover, considering the large number of EV types and subtypes that can cause HFMD, it is possible that IVIGs do not contain adequate quantities of antibodies able to neutralize the infecting agent. To at least partially overcome these limitations, monoclonal antibodies have been suggested. However, studies of monoclonal antibodies are just beginning, and although these studies are promising, we are far from having effective preparations [90]. Similar conclusions can be drawn for drugs. Molecules that inhibit viral entry into cells such as suramin [91] or reduce viral replication such as rupintrivir [92] and kaempferol [93] have been investigated. However, only in vitro and experimental studies are available.
Therefore, vaccines remain the best solution to combat HFMD. Several candidate vaccines have been developed [94, 95]. Initially, inactivated whole-virus aluminium-adjuvant vaccines were prepared based on the strain that was considered to be the most important cause of severe HFMD in each region. Therefore, EV-A71 vaccine development has progressed the fastest; strain C4a was used in China, and the B3 and B4 strains were used in Singapore and Taiwan, respectively [96]. In China, three companies (Chinese Academy of Medical Sciences, Sinovac and Vigoo Biological Company) produced EV-A71 C4a vaccines. All have been tested in randomized clinical trials involving several thousands of infants and young children and all were found to be immunogenic, safe and capable of conferring protection in most of the vaccinated individuals [97,98,99,100,101]. Thus, China’s Food and Drug Administration had licensed all of these preparations for use in humans. Two doses 28 days apart were suggested [95]. However, the analysis of clinical trial data has led to the conclusion that protection is limited in duration and that the administration of a third dose can prolong protection for at least 2 years [95]. In a study enrolling 10,077 participants, in which three doses of the EV71 C4a vaccine were administered at 6, 12 and 18 months, an overall efficacy of 94.7% (95% CI 87.8–97.6) for 2 years was demonstrated [100]. The importance of persistent high levels of specific antibody titres is clearly suggested by the evidence that protection is considerably longer when vaccinated subjects achieve a neutralizing antibody titre higher than 1/16–1/32, the values frequently achieved with the suggested schedule. Zhu et al. reported that for children with a negative baseline of EV71 antibody titres, an antibody level of 26.6 U/mL (1:30) was estimated to provide at least 50% protection for 12 months, and an antibody level of 36.2 U/mL (1:42) may be needed to achieve a 50% protection level for the population for 24 months [102].
The immune response elicited by the vaccines based on the EV-A71 C4a strain seem to be able to confer broad cross-protection against the B and C sub-genotypes [97,98,99, 103, 104]. However, these vaccines are not adequate to fully protect against EV-A71 genotype A strains [105]. Moreover, it is not known whether these vaccines could be effective against EV-A71 sub-genotypes that circulate in India and in Africa because China’s vaccines were not tested in those geographic areas. These vaccines are not effective against the CV-A16 and CV-A6 strains. Similar conclusions can be drawn for the monovalent vaccines, including EV-A71 serotypes B3 and B4, produced in Singapore and Taiwan. Thus, in areas where CV-A16 and CV-A6 circulate alone or in association with EV-A71 and are responsible for severe cases, these vaccines are poorly effective. Monovalent vaccines against CV-A16 or CV-A6 have similar limitations. To overcome these problems, multivalent inactivated vaccines have been suggested and are in development. Whole-virus aluminium-adjuvant bivalent vaccines containing EV-A71 and CV-A16 have been tested in mice. Protection against severe infection due to both viruses, without any immunologic interference, was demonstrated [106, 107]. Moreover, anti-CV-A16 serum was found to be able to neutralize both homologous and heterologous CV-A16 strains [107]. Finally, a trivalent vaccine containing EV-A71, CV-A16 and CV-A6 strains has been tested in experimental animals and has demonstrated adequate immune response and protection [108].
Several other types of vaccines against HFMD are in development. Recombinant proteins and synthetic peptides, DNA vaccines and recombinant vector vaccines, live attenuated vaccines and virus-like particle (VLP) vaccines have been tested. Among these options, vaccines based on live attenuated virus are very attractive because they are economical to manufacture and evoke high and persistent immune responses with cellular and humoral immunity. However, to fully develop these vaccines, adequate knowledge of virulence determinants is needed to sufficiently attenuate viral strains and avoid the risk of severe adverse events [81, 94, 96]. Several attempts in this regard have been made, and it is likely than in the future strains with sufficient attenuation and stability will be available for vaccine formulation [95]. VLP vaccines are in more advanced stages of development. A CV-A16 VLP vaccine was produced from recombinant baculovirus-infected Sf9 cells. Both in vitro and in vivo studies have demonstrated the efficacy of this vaccine. Serum from immunized animals neutralized both homologous and heterologous CV-A16 strains. Moreover, mice were protected against lethal doses of the virus [109]. Similar to the monovalent vaccine, a bivalent VPL vaccine containing both EV-A71 and CV-A16 was found to be effective against experimental infections due to both viruses even if the infectious agents belonged to different sub-genotypes [108].
However, independent of the type of vaccine, further studies are needed to develop an effective universal vaccine able to confer long-term protection. The molecular epidemiology of viruses that cause HFMD could be changed by the recombination between circulating genotypes and sub-genotypes. Moreover, spontaneous mutations of the viral genome could further modify virus circulation. Theoretically, immune escape is possible because causative viruses can undergo a process of antigenic evolution and mutants can be generated, which can lead to poor protection against the sub-genotype included in the vaccine and, in particular, against different sub-genotype strains. The effect of significant modification of the molecular epidemiology of HFMD viruses should be studied because it can continuously modify vaccine efficacy. Vaccines containing several viruses can, at least in part, overcome this problem. However, the most effective combination has not been established. Several aspects of the use of currently available vaccines should be better defined to determine the best schedule of administration, the correlate of protection, the true duration of induced protection and whether a combination of several viruses causes immunologic interference.
Conclusion
In contrast to previous beliefs, in the last 20 years, it has been clarified that HFMD can be associated with severe complications, leading to severe neurological sequelae and, rarely, to death. This finding has led to an enormous number of studies that have indicated that several viruses in addition to those known to be causes of HFMD could be associated with the development of disease. Moreover, it was found that if some viruses were more common in some geographic areas, frequent modification of the molecular epidemiology of the infecting strains could lead to outbreaks caused by infectious agents significantly different from those previously circulating. Vaccines able to confer protection against the most common aetiologic agents in a given country have been developed. However, simultaneous circulation of more than one causative virus and modification of the molecular epidemiology of infectious agents make preparations based on a single agent relatively inadequate. Vaccines with multiple components are a possible solution. However, several problems concerning their development must be solved before adequate prevention of severe cases of HFMD can be achieved.
References
Robinson CR, Doane FW, Rhodes AJ (1958) Report of an outbreak of febrile illness with pharyngeal lesions and exanthem: Toronto, summer 1957; isolation of group A Coxsackie virus. Can Med Assoc J 79:615–621
Nassef C, Ziemer C, Morrell DS (2015) Hand-foot-and-mouth disease: a new look at a classic viral rash. Curr Opin Pediatr 27:486–491
Koh WM, Bogich T, Siegel K, Jin J, Chong EY, Tan CY et al (2016) The epidemiology of hand, foot and mouth disease in Asia: a systematic review and analysis. Pediatr Infect Dis J 35:e285–e300
Crabol Y, Pean P, Mey C, Duong V, Richner B, Laurent D et al (2017) A prospective, comparative study of severe neurological and uncomplicated hand, foot and mouth forms of paediatric enterovirus 71 infections. Int J Infect Dis 59:69–76
Long L, Xu L, Xiao Z, Hu S, Luo R, Wang H et al (2016) Neurological complications and risk factors of cardiopulmonary failure of EV-A71-related hand, foot and mouth disease. Sci Rep 6:23444
Shang L, Xu M, Yin Z (2013) Antiviral drug discovery for the treatment of enterovirus 71 infections. Antivir Res 97:183–194
Aswathyraj S, Arunkumar G, Alidjinou EK, Hober D (2016) Hand, foot and mouth disease (HFMD): emerging epidemiology and the need for a vaccine strategy. Med Microbiol Immunol 205:397–407
World Health Organization. Western Pacific Region. Emerging disease surveillance and response. A Guide to Clinical Management and Public Health Response for Hand, Foot and Mouth Disease (HFMD). Available at: http://www.wpro.who.int/publications/docs/GuidancefortheclinicalmanagementofHFMD.pdf?ua=1 Accessed on: 29 Nov 2017
Liu SL, Pan H, Liu P, Amer S, Chan TC, Zhan J et al (2015) Comparative epidemiology and virology of fatal and nonfatal cases of hand, foot and mouth disease in mainland China from 2008 to 2014. Rev Med Virol 25:115–128
Chang LY, King CC, Hsu KH, Ning HC, Tsao KC, Li CC et al (2002) Risk factors of enterovirus 71 infection and associated hand, foot, and mouth disease/herpangina in children during an epidemic in Taiwan. Pediatrics 109:e88
Ang LW, Phoon MC, Wu Y, Cutter J, James L, Chow VT (2011) The changing seroepidemiology of enterovirus 71 infection among children and adolescents in Singapore. BMC Infect Dis 11:270
Qiaoyun F, Xiongfei J, Lihuan L, Angao X (2013) Epidemiology and etiological characteristics of hand, foot and mouth disease in Huizhou city between 2008 and 2011. Arch Virol 158:895–899
Wang Y, Feng Z, Yang Y, Self S, Gao Y, Longini IM et al (2011) Hand, foot, and mouth disease in China: patterns of spread and transmissibility. Epidemiology 22:781–792
Zhu D, Zhao XY, Yao Y, Dai FF, He H, Li RQ et al (2013) A new factor influencing pathogen detection by molecular assay in children with both mild and severe hand, foot, and mouth disease. Diagn Microbiol Infect Dis 76:162–167
Zeng M, Li Y-F, Wang X-H, Lu GP, Shen HG, Yu H et al (2012) Epidemiology of hand, foot, and mouth disease in children in Shanghai 2007–2010. Epidemiol Infect 140:1122–1130
Ruan F, Yang T, Ma H, Jin Y, Song S, Fontaine RE et al (2011) Risk factors for hand, foot, and mouth disease and herpangina and the preventive effect of hand-washing. Pediatrics 127:e898–e904
Chen SP, Huang YC, Li WC, Chiu CH, Huang CG, Tsao KC et al (2010) Comparison of clinical features between coxsackievirus A2 and enterovirus 71 during the enterovirus outbreak in Taiwan, 2008: a children’s hospital experience. J Microbiol Immunol Infect 43:99–104
Wang YR, Sun LL, Xiao WL, Chen LY, Wang XF, Pan DM (2013) Epidemiology and clinical characteristics of hand foot, and mouth disease in a Shenzhen sentinel hospital from 2009 to 2011. BMC Infect Dis 13:539
Ma E, Chan KC, Cheng P, Cheng P, Wong C, Chuang SK (2010) The enterovirus 71 epidemic in 2008—public health implications for Hong Kong. Int J Infect Dis 14:e775–e780
Ma E, Lam T, Chan KC, Wong C, Chuang SK (2010) Changing epidemiology of hand, foot, and mouth disease in Hong Kong, 2001–2009. Jpn J Infect Dis 63:422–426
Lee TC, Guo HR, Su HJ, Yang YC, Chang HL, Chen KT (2009) Diseases caused by enterovirus 71 infection. Pediatr Infect Dis J 28:904–910
Samphutthanon R, Tripathi NK, Ninsawat S, Duboz R (2014) Spatio-temporal distribution and hotspots of hand, foot and mouth disease (HFMD) in northern Thailand. Int J Environ Res Public Health 11:312–336
Tu PV, Thao NT, Perera D, Huu TK, Tien NT, Thuong TC et al (2007) Epidemiologic and virologic investigation of hand, foot, and mouth disease, southern Vietnam, 2005. Emerg Infect Dis 13:1733–1741
Nguyen NT, Pham HV, Hoang CQ, Nguyen TM, Nguyen LT, Phan HC et al (2014) Epidemiological and clinical characteristics of children who died from hand, foot and mouth disease in Vietnam, 2011. BMC Infect Dis 14:341
Podin Y, Gias EL, Ong F, Leong YW, Yee SF, Yusof MA et al (2006) Sentinel surveillance for human enterovirus 71 in Sarawak, Malaysia: lessons from the first 7 years. BMC Public Health 6:180
Chan MCK, Wong HB (1973) Hand-foot and mouth disease. J Singapore Paediatr Soc 15:31–34
Li C (2008) The prevalence of hand, foot and mouth disease. J Pediatr Pharm 14:64–66
Sun LM, Zheng HY, Zheng HZ, Guo X, He JF, Guan DW et al (2011) An enterovirus 71 epidemic in Guangdong Province of China, 2008: epidemiological, clinical, and virogenic manifestations. Jpn J Infect Dis 64:13–18
Zhang Y, Tan XJ, Wang HY, Yan DM, Zhu SL, Wang DY et al (2009) An outbreak of hand, foot, and mouth disease associated with subgenotype C4 of human enterovirus 71 in Shandong. China J Clin Virol 44:262–267
Abedi GR, Watson JT, Pham H, Nix WA, Oberste MS, Gerber SI (2015) Enterovirus and human parechovirus surveillance—United States, 2009–2013. MMWR Morb Mortal Wkly Rep 64:940–943
Mirand A, Henquell C, Archimbaud C, Ughetto S, Antona D, Bailly JL et al (2012) Outbreak of hand, foot and mouth disease/herpangina associated with coxsackievirus A6 and A10 infections in 2010, France: a large citywide, prospective observational study. Clin Microbiol Infect 18:E110–E118
Mirand A, le Sage FV, Pereira B, Cohen R, Levy C, Archimbaud C et al (2016) Ambulatory pediatric surveillance of hand, foot and mouth disease as signal of an outbreak of coxsackievirus A6 infections, France, 2014–2015. Emerg Infect Dis 22:1884–1893
Zell R (2017) Picornaviridae-the ever-growing virus family. Arch Virol. https://doi.org/10.1007/s00705-017-3614-8
Repass GL, Palmer WC, Stancampiano FF (2014) Hand, foot, and mouth disease: identifying and managing an acute viral syndrome. Cleve Clin J Med 81:537–543
Gao F, Bian LL, Mao QY, Chen P, Yao X, Li JX et al (2016) An epidemic of coxsackievirus B3 infection in infants and children in Jiangsu Province, China: a prospective cohort study. Arch Virol 161:1945–1947
Bian L, Wang Y, Yao X, Mao Q, Xu M, Liang Z (2015) Coxsackievirus A6: a new emerging pathogen causing hand, foot and mouth disease outbreaks worldwide. Expert Rev Anti-Infect Ther 13:1061–1071
Yip CC, Lau SK, Woo PC, Yuen KY (2013) Human enterovirus 71 epidemics: what’s next? Emerg Health Threats J 6:19780
Chen B, Sumi A, Toyoda S, Hu Q, Zhou D, Mise K (2015) Time series analysis of reported cases of hand, foot, and mouth disease from 2010 to 2013 in Wuhan. China BMC Infect Dis 15:495
Centers for Disease Control and Prevention (CDC) (2012) Notes from the field: severe hand, foot, and mouth disease associated with coxsackievirus A6—Alabama, Connecticut, California, and Nevada, November 2011–February 2012. MMWR Morb Mortal Wkly Rep 61:213–214
Yang F, Yuan J, Wang X, Li J, Du J, Su H et al (2014) Severe hand, foot, and mouth disease and coxsackievirus A6-Shenzhen, China. Clin Infect Dis 59:1504–1505
Puenpa J, Mauleekoonphairoj J, Linsuwanon P, Suwannakarn K, Chieochansin T, Korkong S et al (2014) Prevalence and characterization of enterovirus infections among pediatric patients with hand foot mouth disease, herpangina and influenza like illness in Thailand, 2012. PLoS One 9:e98888
Cabrerizo M, Tarragó D, Muñoz-Almagro C, Del Amo E, Domínguez-Gil M, Eiros JM et al (2014) Molecular epidemiology of enterovirus 71, coxsackievirus A16 and A6 associated with hand, foot and mouth disease in Spain. Clin Microbiol Infect 20:150–156
Fonseca MC, Sarmiento L, Resik S, Martínez Y, Hung LH, Morier L et al (2014) Coxsackievirus A6 and enterovirus 71 causing hand, foot and mouth disease in Cuba, 2011-2013. Arch Virol 159:2451–2455
Hayman R, Shepherd M, Tarring C, Best E (2014) Outbreak of variant hand-foot-and-mouth disease caused by coxsackievirus A6 in Auckland, New Zealand. J Paediatr Child Health 50:751–755
Sinclair C, Gaunt E, Simmonds P, Broomfield D, Nwafor N, Wellington L et al (2014) Atypical hand, foot, and mouth disease associated with coxsackievirus A6 infection, Edinburgh, United Kingdom, January to February 2014. Euro Surveill 19:20745
Yang Q, Ding J, Cao J, Huang Q, Hong C, Yang B (2015) Epidemiological and etiological characteristics of hand, foot, and mouth disease in Wuhan, China from 2012 to 2013: outbreaks of coxsackieviruses A10. J Med Virol 87:954–960
Hu YQ, Xie GC, Li DD, Pang LL, Xie J, Wang P et al (2015) Prevalence of coxsackievirus A6 and enterovirus 71 in hand, foot and mouth disease in Nanjing, China in 2013. Pediatr Infect Dis J 34:951–957
Huang SW, Cheng HL, Hsieh HY, Chang CL, Tsai HP, Kuo PH et al (2014) Mutations in the non-structural protein region contribute to intra-genotypic evolution of enterovirus 71. J Biomed Sci 21:33
Chan KP, Goh KT, Chong CY, Teo ES, Lau G, Ling AE (2003) Epidemic hand, foot and mouth disease caused by human enterovirus 71, Singapore. Emerg Infect Dis 9:78–85
Lee MS, Tseng FC, Wang JR, Chi CY, Chong P, Su IJ (2012) Challenges to licensure of enterovirus 71 vaccines. PLoS Negl Trop Dis 6:e1737
Mirand A, Peigue-Lafeuille H (2017) Clinical characteristics and course of hand, foot, and mouth disease. Arch Pediatr 24:1036–1046
Schuffenecker I, Henquell C, Mirand A, Coste-Burel M, Marque-Juillet S, Desbois D et al (2014) New introductions of enterovirus 71 subgenogroup C4 strains, France, 2012. Emerg Infect Dis 20:1343–1346
Mao Q, Wang Y, Yao X, Bian L, Wu X, Xu M et al (2014) Coxsackievirus A16: epidemiology, diagnosis, and vaccine. Hum Vaccines Immunother 10:360–367
Sun T, Liu Y, Zhang Y, Zhou L (2014) Molecular phylogeny of coxsackievirus A16. J Clin Microbiol 52:3829–3830
Xu M, Su L, Cao L, Zhong H, Dong N, Dong Z et al (2015) Genotypes of the enterovirus causing hand foot and mouth disease in Shanghai, China, 2012–2013. PLoS One 10:e0138514
Gaunt E, Harvala H, Österback R, Sreenu VB, Thomson E, Waris M et al (2015) Genetic characterization of human coxsackievirus A6 variants associated with atypical hand, foot and mouth disease: a potential role of recombination in emergence and pathogenicity. J Gen Virol 96:1067–1079
Chen JF, Zhang RS, Ou XH, Chen FM, Sun BC (2014) The role of enterovirus 71 and coxsackievirus A strains in a large outbreak of hand, foot, and mouth disease in 2012 in Changsha. China Int J Infect Dis 28:17–25
Tian H, Zhang Y, Sun Q, Zhu S, Li X, Pan Z et al (2014) Prevalence of multiple enteroviruses associated with hand, foot, and mouth disease in Shijiazhuang City, Hebei province, China: outbreaks of coxsackieviruses a10 and b3. PLoS One 9:e84233
Chang LY, Tsao KC, Hsia SH, Shih SR, Huang CG, Chan WK et al (2004) Transmission and clinical features of enterovirus 71 infections in household contacts in Taiwan. JAMA 291:222–227
Lee MS, Chiang PS, Luo ST, Huang ML, Liou GY, Tsao KC (2012) Incidence rates of enterovirus 71 infections in young children during a nationwide epidemic in Taiwan, 2008–09. PLoS Negl Trop Dis 6:e1476
Yang Z, Zhang Q, Cowling BJ, Lau EHY (2017) Estimating the incubation period of hand, foot and mouth disease for children in different age groups. Sci Rep 7:16464
Blomqvist S, Klemola P, Kaijalainen S, Paananen A, Simonen ML, Vuorinen T et al (2010) Co-circulation of coxsackieviruses A6 and A10 in hand, foot and mouth disease outbreak in Finland. J Clin Virol 48:49–54
World Health Organization. Western Pacific Regional Office, WHO Emerging Disease Surveillance and Response. Hand, Foot and Mouth Disease Information Sheet. 2012; Available at: http://www.wpro.who.int/emerging_diseases/hfmd.information.sheet/en/. Accessed 30 Nov 2017
Mathes EF, Oza V, Frieden IJ, Cordoro KM, Yagi S, Howard R et al (2013) “Eczema coxsackium” and unusual cutaneous findings in an enterovirus outbreak. Pediatrics 132:e149–e157
Flett K, Youngster I, Huang J, McAdam A, Sandora TJ, Rennick M et al (2012) Hand, foot, and mouth disease caused by coxsackievirus A6. Emerg Infect Dis 18:1702–1704
Hubiche T, Schuffenecker I, Boralevi F, Léauté-Labrèze C, Bornebusch L, Chiaverini C et al (2014) Dermatological spectrum of hand, foot and mouth disease from classical to generalized exanthema. Pediatr Infect Dis J 33:e92–e98
Bettoli V, Zauli S, Toni G, Virgili A (2013) Onychomadesis following hand, foot, and mouth disease: a case report from Italy and review of the literature. Int J Dermatol 52:728–730
Davia JL, Bel PH, Ninet VZ et al (2011) Onychomadesis outbreak in Valencia, Spain associated with hand, foot, and mouth disease caused by enteroviruses. Pediatr Dermatol 28:1–5
Clementz GC, Mancini AJ (2000) Nail matrix arrest following hand-foot-mouth disease: a report of five children. Pediatr Dermatol 17:7–11
Osterback R, Vuorinen T, Linna M, Susi P, Hyypiä T, Waris M (2009) Coxsackievirus A6 and hand, foot, and mouth disease, Finland. Emerg Infect Dis 15:1485–1488
Solomon T, Lewthwaite P, Perera D, Cardosa MJ, McMinn P, Ooi MH (2010) Virology, epidemiology, pathogenesis, and control of enterovirus 71. Lancet Infect Dis 10:778–790
Huang MC, Wang SM, Hsu YW, Lin HC, Chi CY, Liu CC (2006) Long-term cognitive and motor deficits after enterovirus 71 brainstem encephalitis in children. Pediatrics 118:e1785–e1788
Chang LY, Huang LM, Gau SS, Wu YY, Hsia SH, Fan TY et al (2007) Neurodevelopment and cognition in children after enterovirus 71 infection. N Engl J Med 356:1226–1234
Zhang Q, MacDonald NE, Smeith JC, Cai K, Yu H, Li H et al (2014) Severe enterovirus type 71 nervous system infections in children in the Shanghai region of China: clinical manifestations and implications for prevention and care. Pediatr Infect Dis J 33:482–487
Huang Y, Zhou Y, Lu H, Yang H, Feng Q, Dai Y et al (2015) Characterization of severe hand, foot, and mouth disease in Shenzhen, China, 2009–2013. J Med Virol 87:1471–1479
Li JL, Yuan J, Yang F, Wu ZQ, Hu YF, Xue Y (2014) Epidemic characteristics of hand, foot, and mouth disease in southern China, 2013: coxsackievirus A6 has emerged as the predominant causative agent. J Inf Secur 69:299–303
Hongyan G, Chengjie M, Qiaozhi Y, Wenhao H, Juan L, Lin P (2014) Hand, foot and mouth disease caused by coxsackievirus A6, Beijing, 2013. Pediatr Infect Dis J 33:1302–1303
Lu QB, Zhang XA, Wo Y, Xu HM, Li XJ, Wang XJ (2012) Circulation of coxsackievirus A10 and A6 in hand-foot-mouth disease in China, 2009–2011. PLoS One 7:e52073
Ooi MH, Wong SC, Lewthwaite P, Cardosa MJ, Solomon T (2010) Clinical features, diagnosis, and management of enterovirus 71. Lancet Neurol 9:1097–1105
Casas-Alba D, de Sevilla MF, Valero-Rello A, Fortuny C, García-García JJ, Ortez C et al (2017) Outbreak of brainstem encephalitis associated with enterovirus-A71 in Catalonia, Spain (2016): a clinical observational study in a children’s reference centre in Catalonia. Clin Microbiol Infect 23:874–881
Klein M (2016) Enterovirus EV-A71 vaccine licensure: what’s next? Int J Vaccines Vaccin 3:00054
Xing W, Liao Q, Viboud C, Zhang J, Sun J, Wu JT et al (2014) Hand, foot, and mouth disease in China, 2008–12: an epidemiological study. Lancet Infect Dis 14:308–318
Li JA, Chen ZB, Lv TG, Han ZL (2014) Genetic polymorphism of CCL2-2518, CXCL10-201, IL8+781 and susceptibility to severity of enterovirus-71 infection in a Chinese population. Inflamm Res 63:549–556
Yang J, Zhao N, Su NL, Sun JL, Lv TG, Chen ZB (2012) Association of interleukin 10 and interferon gamma gene polymorphisms with enterovirus 71 encephalitis in patients with hand, foot, and mouth disease. Scand J Infect Dis 44:465–469
Ong KC, Wong KT (2015) Understanding enterovirus 71 neuropathogenesis and its impact on other neurotropic enteroviruses. Brain Pathol 25:614–624
Wang SM, Lei HY, Liu CC (2012) Cytokine immunopathogenesis of enterovirus 71 brain stem encephalitis. Clin Dev Immunol 2012:876241
Shang W, Qian S, Fang L, Han Y, Zheng C (2017) Association study of inflammatory cytokine and chemokine expression in hand foot and mouth disease. Oncotarget 8:79425–79432
He Y, Yang J, Zeng G, Shen T, Fontaine RE, Zhang L et al (2014) Risk factors for critical disease and death from hand, foot and mouth disease. Pediatr Infect Dis J 33:966–970
Cao RY, Dong DY, Liu RJ, Han JF, Wang GC, Zhao H et al (2013) Human IgG subclasses against enterovirus type 71: neutralization versus antibody dependent enhancement of infection. PLoS One 8:e64024
Jia Q, Ng Q, Chin W, Meng T, Chow VTK, Wang CI et al (2017) Effective in vivo therapeutic IgG antibody against VP3 of enterovirus 71 with receptor-competing activity. Sci Rep 7:46402
Ren P, Zheng Y, Wang W, Hong L, Delpeyroux F, Arenzana-Seisdedos F et al (2017) Suramin interacts with the positively charged region surrounding the 5-fold axis of the EV-A71 capsid and inhibits multiple enterovirus a. Sci Rep 7:42902
Zhang X, Song Z, Qin B, Zhang X, Chen L, Hu Y et al (2013) Rupintrivir is a promising candidate for treating severe cases of enterovirus-71 infection: evaluation of antiviral efficacy in a murine infection model. Antivir Res 97:264–269
Tan CW, Lai JK, Sam IC, Chan YF (2014) Recent developments in antiviral agents against enterovirus 71 infection. J Biomed Sci 21:14
Chong P, Liu CC, Chow YH, Chou AH, Klein M (2015) Review of enterovirus 71 vaccines. Clin Infect Dis 60:797–803
Yee PTI, Laa PC (2017) Impact of genetic changes, pathogenicity and antigenicity on enterovirus-A71 vaccine development. Virology 506:121–129
Mao Q, Wang Y, Bian L, Xu M, Liang Z (2016) EV-A71 vaccine licensure: a first step for multivalent enterovirus vaccine to control HFMD and other severe diseases. Emerg Microbes Infect 5:e75
Zhu FC, Meng FY, Li JX, Li XL, Mao QY, Tao H et al (2013) Efficacy, safety, and immunology of an inactivated alum-adjuvant enterovirus 71 vaccine in children in China: a multicentre, randomised, double-blind, placebo-controlled, phase 3 trial. Lancet 381:2024–2032
Li R, Liu L, Mo Z, Wang X, Xia J, Liang Z et al (2014) An inactivated enterovirus 71 vaccine in healthy children. N Engl J Med 370:829–837
Zhu F, Xu W, Xia J, Liang Z, Liu Y, Zhang X et al (2014) Efficacy, safety, and immunogenicity of an enterovirus 71 vaccine in China. N Engl J Med 370:818–828
Li JX, Song YF, Wang L, Zhang XF, Hu YS, Hu YM et al (2016) Two-year efficacy and immunogenicity of Sinovac enterovirus 71 vaccine against hand, foot and mouth disease in children. Expert Rev Vaccines 15:129–137
Liu L, Mo Z, Liang Z, Zhang Y, Li R, Ong KC et al (2015) Immunity and clinical efficacy of an inactivated enterovirus 71 vaccine in healthy Chinese children: a report of further observations. BMC Med 13:226
Zhu W, Jin P, Li JX, Zhu FC, Liu P (2017) Correlates of protection for inactivated enterovirus 71 vaccine: the analysis of immunological surrogate endpoints. Expert Rev Vaccines. 16:945–949
Li JX, Mao QY, Liang ZL, Ji H, Zhu FC (2014) Development of enterovirus 71 vaccines: from the lab bench to phase 3 clinical trials. Expert Rev Vaccines 13:609–618
Mao Q, Cheng T, Zhu F et al (2013) The cross-neutralizing activity of enterovirus 71 subgenotype C4 vaccines in healthy Chinese infants and children. PLoS One 8:e79599
Zhang H, An D, Liu W, Mao Q, Jin J, Xu L et al (2014) Analysis of cross-reactive neutralizing antibodies in human HFMD serum with an EV71 pseudovirus-based assay. PLoS One 9:e100545
Sun S, Jiang L, Liang Z, Mao Q, Su W, Zhang H et al (2014) Evaluation of monovalent and bivalent vaccines against lethal enterovirus 71 and coxsackievirus A16 infection in newborn mice. Hum Vaccin Immunother 10:2885–2895
Cai Y, Ku Z, Liu Q, Leng Q, Huang Z (2014) A combination vaccine comprising of inactivated enterovirus 71 and coxsackievirus A16 elicits balanced protective immunity against both viruses. Vaccine 32:2406–2412
Caine EA, Fuchs J, Das SC, Partidos CD, Osorio JE (2015) Efficacy of a trivalent hand, foot, and mouth disease vaccine against enterovirus 71 and coxsackieviruses A16 and A6 in mice. Viruses 7:5919–5932
Zhang C, Liu Q, Ku Z, Hu Y, Ye X, Zhang Y et al (2016) Coxsackievirus A16-like particles produced in Pichia pastoris elicit high-titer neutralizing antibodies and confer protection against lethal viral challenge in mice. Antivir Res 129:47–51
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
Conflict of interest
The authors declare that they have no potential conflict of interest.
Ethical approval
Ethical approval was not required for a review article.
Informed consent
Informed consent was not required for a review article.
Rights and permissions
About this article
Cite this article
Esposito, S., Principi, N. Hand, foot and mouth disease: current knowledge on clinical manifestations, epidemiology, aetiology and prevention. Eur J Clin Microbiol Infect Dis 37, 391–398 (2018). https://doi.org/10.1007/s10096-018-3206-x
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s10096-018-3206-x