Abstract
The purpose of this study was to investigate the clinical characteristics of hypervirulent K. pneumoniae (hvKP) induced ventilator-associated pneumonia (VAP) and the microbiological characteristics and epidemiology of the hvKP strains. A retrospective study of 49 mechanically ventilated patients with K. pneumoniae induced VAP was conducted at a university hospital in China from January 2014 to December 2014. Clinical characteristics and K. pneumoniae antimicrobial susceptibility and biofilm formation were analyzed. Genes of capsular serotypes K1, K2, K5, K20, K54 and K57 and virulence factors plasmid rmpA(p-rmpA), iroB, iucA, mrkD, entB, iutA, ybtS, kfu and allS were also evaluated. Multilocus sequence typing (MLST) and random amplified polymorphic DNA (RAPD) analyses were used to study the clonal relationship of the K. pneumoniae strains. Strains possessed p-rmpA and iroB and iucA were defined as hvKP. Of 49 patients, 14 patients (28.6 %) were infected by hvKP. Antimicrobial resistant rate was significantly higher in cKP than that in hvKP. One ST29 K54 extended-spectrum-beta-lactamase (ESBL) producing hvKP strain was detected. The prevalence of K1 and K2 in hvKP was 42.9 % and 21.4 %, respectively. The incidences of K1, K2, K20, p-rmpA, iroB, iucA, iutA, Kfu and alls were significantly higher in hvKP than those in cKP. ST23 was dominant among hvKP strains, and all the ST23 strains had identical RAPD pattern. hvKP has become a common pathogen of VAP in mechanically ventilated patients in China. Clinicians should increase awareness of hvKP induced VAP and enhance epidemiologic surveillance.
Similar content being viewed by others
Introduction
Klebsiella pneumoniae is one of the most common gram-negative bacteria causing hospital-acquired pneumonia (HAP) [1]. K. pneumoniae has been divided into two distinct groups. One is termed “classic” K. pneumoniae (cKP) which was considered the pathogen causing most K. pneumoniae induced hospital-acquired infection [2]. cKP has been notorious for acquiring antimicrobial resistance. The other is a new variant of K. pneumoniae and termed hypervirulent K. pneumoniae (hvKP). hvKP has appeared in the past three decades as the cause of community-acquired liver abscess in Taiwan, South Korea, and other Asian countries [3–5]. Recently, reports on hvKP-induced infection from countries outside Asia have increased [6–8]. hvKP is characterized by causing severe invasive community-acquired infection with metastatic spread in immunocompetent individuals [8]. A specific marker with high sensitivity for detecting hvKP strains is now lacking. A hypermucoviscous phenotype which can be determined by “string test” has been used to differentiate hvKP from cKP in previous studies [9–11]; however, it is unclear whether all hvKP strains are hypermucoviscous [8]. Possessing a large virulent plasmid with virulence factors encoded genes, including regulator of the mucoid phenotype gene (rmpA) and iron-acquisition systems aerobactin biosynthetic gene (iucABCD) and slmochelin biosynthetic gene (iroBCD), has been reported being associated with K. pneumoniae virulence [12–15]. In contrast to cKP, the majority of hvKP strains are susceptible to most antimicrobial with the exception of ampicillin. However, extended-spectrum-beta-lactamase (ESBL)-producing and carbapenem-resistant hvKP strains have already occurred [10–14]. The occurrence of antimicrobial-resistant hvKP isolates has generated the concern that hvKP combining hypervirulence with antimicrobial resistance will become the next “superbug” [16].
Research on hvKP has identified several virulence factors, including capsular serotypes K1 and K2 [17, 18], mucoviscosity associated gene A (magA) [9], regulator of mucoid phenotype A (rmpA) [19], and iron acquisition factors [20]. However, most studies have focused on community-acquired infection caused by hvKP. Study on hvKP induced hospital-acquired infection has been limited. HAP is the second most common hospital-acquired infection after urinary tract infection and is the leading cause of mortality due to hospital-acquired infection [21]. Ventilator-associated pneumonia(VAP) is an important form of HAP [22], and the mortality rate of VAP was reported ranging from 30 to 70 % [23]. Yet, little is known about the clinical and microbiological characteristics of VAP caused by hvKP. The purpose of this study was to investigate the clinical characteristics of hvKP induced VAP in mechanically ventilated patients and the microbiological characteristics and epidemiology of the hvKP strains, using the cKP induced VAP as reference.
Material and methods
Patient information
A retrospective study was conducted at Xiangya Hospital (Hunan, China) from January 2014 to December 2014. Xiangya hospital is a 3500-bed tertiary university hospital with an annual admission of more than 100,000 inpatients. K. pneumoniae strains were isolated from lower respiratory tract secretion of hospitalized patients and stored at –80 °C before use. One K. pneumoniae strain per patient was collected and the initial strain isolated was used for collection. Medical records of patients from whom the collected strains were isolated were reviewed. Cases of VAP that met the following criteria were included: (1) receiving mechanical ventilation and presence of VAP. VAP was defined as pneumonia occurring 48 h or more after endotracheal intubation [16]. Patients had a new or progressive radiographic infiltrate, along with at least two of the following clinical findings: fever greater than 38 °C, a leukocyte count of more than 10,000/μL or less than 4000/μL, and purulent sputum [22]. (2) They must have K. pneumoniae isolated from lower respiratory tract. Patients without these conditions were excluded.
The following data were collected: sex, age, underlying diseases (diabetes, hypertension, chronic pulmonary disease, neurologic disease, chronic liver disease), Acute Physiology and Chronic Health Evaluation II (APACHE II) score [24], empirical antibiotics received and surgery performed within 7 days prior to positive culture of K. pneumoniae, days of hospitalization and days on mechanical ventilation prior to K. pneumoniae cultured, route of ventilation (oroendotracheal, tracheostomy), concurrent K. pneumoniae bacteremia, metastatic K. pneumoniae infection, days of hospital stay and in-hospital mortality. Neurologic diseases encompassed stroke and head injury. Chronic lung diseases included chronic obstructive pulmonary diseases, bronchiectasis, and old pulmonary tuberculosis. Chest radiography reports and laboratory data (white blood cell [WBC] count, albumin, C-reactive protein [CRP], procalcitonin [PCT], total bilirubin) were also obtained. Laboratory data were taken on the day of the first K. pneumoniae strain isolated from the lower respiratory tract. This study was approved by the Xiangya Hospital Ethics Committee.
Microbiological characteristics
String test was performed by using a standard bacteriologic loop to stretch a mucoviscous string from the colony. Strains with a mucoviscous string >5 mm were defined as positive string test [9]. All K. pneumoniae strains underwent antimicrobial susceptibility testing to ampicillin, cefazolin, cefotan, ceftriaxone, cefepime, ceftazidime, ampicillin-sulbactam, piperacillin-tazobactam, aztreonam, amikacin, tobramycin, gentamicin, ertapenem, imipenem, ciprofloxacin, levofloxacin and trimethoprim-sulfamethoxazole by bioMerieux VITEK-2 (bioMerieux). The minimum inhibitory concentrations (MICs) of antimicrobial agents were interpreted according to the performance standards for antimicrobial susceptibility testing issued by the Clinical and Laboratory Standards Institute (CLSI) in 2013 [25]. ESBL was also determined by the bioMerieux VITEK-2 system. In addition, carba NP test was performed to carbapenem resistant strains [26]; moreover, polymerase chain reaction (PCR) was used to detect KPC, NDM, IMP, VIM and OXA48 genes in carba NP positive strains as previously reported [27].
Biofilm assay
A crystal violet assay was performed to measure the ability of forming biofilm among K. pneumoniae strains, which was done in 96-well microtitre plates as previously described with a minor modification [28]. Briefly, bacteria were incubated in Luria-Bertani broth (LB) with 180 rpm in 35 °C for 24 h and then suspended in LB to make a concentration of 1.5 × 108 CFU/mL, then 200ul was added to 96-well plates for incubating at 35 °C for 48 h. Unbound bacteria were removed by washing with sterile distilled water, and the remaining bacteria were stained with 200 μL 1 % (w/v) crystal violet dye for 20 min. Then unbound dye was washed away. The bound crystal violet dye was solubilized by using 200 μL 95 % ethanol. Biofilm was quantified by measuring the optical density (OD) of the supernatant at 570 nm. The biofilm assay for each strain was performed in triplicate and the mean absorbance value was determined.
Polymerase chain reaction-mediated detection of capsular serotype and virulence genes
Crude genomic DNA was extracted from K. pneumoniae strains and genes for K1, K2, K5, K20, K54, and K57 capsular serotypes were amplified by a multiplex PCR as previously described [29]. Virulent plasmid-derived genes of p-rmpA, iucA, and iroB were identified using the primes as previously reported [20, 30], which was also used to determine hvKP. Strains positive for p-rmpA and iroB and iucA were designated as hvKP. Other virulent factor genes of mrkD, entB, iutA, ybtS, kfu and allS were amplified as previously reported [31]. The primers used are listed in Table 1.
Multilocus sequence typing (MLST)
MLST was performed for all K. pneumoniae strains by amplifying and sequencing seven housekeeping genes for K. pneumoniae (gapA, infB, mdh, pgi, phoE, rpoB, and tonB) according to the protocol provided on the MLST website (www.pasteur.fr/mlst) [32]. Alleles and sequence types (STs) were determined according to the MLST database (www.pasteur.fr/mlst/Kpneumoniae.html).
Random amplified polymorphic DNA (RAPD)
All K. pneumoniae strains were analyzed by RAPD-PCR using primers RAPD4 (AAGACGCCGT) as previously described [33]. PCR products were electrophoresed on 2.0 % (w⁄ v) agarose gels, and the banding pattern analysis was performed by NTSYS-pc software (version 2.0). The similarity of banding pattern was calculated using the Dice coefficient. Cluster analysis was performed using the unweighted pair-group method with arithmetic averages (UPGMA). Strains were considered as the same RAPD type if they possessed ≥80 % similarity.
Statistical analyses
Contingency variables were analyzed by 2-tailed Chi-square test or Fisher’s exact test. Medians with 25th–75th percentiles were used for continuous variables, unless otherwise indicated. Continuous variables were analyzed by Student’s t test or the Mann–Whitney U test. A P value of <0.05 was considered to be statistically significant, and all probabilities were two-tailed. All statistical analyses were performed by SPSS, version 20.0 for Windows.
Results
Clinical characteristics
From January 2014 to December 2014, a total of 49 mechanically ventilated patients were identified with K. pneumoniae induced VAP. The patients had mean ± standard deviation age of 56.0 ± 19.0 years. Thirty-nine (79.6 %) were male and 10 (20.4 %) were female. As determined by positive p-rmpA and iroB and iucA, isolates of hvKP were obtained from 14 (28.6 %) patients and cKP strains were from 35 (71.4 %) patients. The baseline characteristics of patients with K. pneumoniae induced VAP is presented in Table 2. Most patients (75.5 %) had neurologic disorder. There was no statistically significant difference in underlying disease between hvKP and cKP groups. The laboratory findings and clinical characteristics of the patients with VAP due to hvKP and cKP are compared in Table 3. Patients infected with hvKP induced VAP had a shorter duration of hospitalization prior to K. pneumonia cultured, the median length of stay was 11 vs. 18 days among cKP infected patients (P = 0.054), whereas the full hospital stay did not differ between them. There was no statistically significant difference in severity of disease as expressed by APACHE II score between patients with hvKP and cKP induced VAP. Metastatic K. pneumoniae infection to other sites of the body did not occur in either the hvKP or cKP infected group. No in-hospital death was found in any of the 49 cases.
Antimicrobial resistance analysis
All 49 K. pneumoniae strains showed uniform resistance to ampicillin. cKP showed significantly higher antimicrobial resistant rate for almost all antimicrobials than hvKP (Table 4). All but one hvKP strain were susceptible to all the tested anitimicrobials except ampicillin. This hvKP strain was an ESBL-producing strain which was resistant to ampicillin, ampicillin-sulbactam, cefazolin, ceftriaxone and aztreonam. The percentage of ESBL-producing strains among cKP was significantly higher than that among hvKP (62.9 % vs. 7.1 %, P < 0.001). Eleven cKP strains resistant to Imipenem and Ertapenem were carbaNP positive. Among them, ten cKP were KPC positive, and 1 cKP possessed NDM.
Microbiological characteristics
All but one hvKP strain (92.5 %) showed hypermucosicovity phenotype as evidenced by positive string test, whereas, only 1 cKP strain (2.9 %) possessed hypermucosicovity phenotype. The biofilm-forming abilities had no significant difference between hvKP and cKP strains (OD570 values (mean ± SD) 0.7367 ± 0.3770 vs. 0.8086 ± 0.375, P = 0.411). Capsular genotypes K1 and K2 comprised 14.3 % (7/49) and 6.1 % (3/49) of all K. pneumoniae strains. All K. pneumoniae strains had entB and mrkD. The majority of K. pneumoniae strains (83.7 %) possessed ybtS. The prevalence of K1 and K2 in hvKP strains were 42.9 % (6/14) and 21.4 % (3/14), respectively. All K1 strains had allS and kfu genes while all K2 strains did not. The incidences of K1, K2, K20, p-rmpA, iroB, iucA,iutA, Kfu and alls genes were significantly higher in hvKP than those in cKP (P = 0.002, P = 0.020, P = 0.020, P < 0.001, P < 0.001, P < 0.001, P < 0.001, P < 0.001 and P = 0.002, respectively) (Table 5).
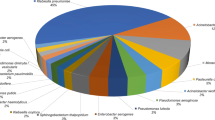
MLST and RAPD analyses
MLST analysis identified 25 sequence types (STs) among the 49 K. pneumoniae strains (Fig. 1). The most prevalent ST in hvKP strains was ST23 (42.8 %), followed by ST65 (14.3 %). All K1 K. pneumoniae belonged to ST23. Two K2 K. pneumoniae belonged to ST65 and the other K2 belonged to ST86. Two K20 K. pneumoniae belonged to ST268 and the other K20 belonged to ST420. The K54 K. pneumoniae belonged to ST29. The most prevalent ST in cKP was ST11 (28.5 %) and they were all KPC positive K. pneumoniae, followed by ST35, ST45 and ST133 (8.6 % each). RAPD analysis showed that 49 K. pneumoniae strains revealed 21 different types. The banding patterns were designated RAPD types 1 to 21 (Fig. 1). Fourteen hvKP strains had five different RAPD patterns. Seven ST23 K. pneumoniae strains showed the identical RAPD banding pattern. Among them, three were isolated from the neurosugery unit in January, February and April 2014, respectively, the other four ST23 were from different clinical wards. Thirty-five cKP strains showed 16 different RAPD types. Ten ST11 K. pneumoniae strains showed the same RAPD type. Dendrogram based on RAPD of 49 K. pneumoniae strains is showed in Fig. 1.
Discussion
This retrospective study was conducted in 49 mechanically ventilated patients with VAP caused by K. pneumoniae from January 2014 to December 2014 in Xiangya Hospital. It was the first systematic study focusing on the clinical characteristics of VAP due to hvKP and its microbiological characteristics in mechanically ventilated patients. We found hvKP accounted for nearly one-third of K. pneumoniae induced VAP cases among mechanically ventilated patients. There was no statistically significant difference in severity of disease between cKP and hvKP groups. The prevalence of genotypes K1, K2, p-rmpA, iroB, iucA, iutA, Kfu and alls in hvKP strains were statistically significantly higher than those in cKP strains. The most prevalent ST in hvKP strains was ST23 with identical RAPD pattern. One ST29 with K54 serotype ESBL-producing K. pneumoniae was found.
In this study, hvKP accounted for 28.6 % (14/49) K. pneumoniae induced VAP in mechanically ventilated patients. This is the highest rate reported in hvKP induced hospital-acquired infection. Liu et al. reported 4.5 % hvKP infection in hospital-acquired K. pneumonia bacteremia in China [34]. In two previous studies in Taiwan, the prevalence of hvKP among hospital-acquired K. pneumoniae bacteremia were reported 14.8 % and 15.2 %, respectively [19, 35]. Li et al. reported 33.0 % hvKP of K. pneumoniae isolated from various specimens; however, most hvKP strains were from community-acquired infection [10]. It has been known that the prevalence of hvKP in invasive Klebsiellae liver abscess was high, ranging from 53 to 98 % [9, 14, 36, 37], and Klebsiellae liver abscess were mostly community-acquired infection.
hvKP is characterized by causing severe community-acquired liver abscess and other community-acquired infections in young healthy people, with the ability to cause metastatic spread [8]. However, in this study, the hvKP infected VAP patients had a mean age of 51 years, and there was no metastatic infection which occurred in hvKP infected patients. The reason for no metastatic spread could be due to prompt effective antibiotic treatment. Compared with patients infected by cKP caused VAP, hvKP infected patients had shorter hospitalization prior to isolated K. pneumoiae (median 11 vs 18 days; P = 0.054) even though the difference was not statistically significant. Based on this, clinicians should be alert to hvKP induced VAP in the early stage of hospitalization for mechanically ventilated patients. The reason for this difference could be that hvKP appears to colonize in the community and patients with VAP due to hvKP were colonized on admission, whereas cKP strains were more likely to be acquired during hospital stay. A previous study showed that 4 % and 2 % of Chinese adults who live in Taiwan, Hong Kong and China or other Asian countries were colonized with a K1 or K2 serotype of K. pneumoiae [38].
In accordance with previous studies [10, 11], we found hvKP were less resistant to most antimicrobials than cKP. ESBL-producing hvKP was found in 7.1 % (1/14) of cases of hvKP. The ESBL-producing hvKP was resistant to ampicillin, cefazolin, ceftriaxone, ampicillin sulbactam and aztreonam. This strain was isolated from a 60-year-old female with type 2 diabetes 3 days after she was hospitalized for stroke. This patient had no history of antibiotic use before being infected by this hvKP strain. ESBL-producing hvKP strains have been reported, with the trend of increasing occurrence [10, 11, 39]. Moreover, two hvKP strains were found resistant to carbapenem and polymyxin B while harboring some virulence genes in Brazil [40]. Recently, hypervirulent carbapenem-resistant K. pneumoniae has emerged in China [34]. Based on whole-genome sequencing, genomic analysis has detected K. pneumoniae strains combining virulence and resistance features [41]. Siu et al. successfully transferred KPC-producing plasmid into a hvKP strain which was originally only resistant to ampicillin and streptomycin, then it became resistant to all beta-lactams after conjugating KPC without losing its virulence [42]. Taken together, these data strongly support the convergence of virulence, and antimicrobial resistance genes could lead to untreatable K. pneumoniae infections [16]. This has generated great interest of developing antivirulence agents to target the virulence factors of hvKP strains instead of using antimicrobial to kill them [14, 20].
In this study, the abilities of biofilm-forming had no significant difference between cKP and hvKP groups. However, Wu et al. reported the biofilm-forming abilities of the pyogenic liver abscess-associated K. pneumoniae were significantly higher than those of the non-tissue invasive K. pneumoniae [43]. The reason for this discrepancy may be due to the fact that those K. pneumoniae strains were isolated from blood, but the K. pneumoniae strains in our study were isolated from respiratory tracts of mechanically ventilated patients. The presence of intubation tube among mechanically ventilated patients favored biofilm formation by providing an insert surface for the attachment of bacteria. MrkD involves type 3 fimbrial adhesin and mediates binding to the extracellular matrix [44]. In this study, all K. pneumoniae strains (100 %) possessed mrkD gene which could also explain the high abilities of biofilm-forming among them.
Capsular serotypes are important virulence factors for K. pneumoniae, especially K1 and K2 serotypes [17, 18]. In this study, the prevalence of K1 and K2 among hvKP was 42.9 and 21.4 %, respectively. A previous study reported 53.8 % hvKP strains isolated from liver abscess were K1 [37], while another study showed 98 % K. pneumoniae from invasive liver abscess possessed K1 [9]. The prevalence of K1 in hvKP from bacteremia has ranged from 23 to 42 % [11, 18, 31]. K2 distribution among hvKP has been reported as 10–46 % [10, 11, 37]. However, only 3.1 % of K. pneumoniae from hospital-acquired bacteremia was reported possessing K1 [11]. In addition to K1 and K2, we have detected three K20 strains, and one K54 strain which was an ESBL-producing ST29 hvKP. To our knowledge, this is the first report of ESBL-producing K. pneumoniae ST29 with K54 serotype. Chuang et al. reported a case of mycotic aneurysm caused by ST29 K54 hvKP which was susceptible to most antimicrobials except ampicillin, and stated it was difficult to treat [45]. The combination of antimicrobial resistant with hvKP might be even worse.
rmpA regulates the synthesis of extracellular polysaccharide capsule, which is responsible for the clinical manifestation of hypermucoviscous phenotype [19]. Three genes have been reported to encode for this factor: two large-plasmid-carried genes, p-rmpA and p-rmpA2, and one chromosomal gene c-rmpA; and it showed 78/79 rmpA/A2-positive K. pneumoniae strains possessed p-rmpA gene, which occurred more commonly than p-rmpA2 (62/79) and c-rmpA (10/79) [46]. In this study, we found one hvKP strain which possessed p-rmpA did not show hypermucoviscous phenotype. This indicated that there may be other regulatory mechanisms for hypermucoviscous phenotype expression [19].
Iron acquisition factors, siderophore enterobactin, aerobactin, salmochelin and yersiniabactin and Kfu, which mediate uptake of ferric iron have been reported as virulence factors in K. pneumoniae infection [20, 30, 47]. In this study, all the K. pneumoniae strains (100 %) had entB. This agreed with a previous study [31]. The majority of K. pneumoniae strains (83.6 %) possessed ybtS and the prevalence had no significant difference between hvKP and cKP strains (71.6 vs. 88.6 %; P = 0.202). The high prevalence of ybtS in the respiratory tract confirmed the point that yersiniabactin is a virulence factor for K. pneumoniae during pulmonary infection [47]. The iutA gene is responsible for encoding a receptor for aerobactin [30]. In this study, strains possessing iutA gene were more prevalent among hvKP than that among cKP (92.9 vs. 2.9 %; P < 0.001) and most p-rmpA positive K. pneumoniae strains (86.6 %) had iutA. This high coexistence of iutA and rmpA agreed with a previous study that rmpA-borne plasmid pLVPK with other rmpA-related genetic loci including iutA was essential to K. pneumonia virulence, not rmpA gene alone [30]. In accordance with previous studies of K. pneumoniae isolated from blood and liver abscess [14, 19], we found all K1 strains had allS and kfu genes while all K2 strains did not; whereas, Lin et al. reported 11.5 % kfu gene was found in K2 strains [18].
In previous studies, ST23 K. pneumoniae was the most common ST in liver abscesses [36, 48] and it has been reported clonally related in Taiwan by Lau et al. [49], while Cheng et al. reported K. pneumoniae liver abscess in Taiwan is not caused by a clonal spread strain [50]. In this study, ST23 was dominant among hvKP strains, and all ST23 strains had the identical RAPD pattern, suggesting they were epidemiologically related, as three of them were isolated from the neurosurgery unit.
In conclusion, contrary to the traditional view that hvKp is an important pathogen mainly causing community-acquired infection, this study demonstrates hvKP has become a common pathogen of VAP in mechanically ventilated patients in China. Our finding of a ST29 with K54 serotype ESBL-producing hvKp strain highlights the need for clinicians to increase awareness of hvKP induced VAP and enhance the epidemiologic surveillance of this pathogen.
References
Jones RN (2010) Microbial etiologies of hospital-acquired bacterial pneumonia and ventilator-associated bacterial pneumonia. Clin Infect Dis Off Publ Infect Dis Soc Am 51(Suppl 1):S81–S87
Kuehn BM (2013) “Nightmare” bacteria on the rise in US hospitals, long-term care facilities. JAMA 309(15):1573–1574
Liu YC, Cheng DL, Lin CL (1986) Klebsiella pneumoniae liver abscess associated with septic endophthalmitis. Arch Intern Med 146(10):1913–1916
Chung DR, Lee SS, Lee HR, Kim HB, Choi HJ, Eom JS, Kim JS, Choi YH, Lee JS, Chung MH, Kim YS, Lee H, Lee MS, Park CK, Korean Study Group for Liver A (2007) Emerging invasive liver abscess caused by K1 serotype Klebsiella pneumoniae in Korea. J Infect 54(6):578–583
Shen DX, Wang J, Li DD (2013) Klebsiella pneumoniae liver abscesses. Lancet Infect Dis 13(5):390–391
Nadasy KA, Domiati-Saad R, Tribble MA (2007) Invasive Klebsiella pneumoniae syndrome in North America. Clin Infect Dis Off Publ Infect Dis Soc Am 45(3):e25–e28
Yu VL, Hansen DS, Ko WC, Sagnimeni A, Klugman KP, von Gottberg A, Goossens H, Wagener MM, Benedi VJ, International Klebseilla Study G (2007) Virulence characteristics of Klebsiella and clinical manifestations of K. pneumoniae bloodstream infections. Emerg Infect Dis 13(7):986–993
Shon AS, Bajwa RP, Russo TA (2013) Hypervirulent (hypermucoviscous) Klebsiella pneumoniae: a new and dangerous breed. Virulence 4(2):107–118
Fang CT, Chuang YP, Shun CT, Chang SC, Wang JT (2004) A novel virulence gene in Klebsiella pneumoniae strains causing primary liver abscess and septic metastatic complications. J Exp Med 199(5):697–705
Li W, Sun G, Yu Y, Li N, Chen M, Jin R, Jiao Y, Wu H (2014) Increasing occurrence of antimicrobial-resistant hypervirulent (hypermucoviscous) Klebsiella pneumoniae isolates in China. Clin Infect Dis Off Publ Infect Dis Soc Am 58(2):225–232
Liu YM, Li BB, Zhang YY, Zhang W, Shen H, Li H, Cao B (2014) Clinical and molecular characteristics of emerging hypervirulent Klebsiella pneumoniae bloodstream infections in mainland China. Antimicrob Agents Chemother 58(9):5379–5385
Nassif X, Sansonetti PJ (1986) Correlation of the virulence of Klebsiella pneumoniae K1 and K2 with the presence of a plasmid encoding aerobactin. Infect Immun 54(3):603–608
Chen YT, Chang HY, Lai YC, Pan CC, Tsai SF, Peng HL (2004) Sequencing and analysis of the large virulence plasmid pLVPK of Klebsiella pneumoniae CG43. Gene 337:189–198
Yu WL, Ko WC, Cheng KC, Lee CC, Lai CC, Chuang YC (2008) Comparison of prevalence of virulence factors for Klebsiella pneumoniae liver abscesses between isolates with capsular K1/K2 and non-K1/K2 serotypes. Diagn Microbiol Infect Dis 62(1):1–6
Struve C, Roe CC, Stegger M, Stahlhut SG, Hansen DS, Engelthaler DM, Andersen PS, Driebe EM, Keim P, Krogfelt KA (2015) Mapping the evolution of hypervirulent Klebsiella pneumoniae. mBio 6(4):e00630
Shon AS, Russo TA (2012) Hypervirulent Klebsiella pneumoniae: the next superbug? Future Microbiol 7(6):669–671
Fang CT, Lai SY, Yi WC, Hsueh PR, Liu KL, Chang SC (2007) Klebsiella pneumoniae genotype K1: an emerging pathogen that causes septic ocular or central nervous system complications from pyogenic liver abscess. Clin Infect Dis Off Publ Infect Dis Soc Am 45(3):284–293
Lin JC, Koh TH, Lee N, Fung CP, Chang FY, Tsai YK, Ip M, Siu LK (2014) Genotypes and virulence in serotype K2 Klebsiella pneumoniae from liver abscess and non-infectious carriers in Hong Kong, Singapore and Taiwan. Gut Pathog 6:21
Yu WL, Ko WC, Cheng KC, Lee HC, Ke DS, Lee CC, Fung CP, Chuang YC (2006) Association between rmpA and magA genes and clinical syndromes caused by Klebsiella pneumoniae in Taiwan. Clin Infect Dis Off Publ Infect Dis Soc Am 42(10):1351–1358
Russo TA, Olson R, MacDonald U, Beanan J, Davidson BA (2015) Aerobactin, but not yersiniabactin, salmochelin, or enterobactin, enables the growth/survival of hypervirulent (hypermucoviscous) Klebsiella pneumoniae ex vivo and in vivo. Infect Immun 83(8):3325–3333
Kollef MH (2004) Prevention of hospital-associated pneumonia and ventilator-associated pneumonia. Crit Care Med 32(6):1396–1405
American Thoracic S, Infectious Diseases Society of America (2005) Guidelines for the management of adults with hospital-acquired, ventilator-associated, and healthcare-associated pneumonia. Am J Respir Crit Care Med 171(4):388–416
Rello J, Ausina V, Ricart M, Castella J, Prats G (1993) Impact of previous antimicrobial therapy on the etiology and outcome of ventilator-associated pneumonia. Chest 104(4):1230–1235
Knaus WA, Draper EA, Wagner DP, Zimmerman JE (1985) APACHE II: a severity of disease classification system. Crit Care Med 13(10):818–829
Clinical and Laboratory Standards Institute (CLSI) (2013) Performance standards for antimicrobial susceptibility testing; Twenty-third informational supplement. CLSI document M100-S23
Nordmann P, Poirel L, Dortet L (2012) Rapid detection of carbapenemase-producing Enterobacteriaceae. Emerg Infect Dis 18(9):1503–1507
Poirel L, Walsh TR, Cuvillier V, Nordmann P (2011) Multiplex PCR for detection of acquired carbapenemase genes. Diagn Microbiol Infect Dis 70(1):119–123
Sanchez CJ Jr, Mende K, Beckius ML, Akers KS, Romano DR, Wenke JC, Murray CK (2013) Biofilm formation by clinical isolates and the implications in chronic infections. BMC Infect Dis 13:47
Turton JF, Perry C, Elgohari S, Hampton CV (2010) PCR characterization and typing of Klebsiella pneumoniae using capsular type-specific, variable number tandem repeat and virulence gene targets. J Med Microbiol 59(Pt 5):541–547
Tang HL, Chiang MK, Liou WJ, Chen YT, Peng HL, Chiou CS, Liu KS, Lu MC, Tung KC, Lai YC (2010) Correlation between Klebsiella pneumoniae carrying pLVPK-derived loci and abscess formation. Eur J Clin Microbiol Infect Dis Off Publ Eur Soc Clin Microbiol 29(6):689–698
Compain F, Babosan A, Brisse S, Genel N, Audo J, Ailloud F, Kassis-Chikhani N, Arlet G, Decre D (2014) Multiplex PCR for detection of seven virulence factors and K1/K2 capsular serotypes of Klebsiella pneumoniae. J Clin Microbiol 52(12):4377–4380
Diancourt L, Passet V, Verhoef J, Grimont PA, Brisse S (2005) Multilocus sequence typing of Klebsiella pneumoniae nosocomial isolates. J Clin Microbiol 43(8):4178–4182
Deschaght P, Van Simaey L, Decat E, Van Mechelen E, Brisse S, Vaneechoutte M (2011) Rapid genotyping of Achromobacter xylosoxidans, Acinetobacter baumannii, Klebsiella pneumoniae, Pseudomonas aeruginosa and Stenotrophomonas maltophilia isolates using melting curve analysis of RAPD-generated DNA fragments (McRAPD). Res Microbiol 162(4):386–392
Zhang Y, Zeng J, Liu W, Zhao F, Hu Z, Zhao C, Wang Q, Wang X, Chen H, Li H, Zhang F, Li S, Cao B, Wang H (2015) Emergence of a hypervirulent carbapenem-resistant Klebsiella pneumoniae isolate from clinical infections in China. J Infect 71(5):553–560
Lee HC, Chuang YC, Yu WL, Lee NY, Chang CM, Ko NY, Wang LR, Ko WC (2006) Clinical implications of hypermucoviscosity phenotype in Klebsiella pneumoniae isolates: association with invasive syndrome in patients with community-acquired bacteraemia. J Intern Med 259(6):606–614
Luo Y, Wang Y, Ye L, Yang J (2014) Molecular epidemiology and virulence factors of pyogenic liver abscess causing Klebsiella pneumoniae in China. Clin Microbiol Infect Off Publ Eur Soc Clin Microbiol Infect Dis 20(11):O818–O824
Lee SS, Chen YS, Tsai HC, Wann SR, Lin HH, Huang CK, Liu YC (2008) Predictors of septic metastatic infection and mortality among patients with Klebsiella pneumoniae liver abscess. Clin Infect Dis Off Publ Infect Dis Soc Am 47(5):642–650
Lin YT, Siu LK, Lin JC, Chen TL, Tseng CP, Yeh KM, Chang FY, Fung CP (2012) Seroepidemiology of Klebsiella pneumoniae colonizing the intestinal tract of healthy Chinese and overseas Chinese adults in Asian countries. BMC Microbiol 12:13
Su SC, Siu LK, Ma L, Yeh KM, Fung CP, Lin JC, Chang FY (2008) Community-acquired liver abscess caused by serotype K1 Klebsiella pneumoniae with CTX-M-15-type extended-spectrum beta-lactamase. Antimicrob Agents Chemother 52(2):804–805
Andrade LN, Vitali L, Gaspar GG, Bellissimo-Rodrigues F, Martinez R, Darini AL (2014) Expansion and evolution of a virulent, extensively drug-resistant (polymyxin B-resistant), QnrS1-, CTX-M-2-, and KPC-2-producing Klebsiella pneumoniae ST11 international high-risk clone. J Clin Microbiol 52(7):2530–2535
Holt KE, Wertheim H, Zadoks RN, Baker S, Whitehouse CA, Dance D, Jenney A, Connor TR, Hsu LY, Severin J, Brisse S, Cao H, Wilksch J, Gorrie C, Schultz MB, Edwards DJ, Nguyen KV, Nguyen TV, Dao TT, Mensink M, Minh VL, Nhu NT, Schultsz C, Kuntaman K, Newton PN, Moore CE, Strugnell RA, Thomson NR (2015) Genomic analysis of diversity, population structure, virulence, and antimicrobial resistance in Klebsiella pneumoniae, an urgent threat to public health. Proc Natl Acad Sci U S A 112(27):E3574–E3581
Siu LK, Huang DB, Chiang T (2014) Plasmid transferability of KPC into a virulent K2 serotype Klebsiella pneumoniae. BMC Infect Dis 14:176
Wu MC, Lin TL, Hsieh PF, Yang HC, Wang JT (2011) Isolation of genes involved in biofilm formation of a Klebsiella pneumoniae strain causing pyogenic liver abscess. PLoS One 6(8):e23500
Jagnow J, Clegg S (2003) Klebsiella pneumoniae MrkD-mediated biofilm formation on extracellular matrix- and collagen-coated surfaces. Microbiology 149(Pt 9):2397–2405
Chuang YC, Lee MF, Yu WL (2013) Mycotic aneurysm caused by hypermucoviscous Klebsiella pneumoniae serotype K54 with sequence type 29: an emerging threat. Infection 41(5):1041–1044
Hsu CR, Lin TL, Chen YC, Chou HC, Wang JT (2011) The role of Klebsiella pneumoniae rmpA in capsular polysaccharide synthesis and virulence revisited. Microbiology 157(Pt 12):3446–3457
Lawlor MS, O’Connor C, Miller VL (2007) Yersiniabactin is a virulence factor for Klebsiella pneumoniae during pulmonary infection. Infect Immun 75(3):1463–1472
Turton JF, Englender H, Gabriel SN, Turton SE, Kaufmann ME, Pitt TL (2007) Genetically similar isolates of Klebsiella pneumoniae serotype K1 causing liver abscesses in three continents. J Med Microbiol 56(Pt 5):593–597
Lau YJ, Hu BS, Wu WL, Lin YH, Chang HY, Shi ZY (2000) Identification of a major cluster of Klebsiella pneumoniae isolates from patients with liver abscess in Taiwan. J Clin Microbiol 38(1):412–414
Cheng HP, Chang FY, Fung CP, Siu LK (2002) Klebsiella pneumoniae liver abscess in Taiwan is not caused by a clonal spread strain. J Microbiol Immunol Infect 35(2):85–88
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
Funding
This work was supported by Hunan Provincial Natural Science Foundation of China (grant number: 14JJ2022).
Conflict of interest
None declared.
Rights and permissions
About this article
Cite this article
Yan, Q., Zhou, M., Zou, M. et al. Hypervirulent Klebsiella pneumoniae induced ventilator-associated pneumonia in mechanically ventilated patients in China. Eur J Clin Microbiol Infect Dis 35, 387–396 (2016). https://doi.org/10.1007/s10096-015-2551-2
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s10096-015-2551-2