Abstract
Background
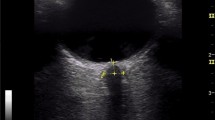
Estimation of intracranial pressure (ICP) may be helpful in the management of neurological critically ill patients. It has been shown that ultrasonography of the optic nerve sheath diameter (ONSD) is a reliable tool for non-invasive estimation of increased intracranial pressure (ICP) at hospital admission or in intensive care. Less is known about the estimation of increased ICP and usefulness of ONSD in the prehospital setting. The aim of this review was to elucidate both prevailing and novel applications of ONSD for neurologists and critical care physicians.
Methods
In this review, we discuss the technique and the novel approach of ONSD measurement, the clinical applications of ONSD in neurology and critical care patients.
Results
ONSD measurement is simple, easy to learn, and has diverse applications. ONSD has utility for ICP measurement in intracranial hemorrhage and ischemic stroke, meningitis and encephalitis, and idiopathic intracranial hypertension (IIH). It is also valuable for lesser known syndromes, where an increase of ICP is postulated, such as acute mountain sickness and posterior reversible encephalopathy syndrome. ONSD changes develop in inflammatory or ischemic optic neuropathies. Some papers demonstrate the usefulness of ONSD studies in symptomatic intracranial hypotension.
Conclusions
ONSD is a safe and low-cost bedside tool with the potential of screening patients who need other neuroimaging and those who may need an invasive measurement of ICP.




Similar content being viewed by others
References
Ertl M et al (2014) Ocular color-coded sonography—a promising tool for neurologists and intensive care physicians. Ultraschall Med 35:422–431. https://doi.org/10.1055/s-0034-1366113
Robba C et al (2018) Optic nerve sheath diameter measured sonographically as non-invasive estimator of intracranial pressure: a systematic review and meta-analysis. Intensive Care Med 44:1284–1294. https://doi.org/10.1007/s00134-018-5305-7
Fichtner J et al (2016) Management of spontaneous intracranial hypotension—transorbital ultrasound as discriminator. J Neurol Neurosurg Psychiatry 87:650–655. https://doi.org/10.1136/jnnp-2015-310853
Geeraerts T, Launey Y, Martin L, Pottecher J, Vigue B, Duranteau J, Benhamou D (2007) Ultrasonography of the optic nerve sheath may be useful for detecting raised intracranial pressure after severe brain injury. Intensive Care Med 33:1704–1711. https://doi.org/10.1007/s00134-007-0797-6
Geeraerts T, Merceron S, Benhamou D, Vigue B, Duranteau J (2008) Non-invasive assessment of intracranial pressure using ocular sonography in neurocritical care patients. Intensive Care Med 34:2062–2067. https://doi.org/10.1007/s00134-008-1149-x
Lochner P, Leone MA, Coppo L, Nardone R, Zedde ML, Cantello R, Brigo F (2016) B-mode transorbital ultrasononography for the diagnosis of acute optic neuritis. A systematic review. Clin Neurophysiol 127:803–809. https://doi.org/10.1016/j.clinph.2015.05.005
Rohr A et al (2010) MR imaging of the optic nerve sheath in patients with craniospinal hypotension. AJNR Am J Neuroradiol 31:1752–1757. https://doi.org/10.3174/ajnr.A2120
Wilson MH, Wright A, Imray CH (2014) Intracranial pressure at altitude. High Alt Med Biol 15:123–132. https://doi.org/10.1089/ham.2013.1151
Hansen HC, Helmke K (1997) Validation of the optic nerve sheath response to changing cerebrospinal fluid pressure: ultrasound findings during intrathecal infusion tests. J Neurosurg 87:34–40. https://doi.org/10.3171/jns.1997.87.1.0034
Helmke K, Hansen HC (1996) Fundamentals of transorbital sonographic evaluation of optic nerve sheath expansion under intracranial hypertension II. Patient study. Pediatr Radiol 26:706–710
Liu D, Li Z, Zhang X, Zhao L, Jia J, Sun F, Wang Y, Ma D, Wei W (2017) Assessment of intracranial pressure with ultrasonographic retrobulbar optic nerve sheath diameter measurement. BMC Neurol 17:188. https://doi.org/10.1186/s12883-017-0964-5
Lochner P et al (2019) Simulation and experimental characterization of lateral imaging resolution of ultrasound systems and assessment of system suitability for acoustic optic nerve sheath diameter measurement. J Neuroimaging 29:34–41. https://doi.org/10.1111/jon.12578
Fowlkes JB, Holland CK (2000) Mechanical bioeffects from diagnostic ultrasound: AIUM consensus statements. American Institute of Ultrasound in Medicine. J Ultrasound Med 19:69–72
Ballantyne SA, O'Neill G, Hamilton R, Hollman AS (2002) Observer variation in the sonographic measurement of optic nerve sheath diameter in normal adults. Eur J Ultrasound 15:145–149
Bauerle J, Lochner P, Kaps M, Nedelmann M (2012) Intra- and interobsever reliability of sonographic assessment of the optic nerve sheath diameter in healthy adults. J Neuroimaging 22:42–45. https://doi.org/10.1111/j.1552-6569.2010.00546.x
Lochner P, Coppo L, Cantello R, Nardone R, Naldi A, Leone MA, Brigo F (2016) Intra- and interobserver reliability of transorbital sonographic assessment of the optic nerve sheath diameter and optic nerve diameter in healthy adults. J Ultrasound 19:41–45. https://doi.org/10.1007/s40477-014-0144-z
Copetti R, Cattarossi L (2009) Optic nerve ultrasound: artifacts and real images. Intensive Care Med 35:1488–1489; author reply 1490-1481. https://doi.org/10.1007/s00134-009-1494-4
Bauerle J, Schuchardt F, Schroeder L, Egger K, Weigel M, Harloff A (2013) Reproducibility and accuracy of optic nerve sheath diameter assessment using ultrasound compared to magnetic resonance imaging. BMC Neurol 13:187. https://doi.org/10.1186/1471-2377-13-187
Helmke K, Hansen HC (1996) Fundamentals of transorbital sonographic evaluation of optic nerve sheath expansion under intracranial hypertension. I. Experimental study. Pediatr Radiol 26:701–705
Krogias C, Ayzenberg I, Schroeder C, Gruter T, Gold R, Yoon MS (2016) Transorbital sonography in CIDP patients: no evidence for optic nerve hypertrophy. J Neurol Sci 362:206–208. https://doi.org/10.1016/j.jns.2016.01.049
Topcuoglu MA, Arsava EM, Bas DF, Kozak HH (2015) Transorbital ultrasonographic measurement of optic nerve sheath diameter in brain death. J Neuroimaging 25:906–909. https://doi.org/10.1111/jon.12233
Tayal VS, Neulander M, Norton HJ, Foster T, Saunders T, Blaivas M (2007) Emergency department sonographic measurement of optic nerve sheath diameter to detect findings of increased intracranial pressure in adult head injury patients. Ann Emerg Med 49:508–514. https://doi.org/10.1016/j.annemergmed.2006.06.040
Bauerle J, Nedelmann M (2011) Sonographic assessment of the optic nerve sheath in idiopathic intracranial hypertension. J Neurol 258:2014–2019. https://doi.org/10.1007/s00415-011-6059-0
Chen LM, Wang LJ, Hu Y, Jiang XH, Wang YZ, Xing YQ (2019) Ultrasonic measurement of optic nerve sheath diameter: a non-invasive surrogate approach for dynamic, real-time evaluation of intracranial pressure. Br J Ophthalmol 103:437–441. https://doi.org/10.1136/bjophthalmol-2018-312934
Ertl M, Aigner R, Krost M, Karnasova Z, Muller K, Naumann M, Schlachetzki F (2017) Measuring changes in the optic nerve sheath diameter in patients with idiopathic normal-pressure hydrocephalus: a useful diagnostic supplement to spinal tap tests. Eur J Neurol 24:461–467. https://doi.org/10.1111/ene.13225
Naldi A et al (2019) Ultrasonography monitoring of optic nerve sheath diameter and retinal vessels in patients with cerebral hemorrhage. J Neuroimaging. https://doi.org/10.1111/jon.12604
Skoloudik D et al (2011) Distal enlargement of the optic nerve sheath in the hyperacute stage of intracerebral haemorrhage. Br J Ophthalmol 95:217–221. https://doi.org/10.1136/bjo.2009.172890
Yesilaras M, Kilic TY, Yesilaras S, Atilla OD, Oncel D, Camlar M (2017) The diagnostic and prognostic value of the optic nerve sheath diameter on CT for diagnosis spontaneous subarachnoid hemorrhage. Am J Emerg Med 35:1408–1413. https://doi.org/10.1016/j.ajem.2017.04.022
Bauerle J, Niesen WD, Egger K, Buttler KJ, Reinhard M (2016) Enlarged optic nerve sheath in aneurysmal subarachnoid hemorrhage despite normal intracranial pressure. J Neuroimaging 26:194–196. https://doi.org/10.1111/jon.12287
Gokcen E, Caltekin I, Savrun A, Korkmaz H, Savrun ST, Yildirim G (2017) Alterations in optic nerve sheath diameter according to cerebrovascular disease sub-groups. Am J Emerg Med 35:1607–1611. https://doi.org/10.1016/j.ajem.2017.04.073
D Amico D, Curone M, Ciasca P, Cammarata G, Melzi L, Bussone G, Bianchi Marzoli S (2013) Headache prevalence and clinical features in patients with idiopathic intracranial hypertension (IIH). Neurol Sci 34(Suppl 1):S147–S149. https://doi.org/10.1007/s10072-013-1388-7
Friedman DI, Liu GT, Digre KB (2013) Revised diagnostic criteria for the pseudotumor cerebri syndrome in adults and children. Neurology 81:1159–1165. https://doi.org/10.1212/WNL.0b013e3182a55f17
Raoof N, Sharrack B, Pepper IM, Hickman SJ (2011) The incidence and prevalence of idiopathic intracranial hypertension in Sheffield, UK. Eur J Neurol 18:1266–1268. https://doi.org/10.1111/j.1468-1331.2011.03372.x
Lochner P, Nardone R, Tezzon F, Coppo L, Brigo F (2013) Optic nerve sonography to monitor treatment efficacy in idiopathic intracranial hypertension: a case report. J Neuroimaging 23:533–534. https://doi.org/10.1111/jon.12005
Lochner P, Brigo F, Zedde ML, Sanguigni S, Coppo L, Nardone R, Naldi A, Sola D, Stolz E (2016) Feasibility and usefulness of ultrasonography in idiopathic intracranial hypertension or secondary intracranial hypertension. BMC Neurol 16:85. https://doi.org/10.1186/s12883-016-0594-3
Lochner P et al (2018) B-mode transorbital ultrasonography for the diagnosis of idiopathic intracranial hypertension: a systematic review and meta-analysis. Ultraschall Med. https://doi.org/10.1055/a-0719-4903
Lochner P, Fassbender K, Lesmeister M, Nardone R, Orioli A, Brigo F, Stolz E (2018) Ocular ultrasound for monitoring pseudotumor cerebri syndrome. J Neurol 265:356–361. https://doi.org/10.1007/s00415-017-8699-1
Headache Classification Committee of the International Headache Society (IHS) (2018) The international classification of headache disorders, 3rd edition. Cephalalgia 38:1–211. https://doi.org/10.1177/0333102417738202
Dubost C, Le Gouez A, Zetlaoui PJ, Benhamou D, Mercier FJ, Geeraerts T (2011) Increase in optic nerve sheath diameter induced by epidural blood patch: a preliminary report. Br J Anaesth 107:627–630. https://doi.org/10.1093/bja/aer186
Fugate JE, Claassen DO, Cloft HJ, Kallmes DF, Kozak OS, Rabinstein AA (2010) Posterior reversible encephalopathy syndrome: associated clinical and radiologic findings. Mayo Clin Proc 85:427–432. https://doi.org/10.4065/mcp.2009.0590
Lee VH, Wijdicks EF, Manno EM, Rabinstein AA (2008) Clinical spectrum of reversible posterior leukoencephalopathy syndrome. Arch Neurol 65:205–210. https://doi.org/10.1001/archneurol.2007.46
Uchino M, Haga D, Nomoto J, Mito T, Kuramitsu T (2007) Brainstem involvement in hypertensive encephalopathy: a report of two cases and literature review. Eur Neurol 57:223–226. https://doi.org/10.1159/000100015
Caputo ND, Fraser RM, Abdulkarim J (2012) Posterior reversible encephalopathy syndrome presenting as papilledema. Am J Emerg Med 30:835 e835-837. https://doi.org/10.1016/j.ajem.2011.03.016
Lochner P, Mader C, Nardone R, Cantello R, Orioli A, Brigo F (2014) Usefulness of ultrasonography in posterior reversible encephalopathy syndrome. Neurol Sci 35:475–477. https://doi.org/10.1007/s10072-013-1562-y
Lochner P, Nardone R, Brigo F, Tamber MS, Zuccoli G (2015) The diagnosis of posterior reversible encephalopathy syndrome. Lancet Neurol 14:1074–1075. https://doi.org/10.1016/S1474-4422(15)00256-2
Nabeta HW et al (2014) Accuracy of noninvasive intraocular pressure or optic nerve sheath diameter measurements for predicting elevated intracranial pressure in cryptococcal meningitis. Open Forum Infect Dis 1:ofu093. https://doi.org/10.1093/ofid/ofu093
Sangani SV, Parikh S (2015) Can sonographic measurement of optic nerve sheath diameter be used to detect raised intracranial pressure in patients with tuberculous meningitis? A prospective observational study. Indian J Radiol Imaging 25:173–176. https://doi.org/10.4103/0971-3026.155869
Lawley JS, Alperin N, Bagci AM, Lee SH, Mullins PG, Oliver SJ, Macdonald JH (2014) Normobaric hypoxia and symptoms of acute mountain sickness: elevated brain volume and intracranial hypertension. Ann Neurol 75:890–898. https://doi.org/10.1002/ana.24171
Ross RT (1985) The random nature of cerebral mountain sickness. Lancet 1:990–991
Lawley JS, Oliver SJ, Mullins P, Morris D, Junglee NA, Jelleyman C, Macdonald JH (2012) Optic nerve sheath diameter is not related to high altitude headache: a randomized controlled trial. High Alt Med Biol 13:193–199. https://doi.org/10.1089/ham.2012.1019
Strapazzon G, Brugger H, Dal Cappello T, Procter E, Hofer G, Lochner P (2014) Factors associated with optic nerve sheath diameter during exposure to hypobaric hypoxia. Neurology 82:1914–1918. https://doi.org/10.1212/WNL.0000000000000457
Sutherland AI, Morris DS, Owen CG, Bron AJ, Roach RC (2008) Optic nerve sheath diameter, intracranial pressure and acute mountain sickness on Mount Everest: a longitudinal cohort study. Br J Sports Med 42:183–188. https://doi.org/10.1136/bjsm.2007.045286
Fagenholz PJ, Gutman JA, Murray AF, Noble VE, Camargo CA Jr, Harris NS (2009) Optic nerve sheath diameter correlates with the presence and severity of acute mountain sickness: evidence for increased intracranial pressure. J Appl Physiol 106:1207–1211. https://doi.org/10.1152/japplphysiol.01188.2007
Lochner P, Falla M, Brigo F, Pohl M, Strapazzon G (2015) Ultrasonography of the optic nerve sheath diameter for diagnosis and monitoring of acute mountain sickness: a systematic review. High Alt Med Biol 16:195–203. https://doi.org/10.1089/ham.2014.1127
Lee HC, Lee WJ, Dho YS, Cho WS, Kim YH, Park HP (2018) Optic nerve sheath diameter based on preoperative brain computed tomography and intracranial pressure are positively correlated in adults with hydrocephalus. Clin Neurol Neurosurg 167:31–35. https://doi.org/10.1016/j.clineuro.2018.02.012
Brzezinska R, Schumacher R (2002) Diagnosis of elevated intracranial pressure in children with shunt under special consideration of transglobe sonography of the optic nerve. Ultraschall Med 23:325–332. https://doi.org/10.1055/s-2002-35050
Newman WD, Hollman AS, Dutton GN, Carachi R (2002) Measurement of optic nerve sheath diameter by ultrasound: a means of detecting acute raised intracranial pressure in hydrocephalus. Br J Ophthalmol 86:1109–1113
Foroozan R, Buono LM, Savino PJ, Sergott RC (2002) Acute demyelinating optic neuritis. Curr Opin Ophthalmol 13:375–380
Youl BD et al (1991) The pathophysiology of acute optic neuritis. An association of gadolinium leakage with clinical and electrophysiological deficits. Brain 114(Pt 6):2437–2450
Dehghani A, Giti M, Akhlaghi MR, Karami M, Salehi F (2012) Ultrasonography in distinguishing optic neuritis from nonarteritic anterior ischemic optic neuropathy. Adv Biomed Res 1:3. https://doi.org/10.4103/2277-9175.94425
Elvin A, Andersson T, Soderstrom M (1998) Optic neuritis. Doppler ultrasonography compared with MR and correlated with visual evoked potential assessments. Acta Radiol 39:243–248
Gerling J, Janknecht P, Hansen LL, Kommerell G (1997) Diameter of the optic nerve in idiopathic optic neuritis and in anterior ischemic optic neuropathy. Int Ophthalmol 21:131–135
Karami M, Janghorbani M, Dehghani A, Riahinejad M (2012) Orbital Doppler evaluation of blood flow velocities in optic neuritis. Korean J Ophthalmol 26:116–122. https://doi.org/10.3341/kjo.2012.26.2.116
Lochner P et al (2014) Transorbital sonography in acute optic neuritis: a case-control study. AJNR Am J Neuroradiol 35:2371–2375. https://doi.org/10.3174/ajnr.A4051
Neroev VV, Karlova IZ, Zaitseva OV, Kruzhkova GV, Boiko AN (2001) Role of ultrasonic B-scanning in differential diagnosis and prognosis of the course of optic neuritis. Vestn oftalmol 117:25–29
Stefanovic IB, Jovanovic M, Krnjaja BD, Veselinovic D, Jovanovic P (2010) Influence of retrobulbar neuritis and papillitis on echographically measured optic nerve diameter. Vojnosanit Pregl 67:32–35
Block HS, Biller J (2014) Neurology of pregnancy. Handb Clin Neurol 121:1595–1622. https://doi.org/10.1016/B978-0-7020-4088-7.00105-X
Dubost C, Le Gouez A, Jouffroy V, Roger-Christoph S, Benhamou D, Mercier FJ, Geeraerts T (2012) Optic nerve sheath diameter used as ultrasonographic assessment of the incidence of raised intracranial pressure in preeclampsia: a pilot study. Anesthesiology 116:1066–1071. https://doi.org/10.1097/ALN.0b013e318246ea1a
Brzan Simenc G, Ambrozic J, Prokselj K, Tul N, Cvijic M, Mirkovic T, Lucovnik M (2018) Ocular ultrasonography for diagnosing increased intracranial pressure in patients with severe preeclampsia. Int J Obstet Anesth 36:49–55. https://doi.org/10.1016/j.ijoa.2018.06.005
Bernal W, Wendon J (1999) Acute liver failure; clinical features and management. Eur J Gastroenterol Hepatol 11:977–984
Ware AJ, D’Agostino AN, Combes B (1971) Cerebral edema: a major complication of massive hepatic necrosis. Gastroenterology 61:877–884
Karvellas CJ, Fix OK, Battenhouse H, Durkalski V, Sanders C, Lee WM, Group USALFS (2014) Outcomes and complications of intracranial pressure monitoring in acute liver failure: a retrospective cohort study. Crit Care Med 42:1157–1167. https://doi.org/10.1097/CCM.0000000000000144
Peck M, Wendon J, Sizer E, Auzinger G, Bernal W (2010) Intracranial pressure monitoring in acute liver failure: a review of 10 years experience. Crit Care 14:P542
Vaquero J et al (2005) Complications and use of intracranial pressure monitoring in patients with acute liver failure and severe encephalopathy. Liver Transpl 11:1581–1589. https://doi.org/10.1002/lt.20625
Rajajee V, Williamson CA, Fontana RJ, Courey AJ, Patil PG (2018) Noninvasive intracranial pressure assessment in acute liver failure. Neurocrit Care 29:280–290. https://doi.org/10.1007/s12028-018-0540-x
Ganschow R, Nolkemper D, Helmke K, Harps E, Commentz JC, Broering DC, Pothmann W, Rogiers X, Hellwege HH, Burdelski M (2000) Intensive care management after pediatric liver transplantation: a single-center experience. Pediatr Transplant 4:273–279
Chelly J et al (2016) The optic nerve sheath diameter as a useful tool for early prediction of outcome after cardiac arrest: a prospective pilot study. Resuscitation 103:7–13. https://doi.org/10.1016/j.resuscitation.2016.03.006
Chae MK et al (2016) Better prognostic value with combined optic nerve sheath diameter and grey-to-white matter ratio on initial brain computed tomography in post-cardiac arrest patients. Resuscitation 104:40–45. https://doi.org/10.1016/j.resuscitation.2016.04.001
Ueda T, Ishida E, Kojima Y, Yoshikawa S, Yonemoto H (2015) Sonographic optic nerve sheath diameter: a simple and rapid tool to assess the neurologic prognosis after cardiac arrest. J Neuroimaging 25:927–930. https://doi.org/10.1111/jon.12246
Ertl M, Weber S, Hammel G, Schroeder C, Krogias C (2018) Transorbital sonography for early prognostication of hypoxic-ischemic encephalopathy after cardiac arrest. J Neuroimaging 28:542–548. https://doi.org/10.1111/jon.12528
You Y et al (2018) Relationship between time related serum albumin concentration, optic nerve sheath diameter, cerebrospinal fluid pressure, and neurological prognosis in cardiac arrest survivors. Resuscitation 131:42–47. https://doi.org/10.1016/j.resuscitation.2018.08.003
Citerio G, Vascotto E, Villa F, Celotti S, Pesenti A (2001) Induced abdominal compartment syndrome increases intracranial pressure in neurotrauma patients: a prospective study. Crit Care Med 29:1466–1471
Cooke SJ, Paterson-Brown S (2001) Association between laparoscopic abdominal surgery and postoperative symptoms of raised intracranial pressure. Surg Endosc 15:723–725
Ficarra V et al (2009) Retropubic, laparoscopic, and robot-assisted radical prostatectomy: a systematic review and cumulative analysis of comparative studies. Eur Urol 55:1037–1063. https://doi.org/10.1016/j.eururo.2009.01.036
Kim MS, Bai SJ, Lee JR, Choi YD, Kim YJ, Choi SH (2014) Increase in intracranial pressure during carbon dioxide pneumoperitoneum with steep trendelenburg positioning proven by ultrasonographic measurement of optic nerve sheath diameter. J Endourol 28:801–806. https://doi.org/10.1089/end.2014.0019
Robba C et al (2016) Effects of pneumoperitoneum and Trendelenburg position on intracranial pressure assessed using different non-invasive methods. Br J Anaesth 117:783–791. https://doi.org/10.1093/bja/aew356
Kim EJ, Koo BN, Choi SH, Park K, Kim MS (2018) Ultrasonographic optic nerve sheath diameter for predicting elevated intracranial pressure during laparoscopic surgery: a systematic review and meta-analysis. Surg Endosc 32:175–182. https://doi.org/10.1007/s00464-017-5653-3
Ertl M, Schierling W, Kasprzak P, Schomig B, Bruckl C, Schlachetzki F, Pfister K (2015) Optic nerve sheath diameter measurement to identify high-risk patients for spinal ischemia after endovascular thoracoabdominal aortic aneurysm repair. J Neuroimaging 25:910–915. https://doi.org/10.1111/jon.12234
Houze-Cerfon CH, Bounes V, Guemon J, Le Gourrierec T, Geeraerts T (2019) Quality and feasibility of sonographic measurement of the optic nerve sheath diameter to estimate the risk of raised intracranial pressure after traumatic brain injury in prehospital setting. Prehosp Emerg Care 23:277–283. https://doi.org/10.1080/10903127.2018.1501444
Maissan IM, Verbaan LA, van den Berg M, Houmes RJ, Stolker RJ, den Hartog D (2018) Helicopter transportation increases intracranial pressure: a proof-of-principle study. Air Med J 37:249–252. https://doi.org/10.1016/j.amj.2018.02.010
Meiburger KM, Acharya UR, Molinari F (2018) Automated localization and segmentation techniques for B-mode ultrasound images: a review. Comput Biol Med 92:210–235. https://doi.org/10.1016/j.compbiomed.2017.11.018
Gerber S et al (2017) Automatic estimation of the optic nerve sheath diameter from ultrasound images imaging for patient-customized simulations and systems for point-of-care ultrasound : International Workshops, BIVPCS 2017 and POCUS 2017, held in conjunction with MICCAI 2017, Quebec City, QC 10549:113–120 https://doi.org/10.1007/978-3-319-67552-7_14
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
This article does not contain any studies with human participants or animals performed by any of the authors.
Conflict of interest
The authors declare that they have no conflict of interest.
Additional information
Publisher’s note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Rights and permissions
About this article
Cite this article
Lochner, P., Czosnyka, M., Naldi, A. et al. Optic nerve sheath diameter: present and future perspectives for neurologists and critical care physicians. Neurol Sci 40, 2447–2457 (2019). https://doi.org/10.1007/s10072-019-04015-x
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s10072-019-04015-x