Abstract
Objective
To determine high resolution CT (HRCT) patterns of pulmonary fibrosis (PF) in children; and their etiological correlates.
Methods
This was a retrospective study involving 149 children with diffuse lung disease (DLD). Patterns of involvement were classified based on dominant lung finding as ground glass opacity (GGO) dominant, nodule dominant, cystic lung disease, or PF.
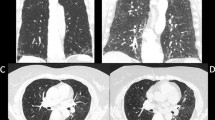
Patterns of PF were classified based on distribution and morphology into airway centric fibrosis (ACF), subpleural fibrosis (SPF), progressive massive fibrosis (PMF) and fibrocavitary. A comparison was made between the two dominant groups for apicobasal distribution, associated findings (GGO, nodules, cysts), and pulmonary artery hypertension (PAH).
Results
Nineteen patients showed PF on HRCT. ACF was commonest (52.6%), followed by SPF (42.1%). The common etiology was sarcoidosis (30%) in ACF, and connective tissue disorders (CTD) (50%) in SPF. Significant difference was found between ACF and SPF in apicobasal distribution (p = 0.04), presence of nodules (p = 0.03), and cysts (p = 0.02).
Conclusion
PF may present as an end stage of several childhood lung diseases. PF on imaging has discernible morphological patterns that correlate with underlying etiology.



Similar content being viewed by others
References
Semple TR, Ashworth MT, Owens CM. Interstitial lung disease in children made easier…well, almost. Radiographics. 2017;37:1679–703.
Kurland G, Deterding RR, Hagood JS, et al. American Thoracic Society Committee on Childhood Interstitial Lung Disease (chILD) and the chILD Research Network. An official American Thoracic Society clinical practice guideline: classification, evaluation, and management of childhood interstitial lung disease in infancy. Am J Respir Crit Care Med. 2013;188:376–94.
Deutsch GH, Young LR, Deterding RR, et al. Diffuse lung disease in young children: application of a novel classification scheme. Am J Respir Crit Care Med. 2007;176:1120–8.
Rice A, Tran-Dang MA, Bush A, Nicholson AG. Diffuse lung disease in infancy and childhood: expanding the chILD classification. Histopathology. 2013;63:743–55.
Nathan N, Sileo C, Thouvenin G, et al. Pulmonary fibrosis in children. J Clin Med. 2019;8:1312.
Clement A; ERS Task Force. Task force on chronic interstitial lung disease in immunocompetent children. Eur Respir J. 2004;24:686–97.
Fan LL, Kozinetz CA, Deterding RR, Brugman SM. Evaluation of a diagnostic approach to pediatric interstitial lung disease. Pediatrics. 1998;101:82–5.
Travis WD, Costabel U, Hansell DM, et al. An official American Thoracic Society/European respiratory society statement: update of the international multidisciplinary classification of the idiopathic interstitial pneumonias. Am J Respir Crit Care Med. 2013;188:733–48.
Silbernagel E, Morresi-Hauf A, Reu S, et al. Airway-centered interstitial fibrosis - an under-recognized subtype of diffuse parenchymal lung diseases. Sarcoidosis Vasc Diffuse Lung Dis. 2018;35:218–29.
Churg A, Myers J, Suarez T, et al. Airway-centered interstitial fibrosis: a distinct form of aggressive diffuse lung disease. Am J Surg Pathol. 2004;28:62–8.
Kuranishi LT, Leslie KO, Ferreira RG, et al. Airway-centered interstitial fibrosis: etiology, clinical findings and prognosis. Respir Res. 2015;16:55.
Raghu G, Remy-Jardin M, Ryerson CJ, et al. Diagnosis of hypersensitivity pneumonitis in adults. an official ATS/JRS/ALAT clinical practice guideline. Am J Respir Crit Care Med. 2020;202:e36–69.
Little BP. Sarcoidosis: overview of pulmonary manifestations and imaging. Semin Roentgenol. 2015;50:52–64.
Vrielynck S, Mamou-Mani T, Emond S, Scheinmann P, Brunelle F, de Blic J. Diagnostic value of high-resolution CT in the evaluation of chronic infiltrative lung disease in children. AJR Am J Roentgenol. 2008;191:914–20.
Sileo C, Epaud R, Mahloul M, et al. Sarcoidosis in children: HRCT findings and correlation with pulmonary function tests. Pediatr Pulmonol. 2014;49:1223–33.
Yue CC, Park CH, Kushner I. Apical fibrocavitary lesions of the lung in rheumatoid arthritis. Report of two cases and review of the literature. Am J Med. 1986;81:741–6.
Schulert GS, Yasin S, Carey B, et al. Systemic juvenile Idiopathic arthritis-associated lung disease: characterization and risk factors. Arthritis Rheumatol. 2019;71:1943–54.
Author information
Authors and Affiliations
Contributions
DB, MJ, and PN conceived of the presented idea. MJ verified the analytical methods. ASB encouraged DB to investigate a specific aspect and supervised the findings of this work. All authors discussed the results and contributed to the final manuscript. SKK supervised the project. MJ will act as the guarantor for this paper.
Corresponding author
Ethics declarations
Conflict of Interest
None.
Additional information
Publisher's Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Supplementary Information
Below is the link to the electronic supplementary material.
Rights and permissions
About this article
Cite this article
Bhalla, D., Jana, M., Naranje, P. et al. Fibrosing Interstitial Lung Disease in Children: An HRCT-Based Analysis. Indian J Pediatr 90, 153–159 (2023). https://doi.org/10.1007/s12098-021-04004-z
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s12098-021-04004-z