Abstract
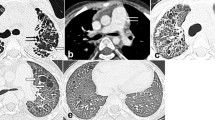
To characterize the distinctive chest high-resolution computerized tomography (HRCT) features and clinical manifestations of primary Sjögren syndrome (pSS)-related interstitial lung disease (ILD). The demographic data, clinical manifestations, and laboratory and radiological findings of 527 pSS patients were retrospectively analyzed. ILD was defined based on the presences of pulmonary signs in HRCT. Two hundred six of 527 patients were diagnosed as pSS-ILD, and the prevalence was 39.1%. The three most frequent abnormalities in HRCT were reticular pattern (92.7%), ground-glass attenuation (87.4%), and bronchovascular bundle thickening (82%). One hundred twenty-four cases (60.2%) of the pSS-ILD patients had only a single HRCT pattern, which involved 86 non-specific interstitial pneumonitis (NSIP) cases (41.7%), 22 usual interstitial pneumonia (UIP) cases (10.68%), 8 organizing pneumonia (OP) cases (3.9%), and 8 lymphocytic interstitial pneumonia (LIP) cases (3.9%), respectively. Besides, the more important observation was that 82 cases had no less than two HRCT patterns, and NSIP admixed with OP (43.9%), NSIP admixed with UIP (35.4%), and NSIP admixed with LIP (19.5%) were the most frequent. HRCT of pSS-ILD patients demonstrated bilateral infiltrates (99%), with abnormalities predominantly in the lower lobes (89.3%) and subpleural areas (81.1%), and a few lesions were characterized by hilum distributed (8.7%). Pulmonary function tests (PFTs) revealed impaired diffusion capacity for carbon monoxide and total lung capacity, and the rate of small airway lesions in the pSS-ILD patients was 3.5 times higher in patients of pSS. Logistic regression analysis showed that dry cough (OR 59.05), clubbing (OR 6.26), elevated lactate dehydrogenase (OR 21.38) and positive anti-Ro (OR 7.86) were relevant factors of pSS-ILD. ILD is the common pulmonary involvement of pSS and the prevalence of pSS-ILD is 39.1%. The single pattern of NSIP and UIP in HRCT are the commonest, and about 40% of the pSS-ILD patients possess multiple patterns in HRCT. The classification of idiopathic pulmonary fibrosis cannot completely include the pulmonary imaging features of pSS-ILD.
Similar content being viewed by others
References
Palm O, Garen T, Berge Enger T, Jensen JL, Lund MB, Aalokken TM, Gran JT (2013) Clinical pulmonary involvement in primary Sjogren’s syndrome: prevalence, quality of life and mortality-a retrospective study based on registry data[J]. Rheumatology 52(1):173–179
Ito I, Nagai S, Kitaichi M, Nicholson AG, Johkoh T, Noma S, Kim DS, Handa T, Izumi T, Mishima M (2005) Pulmonary manifestations of primary Sjogren’s syndrome: a clinical, radiologic, and pathologic study[J]. Am J Resp Crit Care 171(6):632–638
Sebastian A, Misterska-Skora M, Silicki J, Sebastian M, Wiland P (2017) Chest HRCT findings in patients with primary Sjogren’s syndrome[J]. Adv Clin Exp Med 26(7):1101–1106
Yazisiz V, Arslan G, Ozbudak IH, Turker S, Erbasan F, Avci AB, Ozbudak O, Terzioglu E (2010) Lung involvement in patients with primary Sjogren’s syndrome: what are the predictors? [J]. Rheumatol Int 30(10):1317–1324
Shi JH, Liu HR, Xu WB, Feng RE, Zhang ZH, Tian XL, Zhu YJ (2009) Pulmonary manifestations of Sjogren’s syndrome[J]. Respiration 78(4):377–386
Li X, Xu B, Ma Y, Li X, Cheng Q, Wang X, Wang G, Qian L, Wei L (2015) Clinical and laboratory profiles of primary Sjogren’s syndrome in a Chinese population: a retrospective analysis of 315 patients[J]. Int J Rheum Dis 18(4):439–446
Travis WD, Costabel U, Hansell DM, King TE Jr, Lynch DA, Nicholson AG, Ryerson CJ, Ryu JH, Selman M, Wells AU, Behr J, Bouros D, Brown KK, Colby TV, Collard HR, Cordeiro CR, Cottin V, Crestani B, Drent M, Dudden RF, Egan J, Flaherty K, Hogaboam C, Inoue Y, Johkoh T, Kim DS, Kitaichi M, Loyd J, Martinez FJ, Myers J, Protzko S, Raghu G, Richeldi L, Sverzellati N, Swigris J, Valeyre D (2013) An official American Thoracic Society/European Respiratory Society statement: update of the international multidisciplinary classification of the idiopathic interstitial pneumonias[J]. Am J Resp Crit Care 188(6):733–748
Vitali C, Bombardieri S, Jonsson R et al (2002) Classification criteria for Sjogren’s syndrome: a revised version of the European criteria proposed by the American-European Consensus Group[J]. Ann Rheum Dis 61(6):554–558
Shiboski CH, Shiboski SC, Seror R et al (2016) American College of Rheumatology/European League Against Rheumatism Classification Criteria for primary Sjogren’s syndrome: a consensus and data-driven methodology involving three international patient cohorts[J]. Arthritis Rheumatol, 2017 69(1):35–45
Guo X, Bao N, Lei Z et al (2011) Quantitative comparative analysis of high-resolution CT features of idiopathic interstitial pneumonia[J]. Chin J Med 1:11–15
Nannini C, Jebakumar AJ, Crowson CS et al (2013) Primary Sjogren’s syndrome 1976-2005 and associated interstitial lung disease: a population-based study of incidence and mortality[J]. BMJ Open 3(11):003569–003576
Deheinzelin D, Capelozzi VL, Kairalla RA, Barbas Filho JV, Saldiva PH, de Carvalho CR. Interstitial lung disease in primary Sjogren’s syndrome. Clinical-pathological evaluation and response to treatment[J]. Am J Resp Crit Care, 1996, 154(3 Pt 1):794–799
Garcia-Carrasco M, Ramos-Casals M, Rosas J et al (2002) Primary Sjogren syndrome: clinical and immunologic disease patterns in a cohort of 400 patients[J]. Medicine 81(4):270–280
Stojan G, Baer AN, Danoff SK (2013) Pulmonary manifestations of Sjogren’s syndrome[J]. Curr Allergy Asthma Rep 13(4):354–360
Parambil JG, Myers JL, Lindell RM, Matteson EL, Ryu JH (2006) Interstitial lung disease in primary Sjogren syndrome[J]. Chest 130(5):1489–1495
Pertovaara M, Pukkala E, Laippala P et al (2001) A longitudinal cohort study of Finnish patients with primary Sjogren’s syndrome: clinical, immunological, and epidemiological aspects[J]. Ann Rheum Dis 60(5):467–472
Baldini C, Pepe P, Quartuccio L, Priori R, Bartoloni E, Alunno A, Gattamelata A, Maset M, Modesti M, Tavoni A, de Vita S, Gerli R, Valesini G, Bombardieri S (2014) Primary Sjogren’s syndrome as a multi-organ disease: impact of the serological profile on the clinical presentation of the disease in a large cohort of Italian patients[J]. Rheumatology 53(5):839–844
Flament T, Bigot A, Chaigne B, Henique H, Diot E, Marchand-Adam S (2016) Pulmonary manifestations of Sjogren’s syndrome[J]. Eur Respir Rev 25(140):110–123
Roca F, Dominique S, Schmidt J, Smail A, Duhaut P, Lévesque H, Marie I (2017) Interstitial lung disease in primary Sjogren’s syndrome[J]. Autoimmun Rev 16(1):48–54
Manfredi A, Sebastiani M, Cerri S, Cassone G, Bellini P, Casa GD, Luppi F, Ferri C (2017) Prevalence and characterization of non-sicca onset primary Sjogren syndrome with interstitial lung involvement[J]. Clin Rheumatol 36(6):1261–1268
Matsuyama N, Ashizawa K, Okimoto T, Kadota J, Amano H, Hayashi K (2003) Pulmonary lesions associated with Sjogren’s syndrome: radiographic and CT findings[J]. Br J Radiol 76(912):880–884
Lin DF, Yan SM, Zhao Y et al (2010) Clinical and prognostic characteristics of 573 cases of primary Sjogren’s syndrome[J]. Chin Med J 123(22):3252–3257
Ramos-Casals M, Solans R, Rosas J, Camps MT, Gil A, del Pino-Montes J, Calvo-Alen J, Jiménez-Alonso J, Micó ML, Beltrán J, Belenguer R, Pallarés L (2008) Primary Sjogren syndrome in Spain: clinical and immunologic expression in 1010 patients[J]. Medicine 87(4):210–219
Huber AM, Mamyrova G, Lachenbruch PA, Lee JA, Katz JD, Targoff IN, Miller FW, Rider LG, for the Childhood Myositis Heterogeneity Collaborative Study Group (2014) Early illness features associated with mortality in the juvenile idiopathic inflammatory myopathies[J]. Arthritis Care Res 66(5):732–740
Zheng Y (2015) A new understanding of interstitial lung disease in connective tissue[J]. Chin J Rheumatol 9:577–579
Mekinian A, Nicaise-Roland P, Chollet-Martin S, Fain O, Crestani B (2013) Anti-SSA Ro52/Ro60 antibody testing by immunodot could help the diagnosis of Sjogren’s syndrome in the absence of anti-SSA/SSB antibodies by ELISA[J]. Rheumatology (Oxford) 52(12):2223–2228
Sambataro D, Sambataro G, Dal Bosco Y, Polosa R (2017) Present and future of biologic drugs in primary Sjogren’s syndrome[J]. Expert Opin Biol Th 17(1):63–75
Espinosa A, Dardalhon V, Brauner S et al (2009) Loss of the lupus autoantigen Ro52/Trim21 induces tissue inflammation and systemic autoimmunity by disregulating the IL-23-Th17 pathway[J]. Medicine 206(8):1661–1671
Kusume K (1991) Lung injury in idiopathic pulmonary fibrosis and measurement of immunoreactive neutrophil elastase and alpha 1-protease inhibitor in blood[J]. Nihon Kyobu Shikkan Gakkai Zasshi 29(10):1254–1260
Zhang Y, Li H, Wu N, Dong X, Zheng Y (2017) Retrospective study of the clinical characteristics and risk factors of rheumatoid arthritis-associated interstitial lung disease[J]. Clin Rheumatol 36(4):817–823
Yazisiz V, Ozbudak IH, Nizam I, Erbasan F, Avci AB, Ozbudak O, Terzioglu E (2010) A case of primary Sjogren’s syndrome with pulmonary-limited Wegener’s granulomatosis[J]. Rheumatol Int 30(9):1235–1238
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
Disclosures
None.
Rights and permissions
About this article
Cite this article
Dong, X., Zhou, J., Guo, X. et al. A retrospective analysis of distinguishing features of chest HRCT and clinical manifestation in primary Sjögren’s syndrome-related interstitial lung disease in a Chinese population. Clin Rheumatol 37, 2981–2988 (2018). https://doi.org/10.1007/s10067-018-4289-6
Received:
Revised:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s10067-018-4289-6