Abstract:
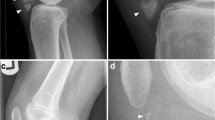
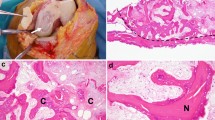
A retrospective review of the frontal and lateral knee radiographs of 200 patients with calcium pyrophosphate dihydrate (CPPD) crystal deposition disease was performed. Of these 200 patients, nine patients (four male, five female, mean age 74 years, age range 63–87 years) had radiographic findings simulating osteonecrosis of the knee. One patient also had magnetic resonance imaging of the involved knee. A total of 10 knee radiographs in nine patients showed articular and periarticular calcification diagnostic of CPPD crystal deposition of the knee. In addition, all 10 radiographs showed flattening of one femoral condyle. Four of the 10 cases demonstrated an area of radiolucency in the subchondral bone surrounded by a halo of sclerosis. Eight of the 10 cases had narrowing of the involved joint compartment and osteophytosis. These findings mimic the radiographic signs of spontaneous osteonecrosis of the knee. In conclusion, flattening of the femoral condyles in CPPD crystal deposition disease simulates that of spontaneous osteonecrosis and probably relates to articular cartilage and meniscal damage that subsequently leads to stress fracture of subchondral bone with bone collapse.
Similar content being viewed by others
Author information
Authors and Affiliations
Additional information
Received: 4 August 1998 / Accepted: 8 April 1999
Rights and permissions
About this article
Cite this article
Kwak, S., Resnick, D. & Haghighi, P. Calcium Pyrophosphate Dihydrate Crystal Deposition Disease of the Knee Simulating Spontaneous Osteonecrosis. Clin Rheumatol 18, 390–393 (1999). https://doi.org/10.1007/s100670050124
Issue Date:
DOI: https://doi.org/10.1007/s100670050124